J Korean Ophthalmol Soc.
2013 Jan;54(1):85-91. 10.3341/jkos.2013.54.1.85.
Transient Hypotony after Silicone Oil Removal in Rhegmatogenous Retinal Detachment
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University School of Medicine, Daegu, Korea. jps11@hanmail.net
- KMID: 2216454
- DOI: http://doi.org/10.3341/jkos.2013.54.1.85
Abstract
- PURPOSE
To determine the risk factors for transient hypotony after silicone oil removal in rhegmatogenous retinal detachment and to analyze changes in intraocular pressure and visual acuity after silicone oil removal.
METHODS
The medical records of 54 eyes of 52 patients who underwent pars plana vitrectomy, silicone oil tamponade followed by silicone oil removal due to rhegmatogenous retinal detachment, were reviewed.
RESULTS
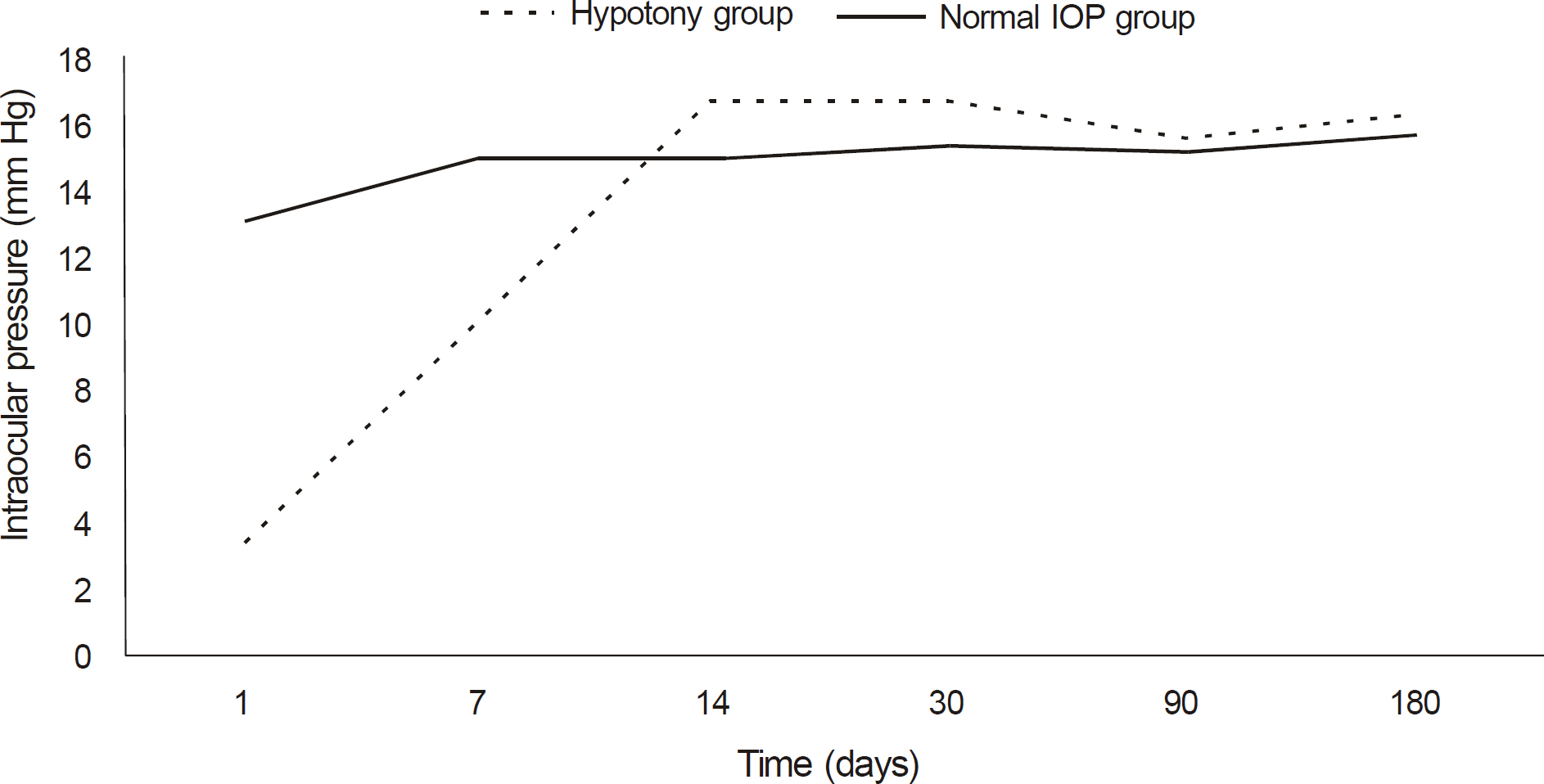
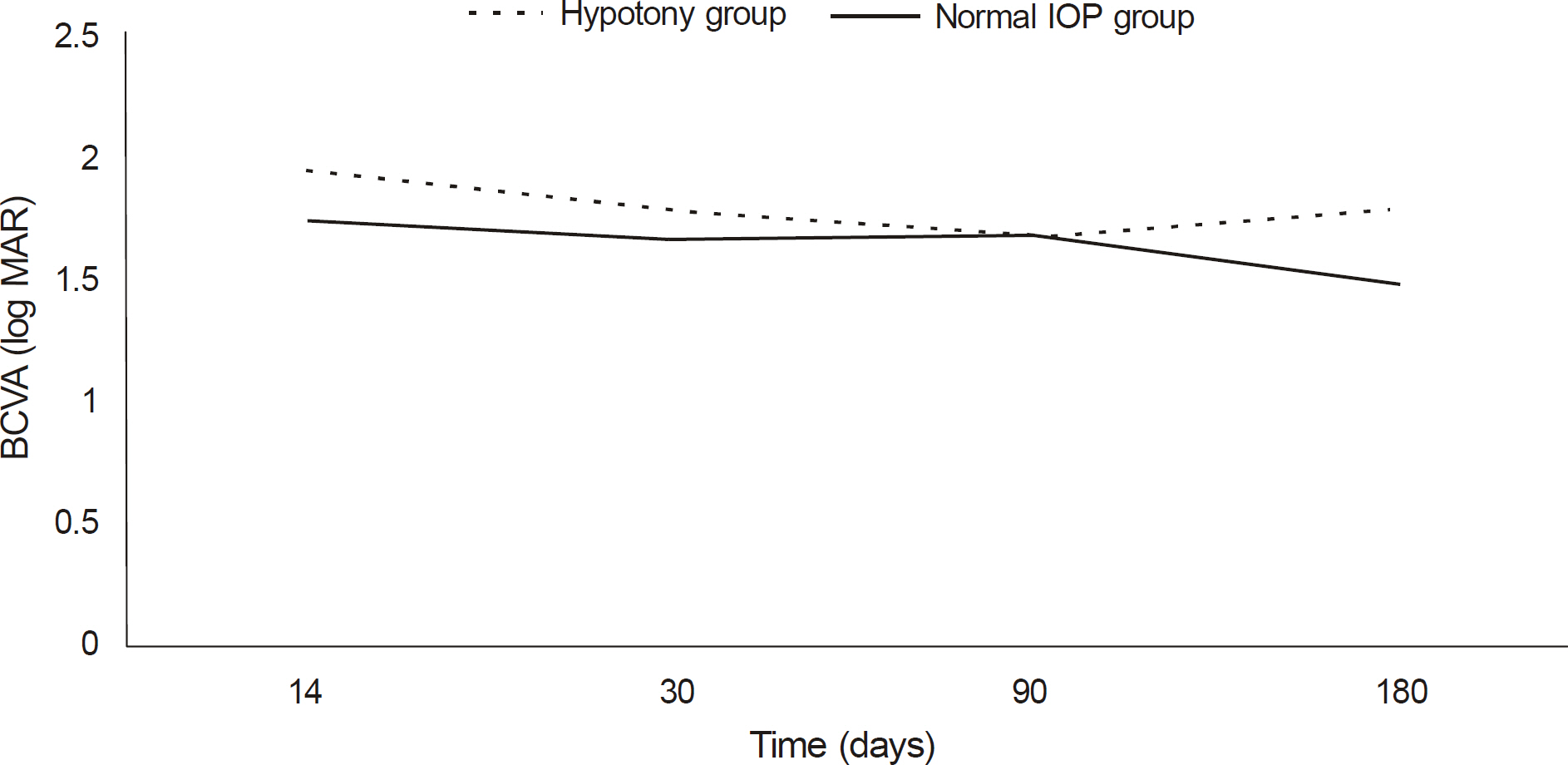
The incidence of transient hypotony after silicone oil removal was 18.5%. Young age (p = 0.011) and axial length (p = 0.002) were risk factors for transient hypotony based on univariate analysis. In multivariate analysis, axial length longer than 26 mm was the only risk factor for transient hypotony (p = 0.005). Seven hypotony patients recovered to normal intraocular pressure spontaneously within 2 weeks. In 2 patients, intraocular pressure was normalized after intravitreal injection of C3F8 gas and 1 patient recovered after a balanced salt