J Korean Ophthalmol Soc.
2013 Feb;54(2):375-381. 10.3341/jkos.2013.54.2.375.
Sequential Correction for Large Exotropia: A Case of Iatrogenic Exotropia Developed after Excision of Medial Rectus Muscle During Functional Endoscopic Sinus Surgery (FESS)
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Incheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Incheon, Korea. yimhb@catholic.ac.kr
- KMID: 2216678
- DOI: http://doi.org/10.3341/jkos.2013.54.2.375
Abstract
- PURPOSE
To report a case of iatrogenic exotropia caused by accidental excision of medial rectus muscle during functional endoscopic sinus surgery (FESS), which was successfully corrected by sequential surgical intervention (superior and inferior rectus muscle transposition followed by lateral rectus muscle recession).
CASE SUMMARY
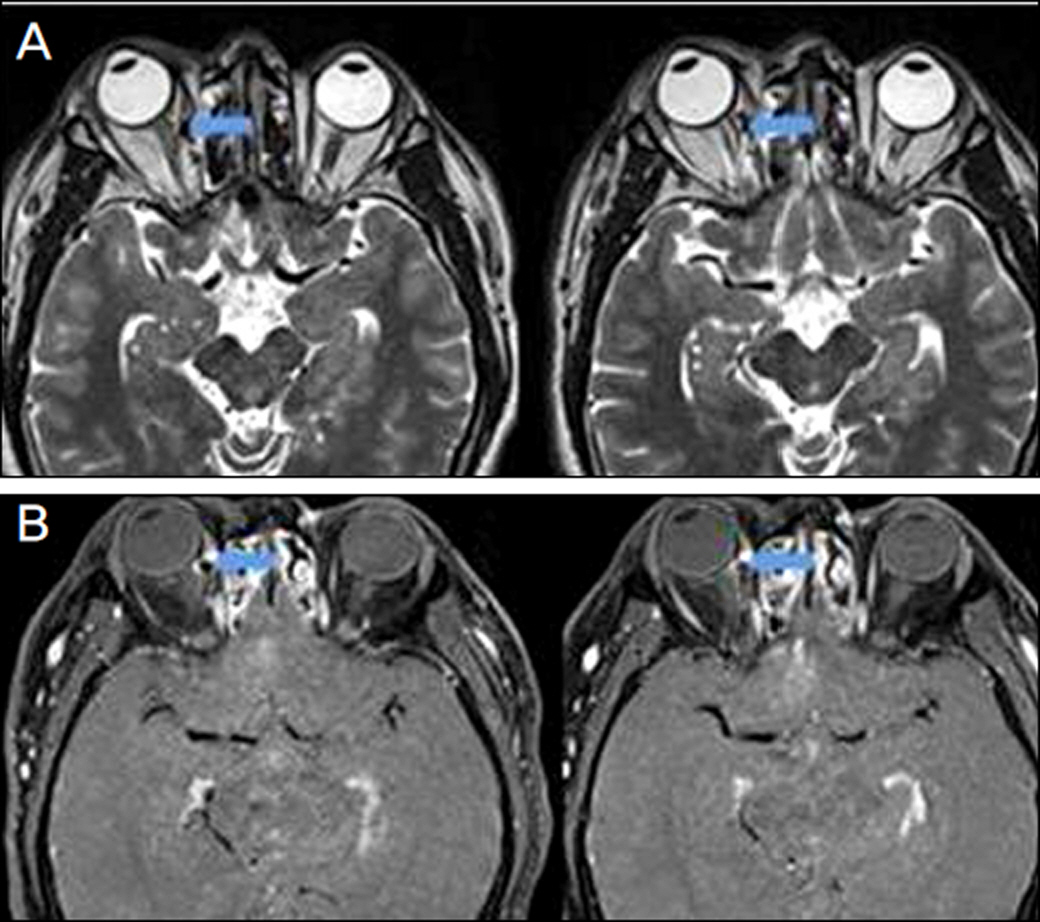
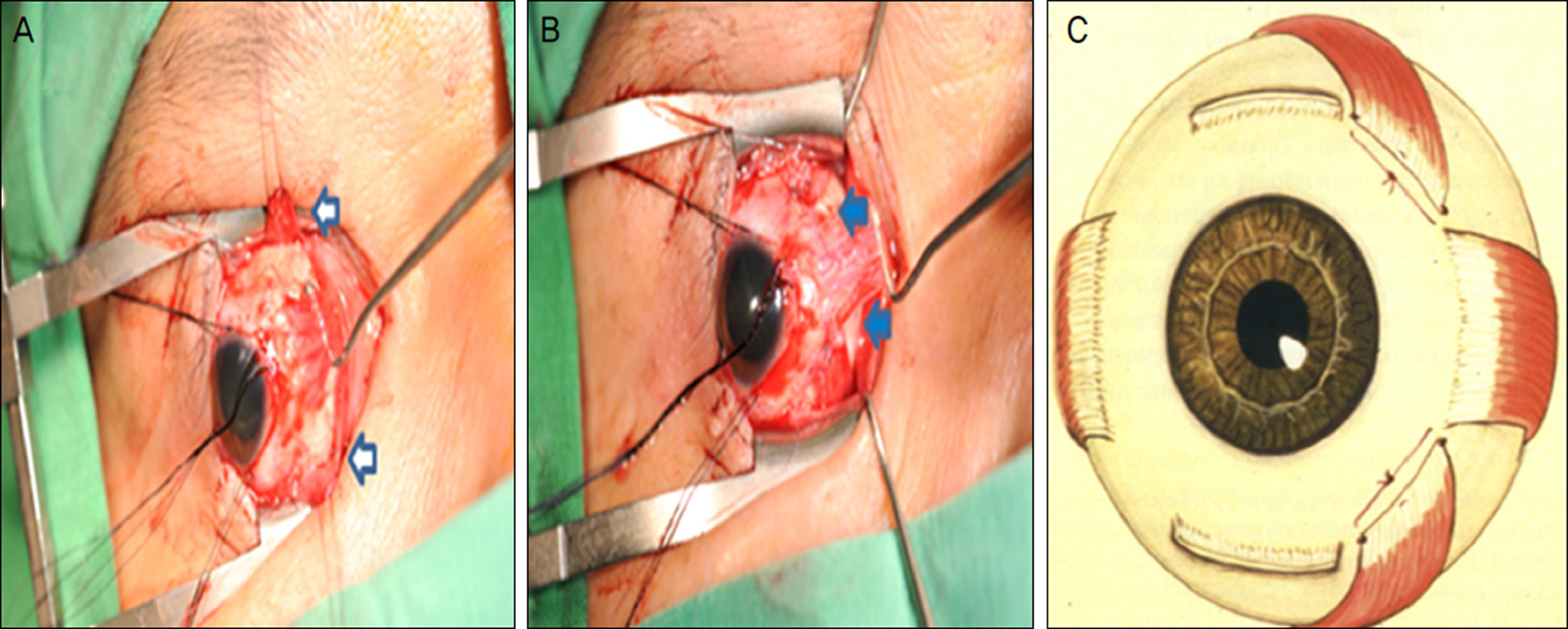
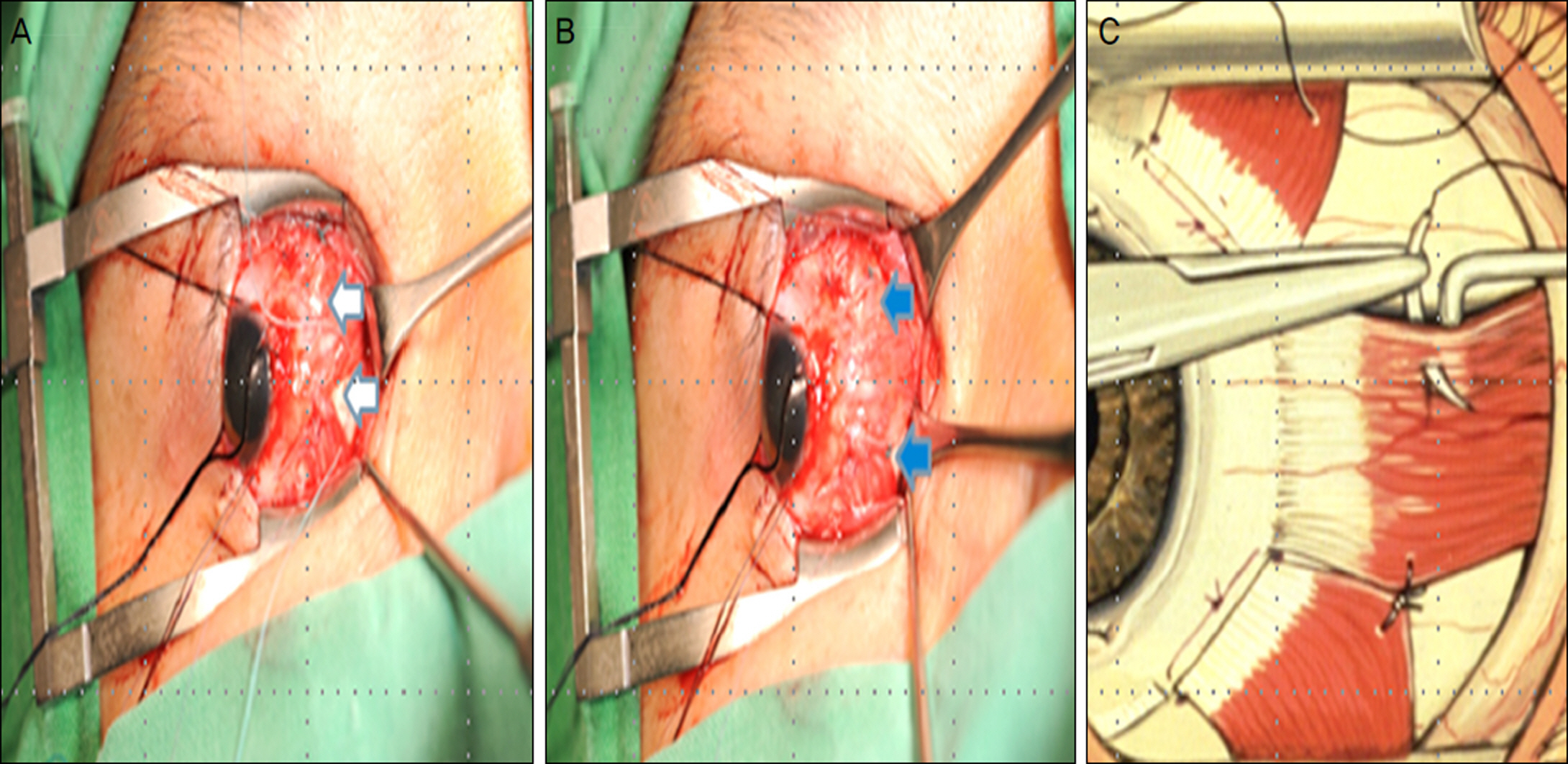
Forty one year old male patient visited our clinic with large exotropia of the right eye developed after functional endoscopic sinus surgery (FESS) which was performed one year ago. At the initial visit in our clinic, there was a large exotropia (95 PD) of the right eye and transection of the medial rectus muscle was observed at the orbital MRI. In order to correct this large iatrogenic exotropia, sequential surgery was planned. Initially, full-tendon transposition of the right superior and inferior rectus muscle was performed which reduced the deviation to 35 PD. Six weeks after the initial surgery, 7 mm right lateral rectus muscle recession was additionally performed, which resulted in exotropia of 10 PD. Diplopia was also improved and the patient was esthetically satisfied with the result.
