J Korean Ophthalmol Soc.
2011 Jun;52(6):647-652. 10.3341/jkos.2011.52.6.647.
Effects of Additional Prednisolone Treatment in Orbital Cellulitis after Bougination
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Dong-A University, Busan, Korea. hbahn@dau.ac.kr
- KMID: 2214634
- DOI: http://doi.org/10.3341/jkos.2011.52.6.647
Abstract
- PURPOSE
To investigate the effects of additional prednisolone treatments in orbital cellulitis after bougination.
METHODS
The medical records of five patients treated for orbital cellulitis after bougination were reviewed. The number of times bouginated, clinical symptoms, biopsy findings, treatment course, recurrence, and prognosis were reviewed.
RESULTS
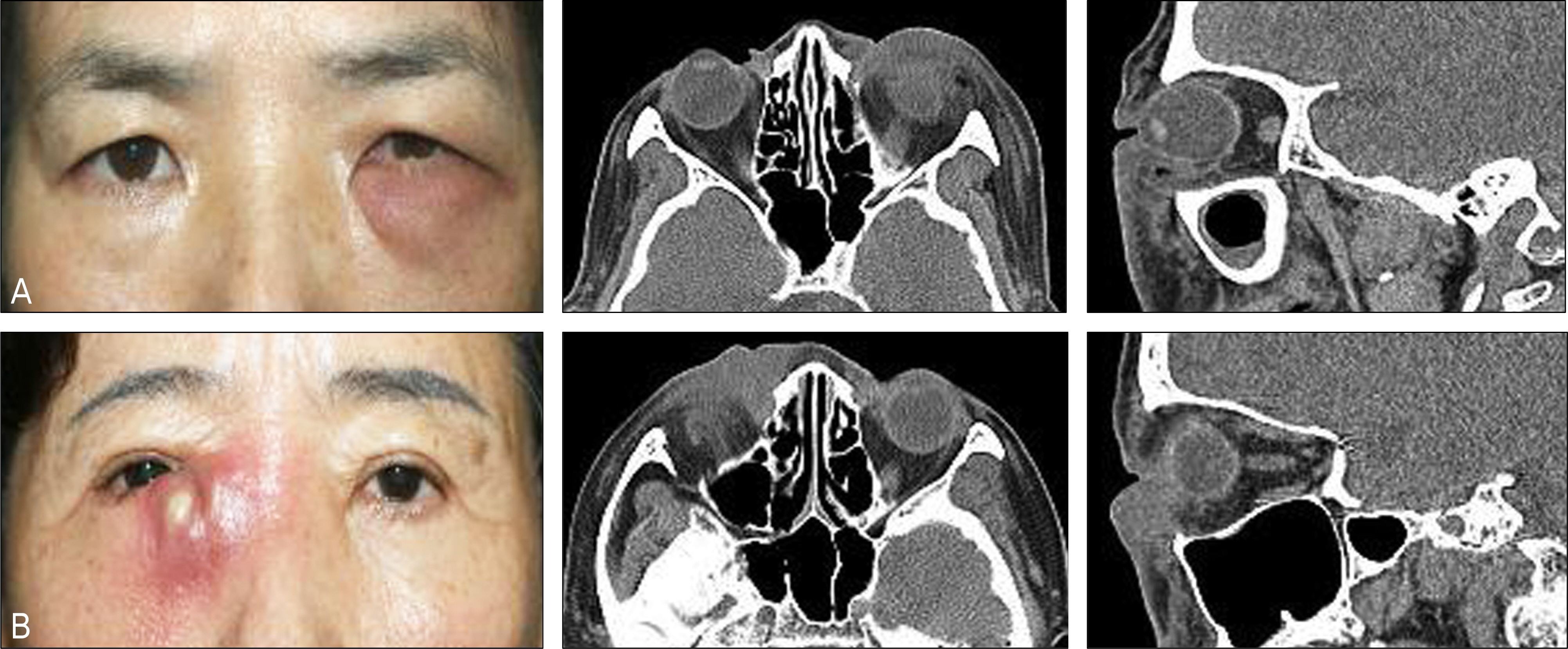
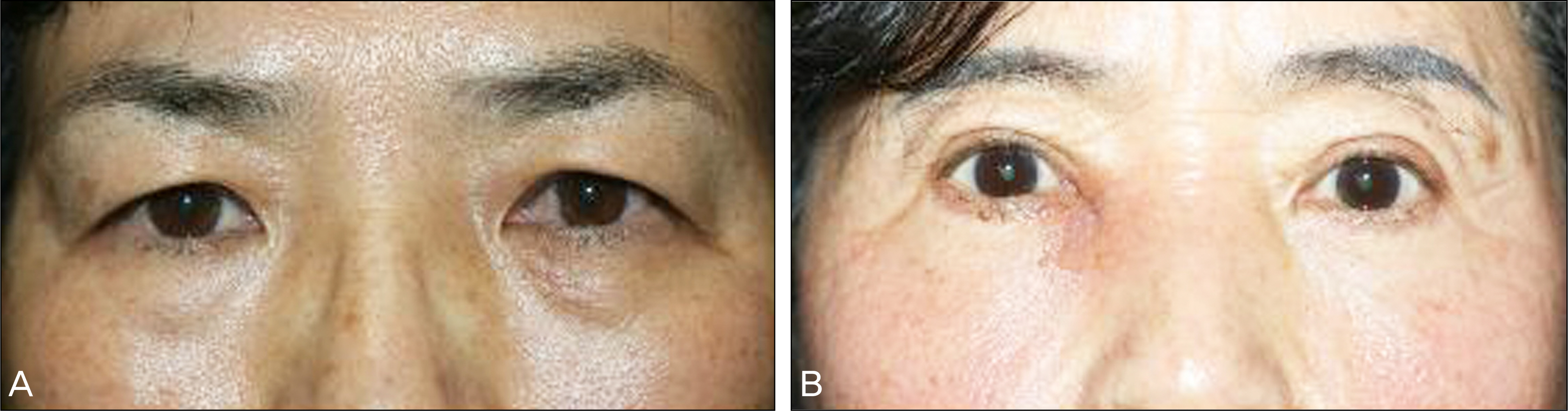
A diffuse, erythematous mass on the lower lid around the medial canthal area was found in all patients. Bougination was performed more than twice in three patients. Chronic inflammation was checked via pathologic tissue biopsy examination in four patients. No patients receiving antibiotic treatments improved, thus additional prednisolone was used and showed satisfactory results, although recurrence was observed in two patients. The recurred two patients improved with repetitive prednisolone treatments.
CONCLUSIONS
