J Korean Ophthalmol Soc.
2011 Oct;52(10):1208-1214. 10.3341/jkos.2011.52.10.1208.
The Effect of Positional Change During Laparoscopic Surgery on Intraocular Pressure
- Affiliations
-
- 1Department of Ophthalmology, Wallace Memorial Baptist Hospital, Busan, Korea. kjdeye@naver.com
- 2Department of General Surgery, Wallace Memorial Baptist Hospital, Busan, Korea.
- KMID: 2215004
- DOI: http://doi.org/10.3341/jkos.2011.52.10.1208
Abstract
- PURPOSE
The present study proposes to examine the change of IOP in response to the rise of abdominal pressure and in response to position change during laparoscopic surgery.
METHODS
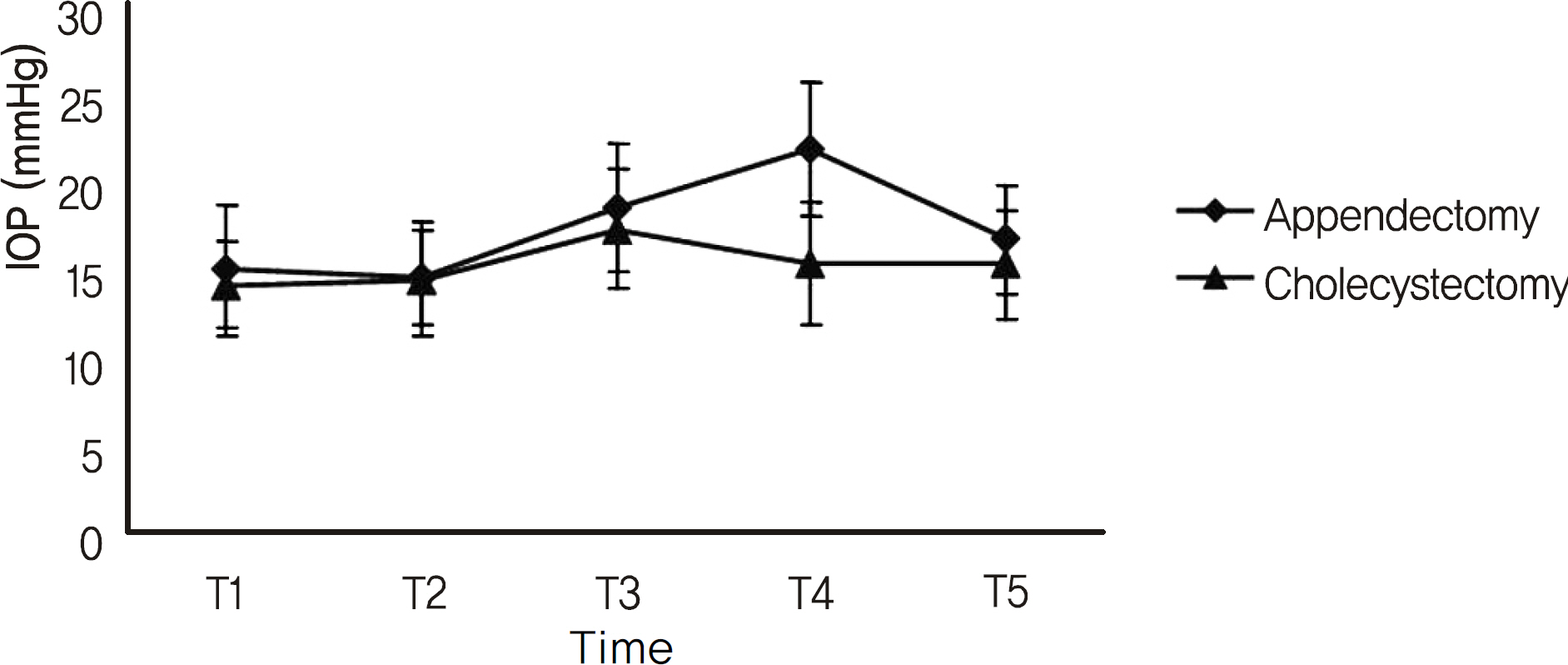
The subjects of the present study included 28 patients who had laparoscopic appendectomy and 20 patients who had laparoscopic cholecystectomy. In both groups, the IOP was measured before surgery, after general anesthesia, after the occurrence of pneumoperitoneum, after position change according to operative method, after the removal of pneumoperitoneum and under general anesthesia.
