J Korean Ophthalmol Soc.
2015 Aug;56(8):1289-1293. 10.3341/jkos.2015.56.8.1289.
Multiple Evanescent White-Dot Syndrome in a 14-Year-Old Girl
- Affiliations
-
- 1Department of Ophthalmology, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea. 98cys@hanmail.net
- KMID: 2215085
- DOI: http://doi.org/10.3341/jkos.2015.56.8.1289
Abstract
- PURPOSE
To report a case of multiple evanescent white-dot syndrome (MEWDS) in a 14-year-old female.
CASE SUMMARY
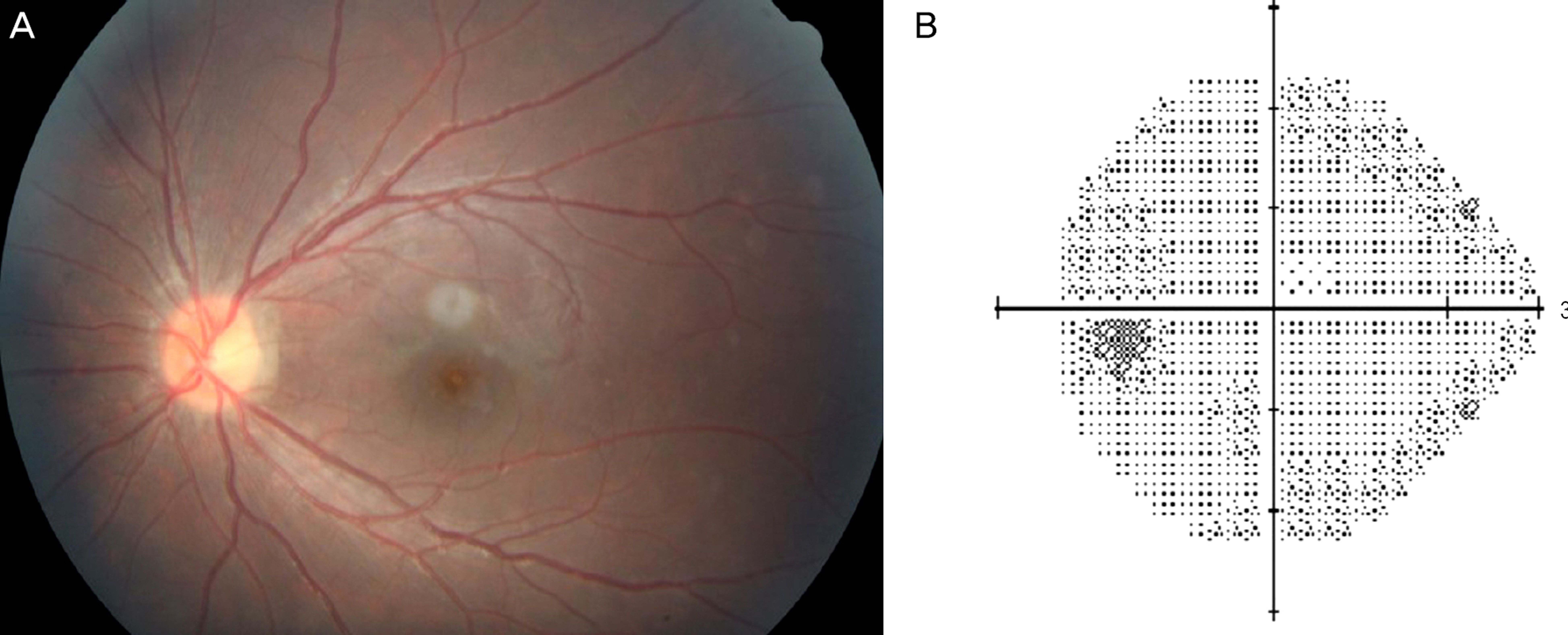
A 14-year-old female presented with decreased visual acuity. Review of systems was unremarkable except for a recent upper respiratory infection prior to her symptoms. On examination, her visual acuity was 20/20 in the right eye and 20/200 in the left eye. Relative afferent pupillary defect was observed. Examination of the left fundus revealed optic disc edema and multiple white dots in the posterior pole. Humphrey visual field test showed enlargement of the blind spot in the left eye. Fluorescein angiography revealed hyperfluorescence and late leakage of the white dots. Indocyanine green angiography showed enlarged late hypofluorescence of the white dots. MEWDS was diagnosed and the patient was followed up with serial examinations. At a follow-up examination 2 weeks later, visual acuity in the left eye improved to 20/70. The majority of white dots on fundus had disappeared and the enlarged scotoma in the left eye recovered to normal size on Humphrey visual field test. At a follow-up examination 3 months later, visual acuity in the left eye improved to 20/30 and residual white dots had further disappeared.