Although antibiotics are administered for the treatment of orbital cellulitis after bougination, the use of additional corticosteroids may be beneficial when inflammation is sustained.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Lee KW, Han SH. A case of orbital cellulitis complicated subdural abscess. J Korean Ophthalmol Soc. 1981; 22:475–8.2. Gamble RC. Acute inflammation of the orbit in children. Arch Ophthalmol. 1933; 10:483–97.3. Jarrett WH, Gutman FA. Ocular complication of infection in the paranasal sinuses. Arch Ophthalmol. 1969; 81:683–8.4. Von Noorden GK. Orbital cellulitis following extraocular muscle surgery. Am J Ophthalmol. 1972; 74:627–9.
Article5. Tsai CC, Kau HC, Kao SC, et al. Efficacy of probing the nasolacrimal duct with adjunctive Mitomycin-C for epiphora in adults. Ophthalmology. 2002; 109:172–4.6. Takahashi Y, Kakizaki H, Chan WO, Selva D. Management of congenital nasolacrimal duct obstruction. Acta Ophthalmol. 2010; 88:506–13.
Article7. Cheon HC, Park JM, Lee JH, Ahn HB. Effect of corticosteroids in the treatment of orbital cellulitis with subperiosteal abscess. J Korean Ophthalmol Soc. 2006; 47:2030–4.8. Velasco e Cruz AA, Demarco RC, Valera FC, et al. Orbital complications of acute rhinosinusitis: a new classification. Braz J Otorhinolaryngol. 2007; 73:684–8.9. Brijlal Meena MK, Sharma P. Epidural empyema secondary to orbital cellulitis: a case report. Eur J Ophthalmol. 2007; 17:841–3.10. Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: analysis of outcomes 1988-1998. Ophthalmology. 2000; 107:1454–6.
