J Rheum Dis.
2016 Feb;23(1):11-18. 10.4078/jrd.2016.23.1.11.
Recent Trends of Ultrasound in Rheumatology
- Affiliations
-
- 1Department of Rheumatology, Yonsei University Wonju College of Medicine, Wonju, Korea. taeyoung@yonsei.ac.kr
- 2Leeds Institute of Rheumatic and Musculoskeletal Medicine, Chapel Allerton Hospital, University of Leeds, United Kingdom.
- 3NIHR Leeds Musculoskeletal Biomedical Research Unit, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom.
- KMID: 2222795
- DOI: http://doi.org/10.4078/jrd.2016.23.1.11
Abstract
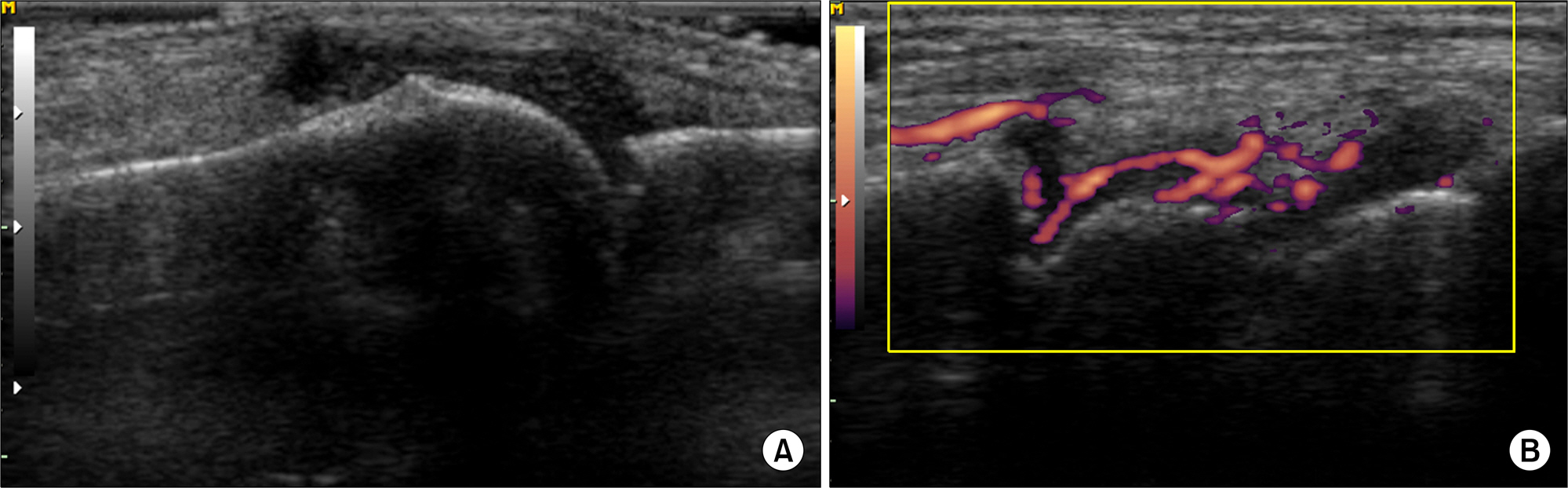
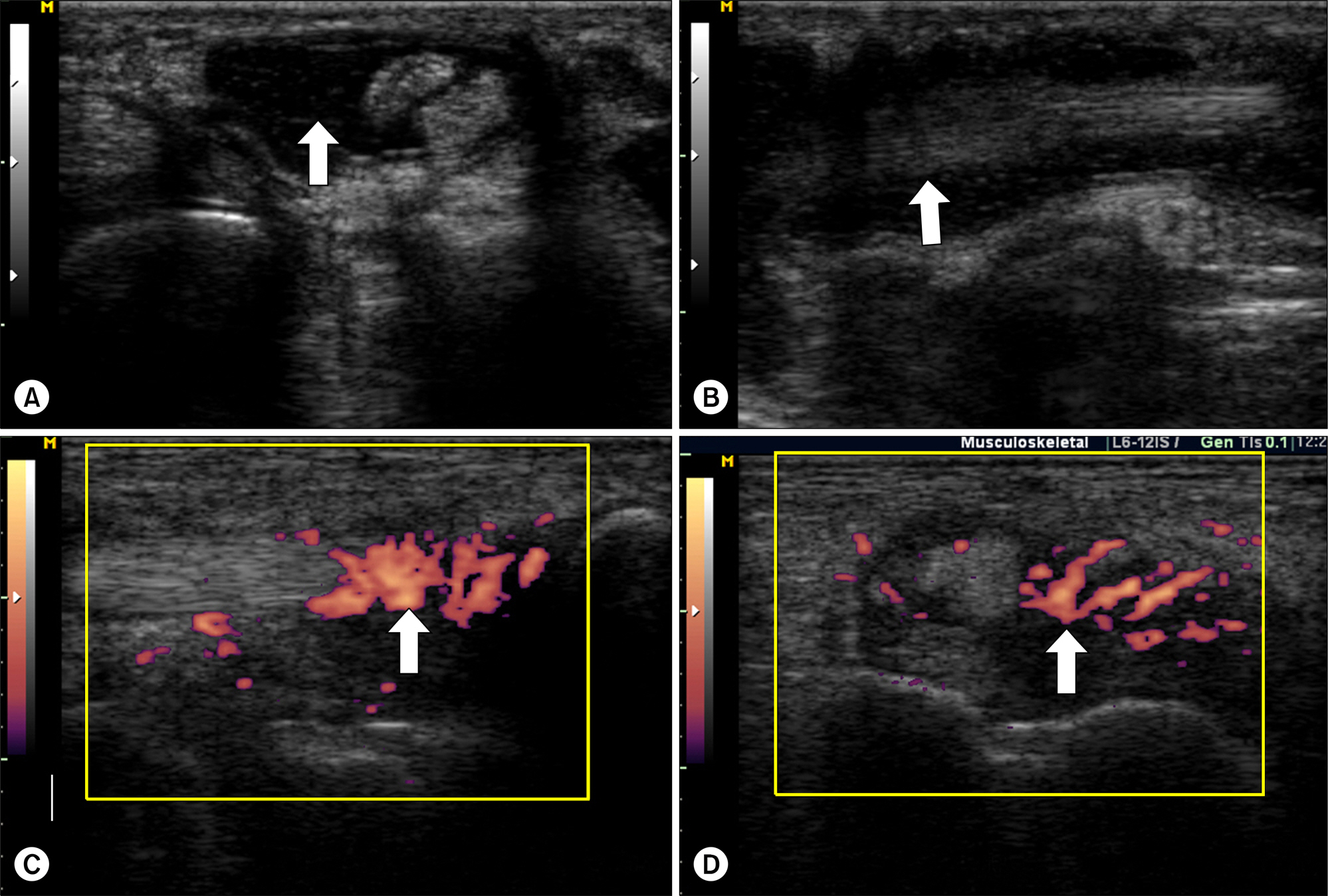
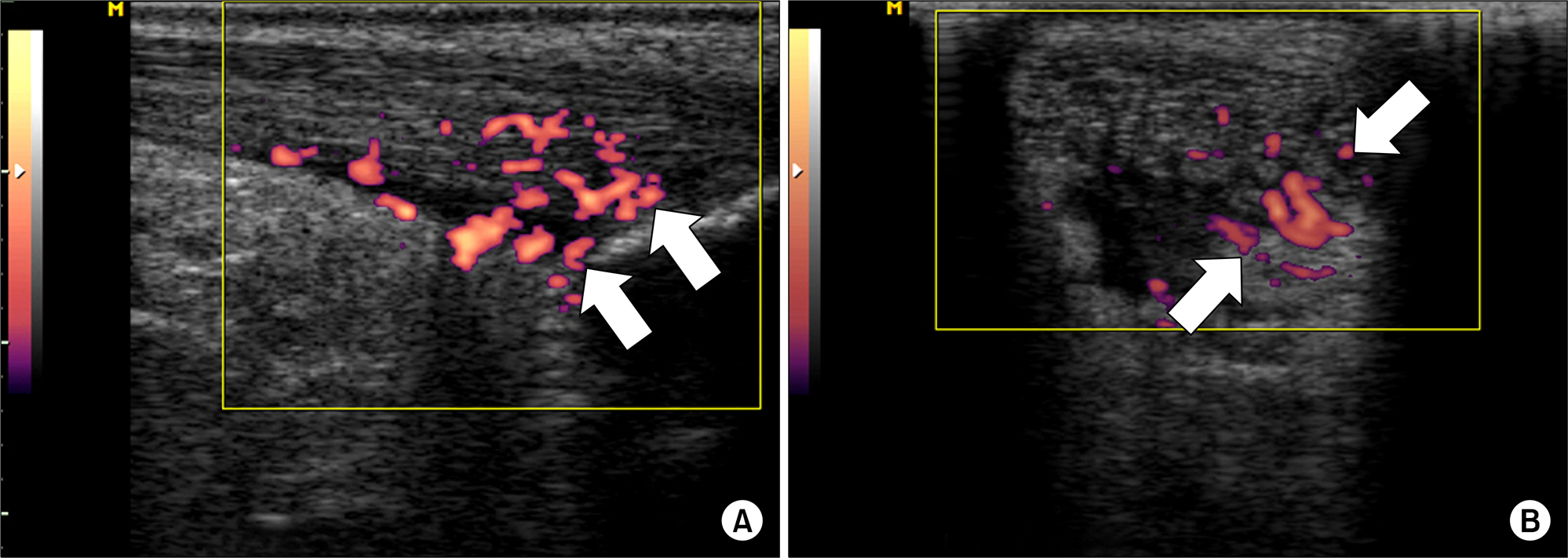
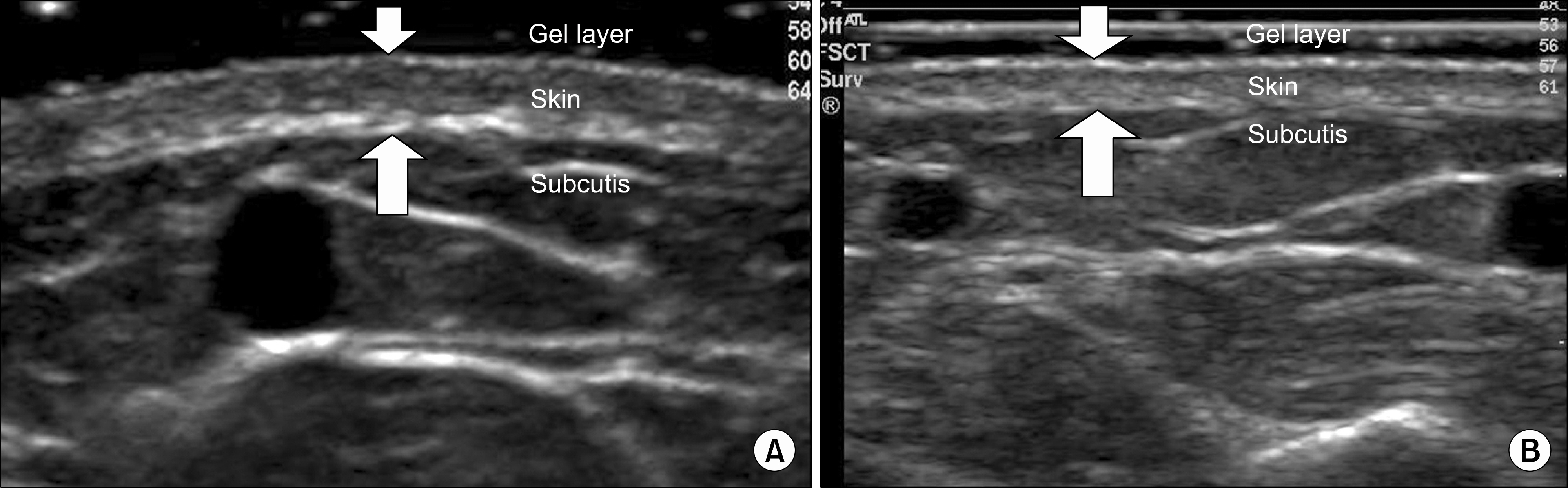
- Owing to the ability of musculoskeletal ultrasound (US) to depict cross sectional images of synovial joint and related structures, US has become the most reliable tool for evaluation of arthritic activity of rheumatoid arthritis (RA). US can detect early synovitis, assess disease activity, and determine true remission in patients with RA. US also can detect early enthesitis in patients with spondyloarthropathies. In addition, US can provide a reliable tool for measuring skin thickness in patients with systemic sclerosis. With guidance of injection or aspiration, US can result in a better clinical outcome. Thus, educational needs and research networks are increasing. We present a review of rheumatology US, focusing on recent trends and advances.