RESULTS
When comparing the IOP before and after the occurrence of pneumoperitoneum, the IOP after the occurrence increased by 3.70 +/- 0.96 mm Hg in the appendectomy group and by 3.15 +/- 0.5 mm Hg in the cholecystectomy group. After the occurrence of pneumoperitoneum, the IOP measured in the head-low position was 3.25 +/- 0.16 mm Hg higher than measured in the level position in the appendectomy group, and the IOP measured in the head-high position was 2 +/- 0.12 mm Hg lower than measured in the level position in the cholecystectomy group. Between the 2 groups, there was a significant difference of 6.5 mm Hg in IOP according to the change of head position.
CONCLUSIONS
In the present study, the occurrence of pneumoperitoneum in laparoscopic surgery increased IOP, and position change according to operative method also changed IOP. In addition, IOP was significantly different between the 2 groups. In order to prevent the patient from being exposed to high IOP for a long period during laparoscopic surgery, keeping the duration of pneumoperitoneum and a head-low position to a minimum may be helpful.
MeSH Terms
Figure
Reference
-
References
1. Ortega AE, Hunter JG, Peters JH, et al. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg. 1995; 169:208–12.2. Long KH, Bannon MP, Zietlow SP, et al. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: Clinical and economic analyses. Surgery. 2001; 129:390–400.
Article3. Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999; 177:250–6.
Article4. Liu CY. Laparoscopic hysterectomy. a review of 72 cases. J Reprod Med. 1992; 37:351–4.5. Joris JL. Anesthesia for laparoscopic surgery. Anesthesia. 5th ed.Miller RD, editor. Philadelphia: Churchill Livingstone;2000. p. 2003–23.
Article6. Morey TE, Dennis DH. Laparoscopic procedure. Kirby RR, Gravenstein N, Lobato EB, Gravenstein JS, editors. Clinical Anesthesia Practice. 2nd ed.Philadelphia: W.B. Saunders Company;2002. p. 1518–32.7. Lee HJ, Oh TH, Park SG. The effects of intraperitoneal carbon dioxide insufflation and head-down tilt position on intracranial pressure. Korean J Anesth. 1996; 31:140–9.
Article8. Lentschener C, Benhamou D, Niessen F, et al. Intraocular pes-sure changes during gynaecological laparoscopy. Anaesthesia. 1996; 51:1106–8.9. Baskaran M, Raman K, Ramani KK, et al. Intraocular pressure changes and ocular biometry during Sirsasana (headstand posture) in yoga practitioners. Ophthalmology. 2006; 113:1327–32.
Article10. Carlson KH, McLaren JW, Topper JE, Brubaker RF. Effect of body position on intraocular pressure and aqueous flow. Invest Ophthalmol Vis Sci. 1987; 28:1346–52.11. Mader TH, Taylor GR, Hunter N, et al. Intraocular pressure, retinal vascular, and visual acuity changes during 48 hours of 10 degrees head-down tilt. Aviat Space Environ Med. 1990; 61:810–3.12. Frey MA, Mader TH, Bagian JP, et al. Cerebral blood velocity and other cardiovascular responses to 2 days of head-down tilt. J Appl Physiol. 1993; 74:319–25.
Article13. Linder BJ, Trick GL, Wolf ML. Altering body position affects intraocular pressure and visual function. Invest Ophthalmol Vis Sci. 1988; 29:1492–7.14. Christophe C, Marc-Antoine C, Anne P, et al. Changes in intraocular pressure during prolonged (7-day) head-down tilt bedrest. J Glaucoma. 2003; 12:204–8.15. Watenpaugh DE, Hargens AR. The cardiovascular system in microgravity. Fregly MJ, Blatteis CM, editors. Handbook of Physiology: Environmental Physiology. New-York: Oxford;1996. 3:chap.p. 29.
