J Korean Ophthalmol Soc.
2012 Jul;53(7):941-946. 10.3341/jkos.2012.53.7.941.
The Ocular Fatigue of Watching Three-Dimensional (3D) Images
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. crisim@korea.ac.kr
- 2Department of Ophthalmology, Gachon University of Medicine and Science, Incheon, Korea.
- KMID: 2215851
- DOI: http://doi.org/10.3341/jkos.2012.53.7.941
Abstract
- PURPOSE
To compare ocular fatigue, non-ocular symptoms, and ocular surface changes, such as tear break-up time (BUT) and ocular surface temperature, after watching 2-dimensional (2D) and 3-dimensional (3D) images.
METHODS
Fourteen volunteers were enrolled in the present study. Subjects watched 2D as well as 3D images and answered questions regarding ocular fatigue and general symptoms such as headache. Before and after watching images, the spherical equivalent, degree of conjunctival injection, tear BUT, and ocular surface temperature were measured and the amount of change was analyzed. While watching images, subjects answered questions regarding ocular fatigue and the time when they began to feel definitive symptoms.
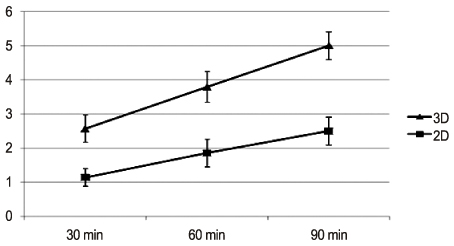
RESULTS
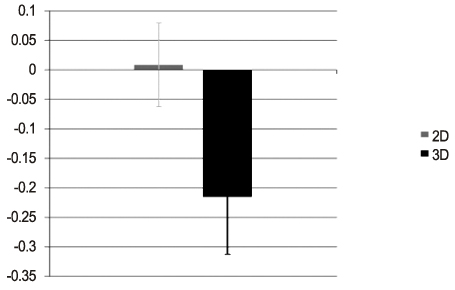
Watching 3D images induced a greater degree of ocular fatigue, headache, and decreasing concentration than watching 2D images (p = 0.038, 0.003, and 0.045, respectively). While watching images, 3D images induced a greater degree of ocular fatigue than 2D images and caused subjects to feel earlier ocular fatigue (3D: 54.86 min, 2D: 78.57 min, p = 0.002). Spherical equivalents became more myopic after watching 3D images.
CONCLUSIONS
After watching 3D images, a greater degree of ocular fatigue, headache, and decreasing concentration was induced and a shorter time to feel definitive ocular fatigue was observed than after watching 2D images. In addition, spherical equivalents changed myopically after watching 3D images.
Figure
Cited by 1 articles
-
Relationship between Ocular Fatigue and Use of a Virtual Reality Device
Sang Hyeok Lee, Martha Kim, Hyosun Kim, Choul Yong Park
J Korean Ophthalmol Soc. 2020;61(2):125-137. doi: 10.3341/jkos.2020.61.2.125.
Reference
-
1. Hoffman DM, Girshick AR, Akeley K, Banks MS. Vergence-accommodation conflicts hinder visual performance and cause visual fatigue. J Vis. 2008. 8:33.1–33.30.2. Ames SL, Wolffsohn JS, McBrien NA. The development of a symptom questionnaire for assessing virtual reality viewing using a head-mounted display. Optom Vis Sci. 2005. 82:168–176.3. Schulze MM, Jones DA, Simpson TL. The development of validated bulbar redness grading scales. Optom Vis Sci. 2007. 84:976–983.4. Lambooij MTM, Ijsselsteinjn WA, Heynderickx I. Woods AJ, Dodgson NA, Merritt JO, editors. Visual discomfort in stereoscopic displays: a review. Stereoscopic Displays and Virtual Reality Systems, Proc SPIE. 2007. v. 6490.5. Suh YW, Kim KH, Kang SY, et al. The objective methods to evaluate ocular fatigue associated with computer work. J Korean Ophthalmol Soc. 2010. 51:1327–1332.6. Ciuffreda KJ, Vasudevan B. Nearwork-induced transient myopia (NITM) and permanent myopia--is there a link? Ophthalmic Physiol Opt. 2008. 28:103–114.7. Goldschmidt E. [On the etiology of myopia. An epidemiological study]. Acta Ophthalmol (Copenh). 1968. Suppl 98. 1+.8. Ong E, Ciuffreda KJ. Nearwork-induced transient myopia: a critical review. Doc Ophthalmol. 1995. 91:57–85.9. Hung GK, Ciuffreda KJ. Incremental retinal-defocus theory of myopia development--schematic analysis and computer simulation. Comput Biol Med. 2007. 37:930–946.10. Iwasaki T, Tawara A, Miyake N. Reduction of asthenopia related to accommodative relaxation by means of far point stimuli. Acta Ophthalmol Scand. 2005. 83:81–88.11. Lambooij M, Fortuin M, IJsselsteijn W, Heynderickx I. Measuring visual fatigue and visual discomfort associated with 3-D displays. J Soc Inf Disp. 2010. 18:931–943.12. Kim SJ, Kim SY. Normal distance stereoacuity by age assessed by the Frisby Davis Distance stereotest. J Korean Ophthalmol Soc. 2008. 49:158–163.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Watching 3-Dimensional Television on Refractive Error in Children
- Influence of Watching 3D Television on Refractive Error in Children with Exodeviation
- Manufacture of the Serially Sectioned Images of the Whole Body (Fifth Report: Methods for Manufacture of the Three Dimensional Images and Virtual Dissection Software)
- The comparison of the lengths and diameters of main bronchi measured from two-dimensional and three-dimensional images in the same patients
- Can Three-Dimensional Reconstructed Image Replace Medical Photograph?