Article11. Greenberg MF, Pollard ZF. Medical treatment of pediatric subperiosteal orbital abscess secondary to sinusitis. J AAPOS. 1998; 2:351–5.
Article12. Rubin SE, Rubin LG, Zito J, et al. Medical management of orbital subperiosteal abscess in children. J Pediatr Ophthalmol Strabismus. 1989; 26:21–7.13. Moon SW, Lee YJ, Lee YS, Jung JH. A case of simultaneous orbi-tal cellulitis and intracranial complication. J Korean Ophthalmol Soc. 2009; 50:467–70.
Article14. Gehanno P, Beauvillain C, Bobin S, et al. Short therapy with amox-icillin-clavulanate and corticosteroids in acute sinusitis: results of a multicentre study in adults. Scand J Infect Dis. 2000; 32:679–84.15. Yen MT, Yen KG. Effect of corticosteroids in the acute management of pediatric orbital cellulitis with subperiosteal abscess. Ophthal Plast Reconstr Surg. 2005; 21:363–6.
Article16. Escardó JA, Pal B, Feyi-Waboso A, et al. Orbital cellulitis caused by Fusobacterium necrophorum. Am J Ophthalmol. 2001; 131:280–1.
Article17. White AR, Kaye C, Poupard J, et al. Augmentin (amoxicillin/clav-ulanate) in the treatment of community-acquired respiratory tract infection: a review of the continuing development of an innovative antimicrobial agent. J Antimicrob Chemother. 2004; 53(Suppl 1):i3–20.18. Song HJ, Chi MJ. Brain abscess formation accompanied by improve-ment of orbital cellulitis. J Korean Ophthalmol Soc. 2010; 51:131–5.
Article19. Rahbar R, Robson CD, Petersen RA, et al. Management of orbital subperiosteal abscess in children. Arch Otolaryngol Head Neck Surg. 2001; 127:281–6.
Article20. Sajjadian A, Chundru U, Isaacson G. Prospective application of a protocol for selective nonsurgical management of suspected orbital subperiosteal abscesses in children. Ann Otol Rhinol Laryngol. 1999; 108:459–62.
Article21. Young JD, MacEwen CJ. Managing congenital lacrimal obstruction in general practice. BMJ. 1997; 315:293–6.22. McKinley SH, Yen MT, Miller AM, Yen KG. Microbiology of pediatric orbital cellulitis. Am J Ophthalmol. 2007; 144:497–501.
Article23. Lennard CM, Mann EA, Sun LL, et al. Interleukin-1 beta, interleukin-5, interleukin-6, interleukin-8, and tumor necrosis factor-alpha in chronic sinusitis: response to systemic corticosteroids. Am J Rhinol. 2000; 14:367–73.24. Bachert C, Wagenmann M, Rudack C, et al. The role of cytokines in infectious sinusitis and nasal polyposis. Allergy. 1998; 53:2–13.
Article25. Fauci AS, Braunwald E, Kasper DL, et al. Harrison's Principles of Internal Medicine. 17th ed.Vol. 2. New York: McGraw-Hill;2008. p. 2251–2.26. Mombaerts I, Goldschmeding R, Schlingemann RO, Koornneef L. What is orbital pseudotumor? Surv Ophthalmol. 1996; 41:66–78.
Article27. Char DH, Miller T. Orbital pseudotumor. Fine-needle aspiration biopsy and response to therapy. Ophthalmology. 1993; 100:1702–10.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital Cellulitis With Subperisoteal Abscess Secondary to Dental Extraction
- Retinoblastoma Manifested by Hyphema and Orbital Cellulitis
- Successful Treatment of Steroid-Dependent Eosinophilic Cellulitis With Cyclosporine
- A Case ef Orbital Cellulitis Subdural Subdural Abscess
- A Case of Deep Neck Infecton Followed by Orbital Cellulitis