Article16. Smith TJ, Lewis J. Effect of inverted body position intraocular pressure. Am J Ophthalmol. 1985; 99:617–8.17. Friberg TR, Sanborn G, Weinreb RN. Intraocular and episcleral venous pressure increase during inverted posture. Am J Ophthalmol. 1987; 103:523–6.
Article18. Miller RD. Anesthesia. 4th ed.New York: Chruchill Livingstone Inc;1994. p. 2175–9.19. Morgan GE Jr, Mikhail MS. Clinical Anesthesiology. 2nd ed.Stamford: Appleton & Lange;1996. p. 656–7.20. Murphy DF. Anesthesia and intraocular pressure. Anesth Analg. 1985; 64:520–30.
Article21. Gannedahl P, Odeberg S, Brodin LA, Sollevi A. Effects of posture and pneumoperitoneum during naesthesia on the indices of left ventricular filling. Acta Anaesthesiol Scand. 1996; 40:160–6.22. Macri FJ. Interdependence of venous and eye pressure. Arch Ophthalmol. 1961; 65:150–7.
Article23. Lentschener C, Leveque JP, Mazoit JX, Benhamou D. The effect of aberrations on intraocular pressure in rabbits with al-pha-chymotrypsin-induced glaucoma. Anesth Analg. 1998; 86:1283–8.24. Sator S, Wilding E, Schabernig C, et al. Desflurane maintains intraocular pressure at an equivalent level to isoflurane and propofol during unstressed nonophthalmic surgery. Br J Anaesth. 1998; 80:243–4.
Article25. Alexander R, Hill R, Lipham WJ, et al. Remifentanil prevents an increase in intraocular pressure after succinylcholine and tracheal intubation. Br J Anaesth. 1998; 81:606–7.
Article26. Attru AA, Momota Y. Trabecular outflow facility and formation rate of aqueous humor during anesthesia with sevofluranenitrous oxide or sevoflurane-remifentanil in rabbits. Anesth Analg. 1999; 88:781–6.27. Lee JK, Lee JS, Kim YK. The relationship between intraocular pressure and health parameters. J Korean Ophthalmol Soc. 2009; 50:105–12.
Article28. Lee JS, Kim CM, Choi HY, Oum BS. A relationship between intraocular pressure and age and body mass index in a Korean population. J Korean Ophthalmol Soc. 2003; 44:1559–66.29. Carel RS, Korczyn AD, Rock M, Goya I. Association between ocular pressure and certain health parameters. Ophthalmology. 1984; 91:311–4.
Article30. Klein BE, Klein R, Linton KL. Intraocular pressure in an American community. The Beave Dam Eye study. Invest Ophthalmol Vis Sci. 1992; 33:2224–8.31. Bulpitt CJ, Hodes C, Everott MG. Intraocular pressure and systemic blood pressure in the elderly. Br J Ophthalmol. 1975; 59:717–20.
Article32. Shiose Y, Kawase Y. A new approach to stratified normal intraocular pressure in a general population. Am J Ophthalmol. 1986; 101:714–21.
Article33. Son YS, Oh SC, Chung KD, et al. A comparison of the effects of propofol and sevoflurane anesthesias on intraocular pressure during laparoscopic hysterectomy. Korean J Anesth. 2005; 48:10–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraocular Pressure Change used Topical 0.1% Fluorometholone in Children after Strabismus Surgery
- Change in Intraocular Pressure According to Sleeping Posture in Normal People
- The Change of the Intraocular Pressure and Blood Pressure After Exercise
- Position does not affect the optic nerve sheath diameter during laparoscopy
- Positional Change of Intraocular Pressure and Its Relationship to Ocular Pulse Amplitude