J Rheum Dis.
2013 Dec;20(6):381-384. 10.4078/jrd.2013.20.6.381.
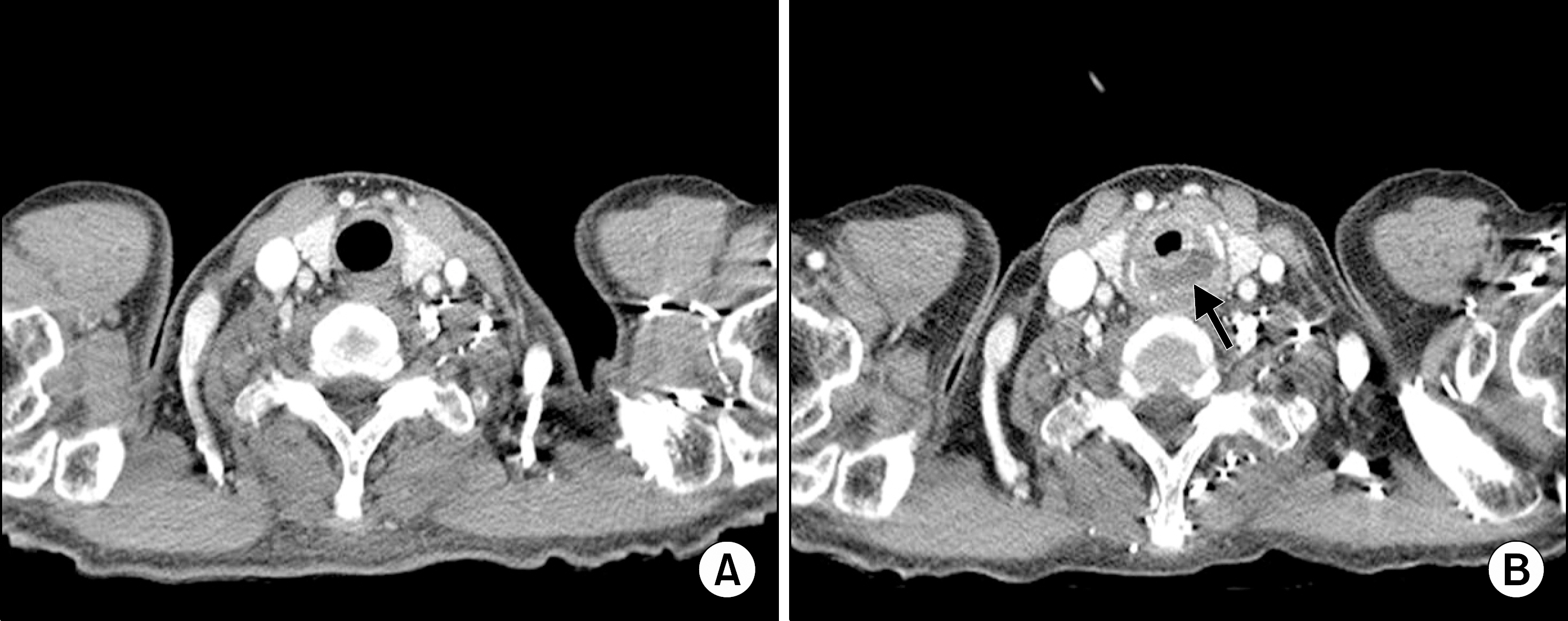
Spontaneous Esophageal Perforation and Hypopharyngeal Abscess in Adult Dermatomyositis: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 2Department of Pathology, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Radiology, Chungbuk National University Hospital, Cheongju, Korea.
- 4Department of Internal Medicine, Incheon Saint Mary's Hospital, The Catholic University of Korea, Incheon, Korea. kykang@catholic.ac.kr
- KMID: 2222999
- DOI: http://doi.org/10.4078/jrd.2013.20.6.381
Abstract
- In patients with dermatomyositis, chronic inflammation of the pharynx and esophagus results in coughing and difficulty in swallowing. These become important clinical symptoms, especially if they contribute to malnutrition or aspiration pneumonia. They can ultimately reduce the quality of life. In rare cases, if the symptoms worsen despite proper treatment, serious complications may arise, a reason to suspect an esophageal perforation or abscess. The authors report a case of dermatomyositis in an adult patient with rare complications of spontaneous esophageal perforation and hypopharyngeal abscess. The patient received non-surgical treatment and was able to resume oral intake of food.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Iking-Konert C, Ostendorf B, Jung G, Becker A, Schneider M. "Bubbles in the brain": an unusual complication of dermatomyositis. Ann Rheum Dis. 2006; 65:550–1.
Article2. Ebert EC. Review article: the gastrointestinal complications of myositis. Aliment Pharmacol Ther. 2010; 31:359–65.
Article3. Williams RB, Grehan MJ, Hersch M, Andre J, Cook IJ. Biomechanics, diagnosis, and treatment outcome in inflammatory myopathy presenting as oropharyngeal dysphagia. Gut. 2003; 52:471–8.
Article4. Oh TH, Brumfield KA, Hoskin TL, Stolp KA, Murray JA, Bassford JR. Dysphagia in inflammatory myopathy: clinical characteristics, treatment strategies, and outcome in 62 patients. Mayo Clin Proc. 2007; 82:441–7.
Article5. Du Y, Dai N, Yu H, Lu Z. Tracheoesophageal fistula: a rare complication of adult dermatomyositis. Eur J Dermatol. 2008; 18:347–8.6. Dougenis D, Papathanasopoulos PG, Paschalis C, Papapet-ropoulos T. Spontaneous esophageal rupture in adult dermatomyositis. Eur J Cardiothorac Surg. 1996; 10:1021–3.
Article7. Ghandour Z, al Karawi MA, Mohamed AE. Spontaneous esophageal perforation: unusual presentation of tuber-culosis. Endoscopy. 1997; 29:143–4.
Article8. Al-Shawwa B, D'Andrea L, Quintero D. Candida esophageal perforation and esophagopleural fistula: a case report. J Med Case Rep. 2008; 2:209.
Article9. Wu JT, Mattox KL, Wall MJ Jr. Esophageal perforations: new perspectives and treatment paradigms. J Trauma. 2007; 63:1173–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypopharyngeal Perforation Associated with Traffic Accident
- A Case of Mediastinal Abscess following Esophageal Perforation
- Iatrogenic esophageal perforation in a newborn: A case report
- Treatment of a Periesophageal Abscess with Endoscopic Ultrasonography-Guided Drainage and Antibiotics: A Case Report
- Boerhaave's Syndrome: Pneumoperitoneum Caused by Spontaneous Rupture of the Anterior Wall of the Esophagus