MeSH Terms
Figure
Reference
-
1. Cooperberg PL, Tsang I, Truelove L, Knickerbocker WJ. Gray scale ultrasound in the evaluation of rheumatoid arthritis of the knee. Radiology. 1978; 126:759–63.
Article2. Szkudlarek M, Narvestad E, Klarlund M, Court-Payen M, Thomsen HS, Østergaard M. Ultrasonography of the meta-tarsophalangeal joints in rheumatoid arthritis: comparison with magnetic resonance imaging, conventional radiography, and clinical examination. Arthritis Rheum. 2004; 50:2103–12.
Article3. Karim Z, Wakefield RJ, Quinn M, Conaghan PG, Brown AK, Veale DJ, et al. Validation and reproducibility of ultrasonography in the detection of synovitis in the knee: a comparison with arthroscopy and clinical examination. Arthritis Rheum. 2004; 50:387–94.
Article4. Kane D, Balint PV, Sturrock RD. Ultrasonography is superior to clinical examination in the detection and localization of knee joint effusion in rheumatoid arthritis. J Rheumatol. 2003; 30:966–71.5. Terslev L, Torp-Pedersen S, Qvistgaard E, Bliddal H. Spectral Doppler and resistive index. A promising tool in ultrasonographic evaluation of inflammation in rheumatoid arthritis. Acta Radiol. 2003; 44:645–52.
Article6. Szkudlarek M, Court-Payen M, Jacobsen S, Klarlund M, Thomsen HS, Østergaard M. Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Arthritis Rheum. 2003; 48:955–62.
Article7. Stone M, Bergin D, Whelan B, Maher M, Murray J, McCarthy C. Power Doppler ultrasound assessment of rheumatoid hand synovitis. J Rheumatol. 2001; 28:1979–82.8. Grassi W, Filippucci E, Farina A, Cervini C. Sonographic imaging of tendons. Arthritis Rheum. 2000; 43:969–76.
Article9. Smith TO, Back T, Toms AP, Hing CB. Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol. 2011; 66:1036–48.
Article10. Park GY, Lee SM, Lee MY. Diagnostic value of ultrasonography for clinical medial epicondylitis. Arch Phys Med Rehabil. 2008; 89:738–42.
Article11. Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G, et al. T2T Expert Committee. Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis. 2010; 69:631–7.
Article12. van der Heijde DM, van't Hof MA, van Riel PL, Theunisse LA, Lubberts EW, van Leeuwen MA, et al. Judging disease activity in clinical practice in rheumatoid arthritis: first step in the development of a disease activity score. Ann Rheum Dis. 1990; 49:916–20.
Article13. Prevoo ML, van't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995; 38:44–8.
Article14. Wakefield RJ, D'Agostino MA, Naredo E, Buch MH, Iagnocco A, Terslev L, et al. After treat-to-target: can a targeted ultrasound initiative improve RA outcomes? Ann Rheum Dis. 2012; 71:799–803.15. Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, et al. American College of Rheumatology; European League Against Rheumatism. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum. 2011; 63:573–86.16. Szkudlarek M, Court-Payen M, Strandberg C, Klarlund M, Klausen T, Ostergaard M. Power Doppler ultrasonography for assessment of synovitis in the metacarpophalangeal joints of patients with rheumatoid arthritis: a comparison with dynamic magnetic resonance imaging. Arthritis Rheum. 2001; 44:2018–23.