solution injection into the anterior chamber. Two weeks after silicone oil removal, there was no significant difference in intraocular pressure between the hypotony group and normal intraocular pressure group. Additionally, there was no statistically significant difference in best corrected visual acuity between the 2 groups after 2 weeks.
CONCLUSIONS
Although transient hypotony after silicone oil removal in rhegmatogenous retinal detachment was frequently observed in the present study, the final best corrected visual acuity and intraocular pressure was not always affected. Ocular hypotony should be examined thoroughly in the early postoperative period.
MeSH Terms
Figure
Reference
-
References
1. Casswell AG, Gregor ZJ. Silicone oil removal. II. Operative and postoperative complications. Br J Ophthalmol. 1987; 71:898–902.
Article2. Hutton WL, Azen SP, Blumenkranz MS, et al. The effects of abdominal oil removal. Silicone Study Report 6. Arch Ophthalmol. 1994; 112:778–85.3. Azen SP, Scott IU, Flynn HW Jr, et al. Silicone oil in the repair of complex retinal detachments. A prospective observational abdominal study. Ophthalmology. 1998; 105:1587–97.4. Abu El-Asrar AM, Al-Bishi SM, Kangave D. Outcome of abdominal silicone oil tamponade in complex rhegmatogenous retinal detachment. Eur J Ophthalmol. 2003; 13:474–81.5. Lesnoni G, Rossi T, Nistri A, Boccassini B. abdominal prognosis after removal of silicone oil. Eur J Ophthalmol. 2000; 10:60–5.6. Jonas JB, Knorr HL, Rank RM, Budde WM. Intraocular pressure and silicone oil endotamponade. J Glaucoma. 2001; 10:102–8.
