J Korean Ophthalmol Soc.
2014 Oct;55(10):1558-1561. 10.3341/jkos.2014.55.10.1558.
A Case of Corneal Opacity Improved by Treatment of Demodex Blepharitis
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. jck50ey@hanmail.net
- KMID: 2216879
- DOI: http://doi.org/10.3341/jkos.2014.55.10.1558
Abstract
- PURPOSE
To report a case of corneal opacity improved by treatment of demodex blepharitis.
CASE SUMMARY
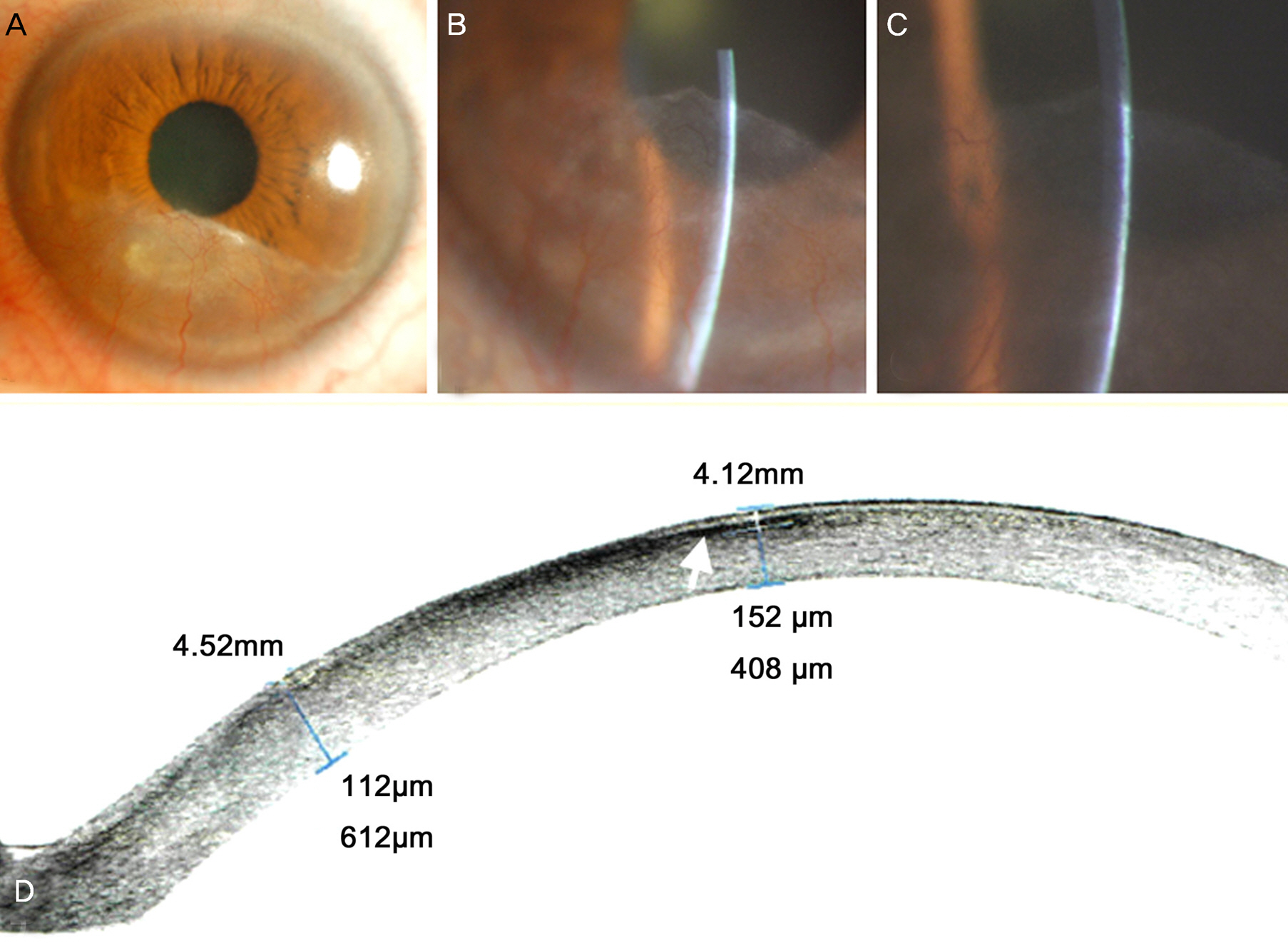
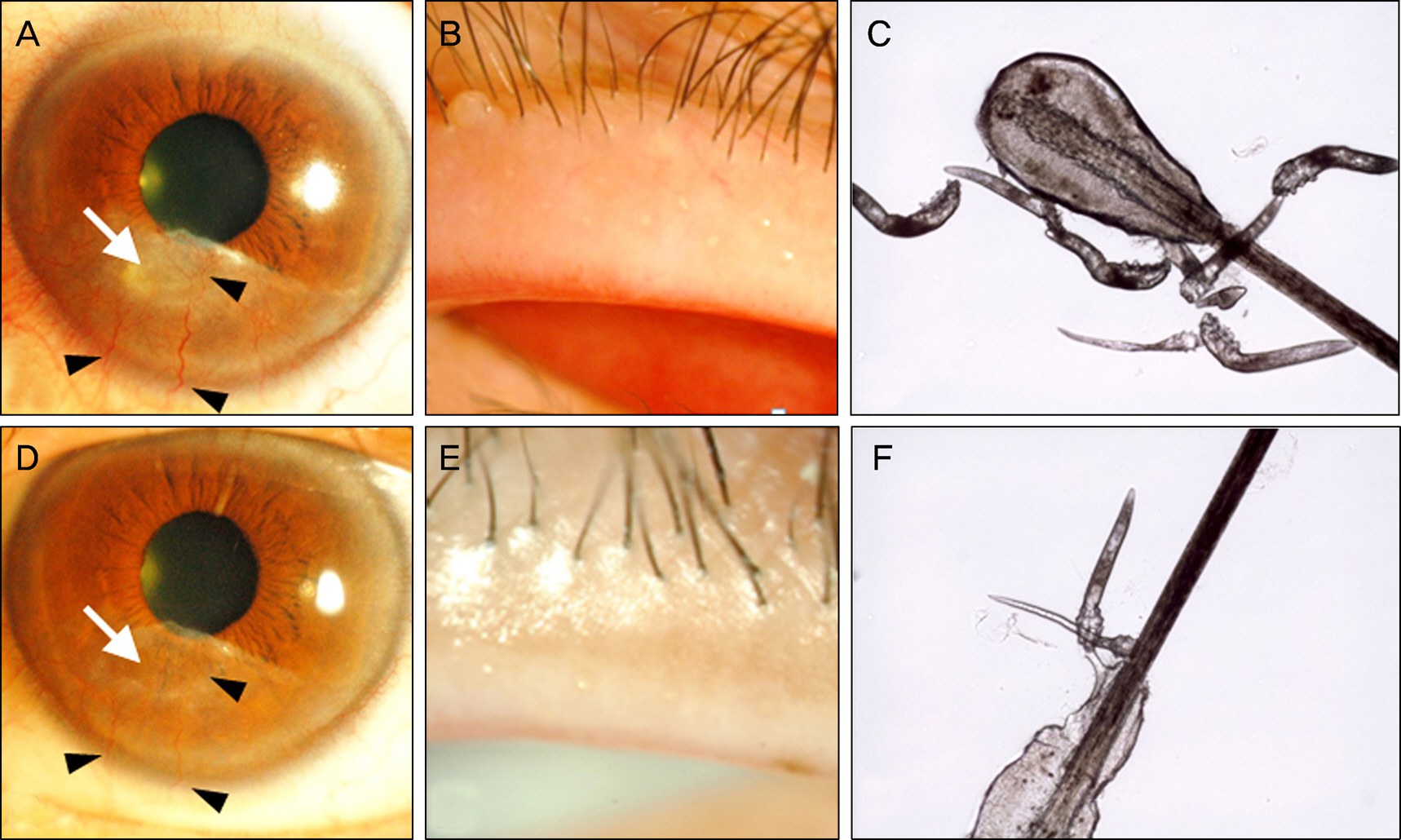
A 50-year-old female who received sub-laser-assisted in situ keratomileusis (LASIK) flap surgery was referred to our clinic with corneal opacity and neovascularization in her left eye. Her visual acuity was 0.5. Telangiectasis of the eyelid margin and meibomian gland dysfunction were observed. Seven Demodex folliculorum were found in 4 eyelashes of the left eye. Lid scrub with 0.4% polyhexamethylene biguanide (PHMB) and ointment containing dexamethasone was started for demodex blepharitis treatment. After 6 months of treatment, the number of Demodex folliculorum was decreased to 2 and the best corrected visual acuity was 0.8. Corneal opacity and neovascularization were also improved.