Article17. Terslev L, Torp-Pedersen S, Savnik A, von der Recke P, Qvistgaard E, Danneskiold-Samsøe B, et al. Doppler ultrasound and magnetic resonance imaging of synovial inflammation of the hand in rheumatoid arthritis: a comparative study. Arthritis Rheum. 2003; 48:2434–41.
Article18. Walther M, Harms H, Krenn V, Radke S, Faehndrich TP, Gohlke F. Correlation of power Doppler sonography with vascularity of the synovial tissue of the knee joint in patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum. 2001; 44:331–8.
Article19. Rowbotham EL, Grainger AJ. Rheumatoid arthritis: ultrasound versus MRI. AJR Am J Roentgenol. 2011; 197:541–6.
Article20. Rubin JM, Bude RO, Carson PL, Bree RL, Adler RS. Power Doppler US: a potentially useful alternative to mean frequency-based color Doppler US. Radiology. 1994; 190:853–6.
Article21. Emery P, Salmon M. Early rheumatoid arthritis: time to aim for remission? Ann Rheum Dis. 1995; 54:944–7.
Article22. Brown AK, Quinn MA, Karim Z, Conaghan PG, Peterfy CG, Hensor E, et al. Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying anti-rheumatic drug-induced clinical remission: evidence from an imaging study may explain structural progression. Arthritis Rheum. 2006; 54:3761–73.
Article23. Peluso G, Michelutti A, Bosello S, Gremese E, Tolusso B, Ferraccioli G. Clinical and ultrasonographic remission determines different chances of relapse in early and long standing rheumatoid arthritis. Ann Rheum Dis. 2011; 70:172–5.
Article24. Saleem B, Brown AK, Keen H, Nizam S, Freeston J, Karim Z, et al. Disease remission state in patients treated with the combination of tumor necrosis factor blockade and methotrexate or with disease-modifying antirheumatic drugs: a clinical and imaging comparative study. Arthritis Rheum. 2009; 60:1915–22.
Article25. Wakefield RJ, Balint PV, Szkudlarek M, Filippucci E, Backhaus M, D'Agostino MA, et al. OMERACT 7 Special Interest Group. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol. 2005; 32:2485–7.26. Lehtinen A, Taavitsainen M, Leirisalo-Repo M. Sonographic analysis of enthesopathy in the lower extremities of patients with spondylarthropathy. Clin Exp Rheumatol. 1994; 12:143–8.27. D'Agostino MA, Said-Nahal R, Hacquard-Bouder C, Brasseur JL, Dougados M, Breban M. Assessment of peripheral enthesitis in the spondylarthropathies by ultrasonography combined with power Doppler: a cross-sectional study. Arthritis Rheum. 2003; 48:523–33.28. Balint PV, Kane D, Wilson H, McInnes IB, Sturrock RD. Ultrasonography of entheseal insertions in the lower limb in spondyloarthropathy. Ann Rheum Dis. 2002; 61:905–10.
Article29. Alcalde M, Acebes JC, Cruz M, González-Hombrado L, Herrero-Beaumont G, Sánchez-Pernaute O. A sonographic enthesitic index of lower limbs is a valuable tool in the assessment of ankylosing spondylitis. Ann Rheum Dis. 2007; 66:1015–9.
Article30. de Miguel E, Cobo T, Muñoz-Fernández S, Naredo E, Usón J, Acebes JC, et al. Validity of enthesis ultrasound assessment in spondyloarthropathy. Ann Rheum Dis. 2009; 68:169–74.
Article31. Gandjbakhch F, Terslev L, Joshua F, Wakefield RJ, Naredo E, D'Agostino MA. OMERACT Ultrasound Task Force. Ultrasound in the evaluation of enthesitis: status and perspectives. Arthritis Res Ther. 2011; 13:R188.