Article7. Jiang F, Krause M, Ruprecht KW, Hille K. Risk factors for abdominal success and visual outcome in patients undergoing silicone oil removal. Eur J Ophthalmol. 2002; 12:293–8.8. Gonvers M. Temporary silicone oil tamponade in the management of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1985; 100:239–45.
Article9. La Heij EC, Hendrikse F, Kessels AG. Results and complications of temporary silicone oil tamponade in patients with complicated retinal detachments. Retina. 2001; 21:107–14.
Article10. Goezinne F, La Heij EC, Berendschot TT, et al. Risk factors for abdominal and worse visual outcome after silicone oil removal in eyes with complicated retinal detachment. Eur J oOphthalmol. 2007; 17:627–37.11. Kim SW, Oh J, Yang KS, et al. Risk factors for the development of transient hypotony after silicone oil removal. Retina. 2010; 30:1228–36.
Article12. Pearson RV, McLeod D, Gregor ZJ. Removal of silicone oil abdominal diabetic vitrectomy. Br J Ophthalmol. 1993; 77:204–7.13. Scholda C, Egger S, Lakits A, Haddad R. Silicone oil removal: abdominal, risks and complications. Acta Ophthalmol Scand. 1997; 75:695–9.14. Falkner CI, Binder S, Kruger A. Outcome after silicone oil removal. Br J Ophthlamol. 2001; 85:1324–7.