CONCLUSIONS
Cases of MEWDS have been reported in patients as old as 67 years; however, MEWDS is a rare disease and most patients are young females. The authors describe the youngest case to date in Korea of MEWDS in 14-year-old female with typical clinical course.
MeSH Terms
Figure
Reference
-
References
1. Jampol LM, Sieving PA, Pugh D. . Multiple evanescent white dot syndrome. I. Clinical findings. Arch Ophthalmol. 1984; 102:671–4.2. Olitsky SE. Multiple evanescent white-dot syndrome in a 10- year-old child. J Pediatr Ophthalmol Strabismus. 1998; 35:288–9.3. Lim JI, Kokame GT, Douglas JP. Mutiple evanescent white dot syndrome in older patients. Am J Ophthalmol. 1999; 127:725–8.4. Ryan SJ, Schachat AP, Wilkinson CP. . Retina. 5th. Vol. 2. Toronto: Elsevier Saunders;2013. p. 1364–8.5. Buggage RR. White dot syndromes. Focal points: clinical Modules for Ophthalmologist. American Academay of Opthalmology. San Francisco. 2007; Module 4.6. Abu-Yaghi NE, Hartono SP, Hodge DO. . White dot syndromes: 20-year study of incidence, clinical features, and outcomes. Ocul Immunol Inflamm. 2011; 19:426–30.7. McCollum CJ, Kimble JA. Peripapillary subretinal neovascularization associated with multiple evanescent white-dot syndrome. Arch Ophthalmol. 1992; 110:13–4.
Article8. Fine L, Fine A, Cunningham ET Jr. Multiple evanescent white dot syndrome following hepatitis a vaccination. Arch Ophthalmol. 2001; 119:1856–8.9. Baglivo E, Safran AB, Bottuat FX. Multiple evanescent white dot syndrome after hepatitis B vaccine. Am J Ophthalmol. 1996; 122:431–2.
Article10. Gross NE, Yannuzzi LA, Freund KB. . Multiple evanescent white dot syndrome. Arch Ophthalmol. 2006; 124:493–500.
Article11. Ie D, Glaser BM, Murphy . . Indocyanine green angiography in multiple evanescent white-dot syndrome. Am J Ophthalmol. 1994; 117:7–12.
Article12. Nakao K, Isashiki M. Multiple evanescent white dot syndrome. Jpn J Ophthalmol. 1986; 30:376–84.13. Spaide RF, Koizumi H, Freund KB. Photoreceptor outer segment abnormalities as a cause of blind spot enlargement in acute zonal occult outer retinopathy-complex diseases. Am J Ophthalmol. 2008; 146:111–20.
Article14. Hamed LM, Glaser JS, Gass DM, Schatz NJ. Protracted enlarge-ment of the blind spot in multiple evanescent white dot syndrome. Arch Ophthalmol. 1989; 107:194–8.
Article15. Boo SD, Kim SY, Kwon OW. Multiple evanescent white dot syndrome. J Korean Ophthalmol Soc. 1992; 33:925–9.16. Kim WJ, Park SH, Shin HH. Multiple evanescent white dot syndrome. J Korean Ophthalmol Soc. 1994; 35:344–8.17. Nam DH, Huh K. Multiple evanescent white dot syndrome with Ebstein-Barr virus infection. J Korean Ophthalmol Soc. 1998; 39:790–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Evanescent White Dot Syndrome
- Multiple Evanescent White Dot Syndrome with Ebstein-Barr Virus Infection
- Two cases of Multiple Evanescent White Dot Syndrome
- A Case of Subfoveal Choroidal Neovascularization following Multiple Evanescent White-Dot Syndrome
- Atypical Multiple Evanescent White Dot Syndrome with Pigmented Patches of Recovery Phase