Article32. Eshed I, Hermann KG. Novel imaging modalities in spondyloarthritis. Curr Opin Rheumatol. 2015; 27:333–42.
Article33. Jans L, Jaremko JL, Kaeley GS. Novel imaging modalities in spondyloarthritis. Best Pract Res Clin Rheumatol. 2014; 28:729–45.
Article34. Alexander H, Miller DL. Determining skin thickness with pulsed ultra sound. J Invest Dermatol. 1979; 72:17–9.
Article35. Myers SL, Cohen JS, Sheets PW, Bies JR. B-mode ultrasound evaluation of skin thickness in progressive systemic sclerosis. J Rheumatol. 1986; 13:577–80.36. Moore TL, Lunt M, McManus B, Anderson ME, Herrick AL. Seventeen-point dermal ultrasound scoring system–a reliable measure of skin thickness in patients with systemic sclerosis. Rheumatology (Oxford). 2003; 42:1559–63.
Article37. Akesson A, Hesselstrand R, Scheja A, Wildt M. Longitudinal development of skin involvement and reliability of high frequency ultrasound in systemic sclerosis. Ann Rheum Dis. 2004; 63:791–6.
Article38. Dines KA, Sheets PW, Brink JA, Hanke CW, Condra KA, Clendenon JL, et al. High frequency ultrasonic imaging of skin: experimental results. Ultrason Imaging. 1984; 6:408–34.
Article39. Scheja A, Akesson A. Comparison of high frequency (20 MHz) ultrasound and palpation for the assessment of skin involvement in systemic sclerosis (scleroderma). Clin Exp Rheumatol. 1997; 15:283–8.40. Kaloudi O, Bandinelli F, Filippucci E, Conforti ML, Miniati I, Guiducci S, et al. High frequency ultrasound measurement of digital dermal thickness in systemic sclerosis. Ann Rheum Dis. 2010; 69:1140–3.
Article41. Kang T, Abignano G, Lettieri G, Wakefield RJ, Emery P, del Galdo F. Skin imaging in systemic sclerosis. Eur J Rheumatol. 2014; 1:111–6.
Article42. Ch'ng SS, Roddy J, Keen HI. A systematic review of ultrasonography as an outcome measure of skin involvement in systemic sclerosis. Int J Rheum Dis. 2013; 16:264–72.43. Louis LJ. Musculoskeletal ultrasound intervention: principles and advances. Radiol Clin North Am. 2008; 46:515–33.
Article44. Sibbitt WL Jr, Peisajovich A, Michael AA, Park KS, Sibbitt RR, Band PA, et al. Does sonographic needle guidance affect the clinical outcome of intraarticular injections? J Rheumatol. 2009; 36:1892–902.
Article45. Koski JM. Ultrasound guided injections in rheumatology. J Rheumatol. 2000; 27:2131–8.46. Gilliland CA, Salazar LD, Borchers JR. Ultrasound versus anatomic guidance for intraarticular and periarticular injection: a systematic review. Phys Sportsmed. 2011; 39:121–31.
Article47. Naredo E, Bijlsma JW, Conaghan PG, Acebes C, Balint P, Berner-Hammer H, et al. Recommendations for the content and conduct of European League Against Rheumatism (EULAR) musculoskeletal ultrasound courses. Ann Rheum Dis. 2008; 67:1017–22.
Article48. Bruyn GA, Naredo E, Iagnocco A, Balint PV, Backhaus M, Gandjbakhch F, et al. OMERACT Ultrasound Task Force. The OMERACT ultrasound working group 10 years on: update at OMERACT 12. J Rheumatol. 2015; 42:2172–6.
Article49. Kang T, Wakefield RJ, Emery P. Musculoskeletal ultrasound in rheumatology in Korea: targeted ultrasound initiative survey. Int J Rheum Dis. 2014 Oct 28; [Epub].DOI: DOI: 10.1111/ 1756-185X.12508.
Article