Article15. Schubert HD. Postsurgical hypotony: relationship to fistulization, inflammation, chorioretinal lesions, and the vitreous. Surv Ophthalmol. 1996; 41:97–125.
Article16. Hoganogan MJ, Kimuraimura SJ, Thygesonhygeson P. Signs and symptoms of uveitis. I. Anterior uveitis. Am J Ophthalmol. 1959; 47(5, Part 2):155–70.17. Framme C, Klotz S, Wolf-Schnurrbusch UE, et al. Intraocular abdominal changes following 20G abdominal vitrectomy. Acta Ophthalmol. 2012; 90:744–9. Sep 28. doi:. DOI: 10.1111/j.1755-3768.2011.02251.x.18. Henderer JD, Budenz DL, Flynn HW Jr, et al. Elevated intraocular pressure and hypotony following silicone oil retinal tamponade for complex retinal detachment: incidence and risk factors. Arch Ophthalmol. 1999; 117:189–95.19. Toris CB, Yablonski ME, Wang YL, Camras CB. Aqueous humor dynamics in the aging human eye. Am J Ophthalmol. 1999; 127:407–12.
Article20. McBrien NA, Cornell LM, Gentle A. Structural and ultrastructural changes to the sclera in a mammalian model of high myopia. Invest Ophthalmol Vis Sci. 2001; 42:2179–87.21. Brubaker RF. Flow of aqueous humor in humans [The Friedenwald Lecture]. Invest Ophthalmol Vis Sci. 1991; 32:3145–66.22. Arevalo JF, Garcia RA, Fernandez CF. Anterior segment inflammation and hypotony after posterior segment surgery. Ophthalmol Clin North Am. 2004; 17:527–37.
Article23. Roters S, Engels BF, Szurman P, Krieglstein GK. Typical abdominal biomicroscopyic findings seen in ocular hypotony. Ophthalmologica. 2002; 216:90–5.24. Nehemy MB, Zisman M, Marigo FA, et al. Ultrasound abdominal after vitrectomy in eyes with normal intraocular pressure and in eyes with chronic hypotony. Eur J Ophthalmol. 2008; 18:614–8.25. Chen WL, Yang CM, Chen YF, et al. Ciliary detachment after pars plana vitrectomy: an ultrasound biomicroscopic study. Retina. 2002; 22:53–8.26. Lee GH, Ahn JK, Park YG. Intravitreal triamcinolone reduces the morphologic changes of ciliary body after pars plana vitrectomy for retinal vascular diseases. Am J Ophthalmol. 2008; 145:1037–44.
Article27. Liu JH, Kripke DF, Twa MD, et al. Twenty-four-hour pattern of abdominal pressure in young adults with moderate to severe myopia. Invest Ophthalmol Vis Sci. 2002; 43:2351–5.28. Araie M, Sugiura Y, Minota K, Akazawa K. Effects of the encircling procedure on the aqueous flow rate in retinal detachment eyes: a fluorometric study. Br J Ophthalmol. 1987; 71:510–5.
Article29. Costa VP, Arcieri ES. Hypotony maculopathy. Acta Ophthalmol Scand. 2007; 85:586–97.
Article30. Kim JR, Kim IT. Treatment of hypotony Maculopathy caused by silicone oil removal with gas tamponade. J Korean Ophthalmol Soc. 2010; 51:1028–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors for Recurrent Rhegmatogenous Retinal Detachment after Silicone Oil Removal
- A Clinical Study of Retinal Detachment Following Intraocular Silicone Oil Removal
- Treatment of Hypotony Maculopathy Caused by Silicone Oil Removal With Gas Tamponade
- Complications Associated with Intravitreal Silicone Oil Injection
- Clinical Evaluation of Choroidal Detachment Associated with Rhegmatogenous Retinal Detachment