CONCLUSIONS
The present study showed that demodex blepharitis can induce atypical corneal opacity and neovascularization after LASIK surgery. Evaluation and treatment of demodex blepharitis in these patients is important.
MeSH Terms
Figure
Reference
-
References
1. English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981; 91:362–72.
Article2. Kim JH, Chun YS, Kim JC. Clinical and immunological responses in ocular demodecosis. J Korean Med Sci. 2011; 26:1231–7.
Article3. Gao YY, Di Pascuale MA, Elizondo A, Tseng SC. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007; 26:136–43.
Article4. Koo H, Kim TH, Kim KW, et al. Ocular surface discomfort and demodex: effect of tea tree oil eyelid scrub in demodex blepharitis. J Korean Med Sci. 2012; 27:1574–9.
Article5. Kheirkhah A, Casas V, Li W, et al. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol. 2007; 143:743–9.
Article6. O'Reilly N, Gallagher C, Reddy Katikireddy K, et al. Demodex-associated Bacillus proteins induce an aberrant wound healing response in a corneal epithelial cell line: possible implications for corneal ulcer formation in ocular rosacea. Invest Ophthalmol Vis Sci. 2012; 53:3250–9.7. Hafezi F, Seiler T. Persistent subepithelial haze in thin-flap LASIK. J Refract Surg. 2010; 26:222–5.
Article8. Randleman JB, Shah RD. LASIK interface complications: etiology, management, and outcomes. J Refract Surg. 2012; 28:575–86.
Article9. Fantes FE, Hanna KD, Waring GO 3rd, et al. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990; 108:665–75.
Article10. Norn MS. Incidence of Demodex folliculorum on skin of lids and nose. Acta Ophthalmol (Copenh). 1982; 60:575–83.
Article11. Lee SH, Oh DH, Jung JY, et al. Comparative ocular microbial communities in humans with and without blepharitis. Invest Ophthalmol Vis Sci. 2012; 53:5585–93.
Article12. Moller-Pedersen T, Cavanagh HD, Petroll WM, Jester JV. Stromal wound healing explains refractive instability and haze development after photorefractive keratectomy: a 1-year confocal microscopic study. Ophthalmology. 2000; 107:1235–45.13. Woessner JF Jr. Matrix metalloproteinases and their inhibitors in connective tissue remodeling. FASEB J. 1991; 5:2145–54.
Article14. Strissel KJ, Girard MT, West-Mays JA, et al. Role of serum amyloid A as an intermediate in the IL-1 and PMA-stimulated signaling pathways regulating expression of rabbit fibroblast collagenase. Exp Cell Res. 1997; 237:275–87.
Article15. Strissel KJ, Rinehart WB, Fini ME. Regulation of paracrine cytokine balance controlling collagenase synthesis by corneal cells. Invest Ophthalmol Vis Sci. 1997; 38:546–52.16. Stockinger B, Veldhoen M. Differentiation and function of Th17 T cells. Curr Opin Immunol. 2007; 19:281–6.
Article17. Starnes T, Robertson MJ, Sledge G, et al. Cutting edge: IL-17F, a novel cytokine selectively expressed in activated T cells and monocytes, regulates angiogenesis and endothelial cell cytokine production. J Immunol. 2001; 167:4137–40.
Article18. Numasaki M, Fukushi J, Ono M, et al. Interleukin-17 promotes angiogenesis and tumor growth. Blood. 2003; 101:2620–7.
Article19. Moon JH, Kim JC. Clinical efficacy of polyhexamethylene biguanide lid scrub on demodex blepharitis. J Korean Ophthalmol Soc. 2014; 55:493–7.
Article