CONCLUSIONS
Even in a case of iatrogenic exotropia following one year after an accidental excision of medial rectus muscle during intranasal sinus surgery, sequential surgery such as transposition of superior and inferior rectus muscle followed by lateral rectus muscle recession can result in satisfying cosmetic and functional improvement.
Keyword
Figure
Reference
-
References
1. Lessell S. Indirect optic nerve trauma. Arch Ophthalmol. 1989; 107:382–6.
Article2. Bleier BS, Schlosser RJ. Prevention and management of medial rectus injury. Otolaryngol Clin North Am. 2010; 43:801–7.
Article3. Lee MH, Kin SD, Hur YJ. A case of medial rectus muscle injury after functional endoscopic sinus polypectomy and ethmoidectomy. J Korean Ophthalmol Soc. 2002; 43:934–9.4. Kim HC, Kim JH, Lee SY. A case of medial rectus muscle injury and optic nerve transection developed during functional endoscopic sinus surgery. J Korean Ophthalmol Soc. 2003; 44:2705–10.5. Wigand ME. [Transnasal, endoscopical surgery for chronic sinusitis. III. Endonasal ethmoidectomy (author's transl)]. HNO. 1981; 29:287–93.6. Stammberger H, Posawetz W. Functional endoscopic sinus surgery. Concept, indications and results of the Messerklinger technique. Eur Arch Otorhinolaryngol. 1990; 247:63–76.
Article7. Kitthaweesin K, Yospaiboon Y. Dexamethasone and methylprednisolone in treatment of indirect traumatic optic neuropathy. J Med Assoc Thai. 2001; 84:628–34.8. Neuhaus RW. Orbital complications secondary to endoscopic sinus surgery. Ophthalmology. 1990; 97:1512–8.
Article9. Huang CM, Meyer DR, Patrinely JR, et al. Medial rectus muscle injuries associated with functional endoscopic sinus surgery: characterization and management. Ophthal Plast Reconstr Surg. 2003; 19:25–37.10. Thacker NM, Velez FG, Demer JL, et al. Extraocular muscle damage associated with endoscopic sinus surgery: an ophthalmology perspective. Am J Rhinol. 2005; 19:400–5.
Article11. Lee MS, Ahn JH, Kim HY, Lee SY. Clinical study of orbital wall fracture. J Korean Ophthalmol Soc. 1997; 38:1687–93.12. Koornneef L. Current concepts on the management of orbital blowout fractures. Ann Plast Surg. 1982; 9:185–200.
Article13. Hong JE, Goldberg AN, Cockerham KP. Botulinum toxin A therapy for medial rectus injury during endoscopic sinus surgery. Am J Rhinol. 2008; 22:95–7.
Article14. Penne RB, Flanagan JC, Stefanyszyn MA, Nowinski T. Ocular motility disorders secondary to sinus surgery. Ophthal Plast Reconstr Surg. 1993; 9:53–61.
Article15. France TD, Simon JW. Anterior segment ischemia syndrome following muscle surgery: the AAPO&S experience. J Pediatr Ophthalmol Strabismus. 1986; 23:87–91.16. Olver JM, Lee JP. The effects of strabismus surgery on anterior segment circulation. Eye (Lond). 1989; 3(Pt 3):318–26.
Article17. Hong S, Chang YH, Han SH, Lee JB. Effect of full tendon transposition augmented with posterior intermuscular suture for paralytic strabismus. Am J Ophthalmol. 2005; 140:477–83.
Article18. Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997; 1:20–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Medial Rectus Muscle Injury and Optic Nerve Transection Developed During Functional Endoscopic Sinus Surgery
- Medial transposition of the lateral rectus muscle in experimentally induced medial rectus paralysis
- Injury of the Medial Rectus Muscle by Using a Microdebrider During Endoscopic Sinus Surgery : A Case Report
- The Effect of Unilateral Medial Rectus Muscle Resection in Patients with Recurrent Exotropia
- Medial Transposition of the Lateral Rectus Muscle in the Experimentally Induced Medial Rectus Paralysis