J Korean Ophthalmol Soc.
2015 Sep;56(9):1424-1431. 10.3341/jkos.2015.56.9.1424.
The Effect of Inferior Oblique Muscle Transposition in Primary and Secondary Inferior Oblique Muscle Overaction
- Affiliations
-
- 1Department of Ophthalmology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea. 212010@eulji.ac.kr
- KMID: 2214559
- DOI: http://doi.org/10.3341/jkos.2015.56.9.1424
Abstract
- PURPOSE
To evaluate and compare the effect of transposition of inferior oblique muscle in patients with primary inferior oblique muscle overaction and secondary due to superior oblique muscle palsy.
METHODS
The present study included 41 patients (53 eyes), who appeared to have primary or secondary inferior oblique muscle overaction due to superior oblique muscle palsy and received transposition of inferior oblique muscle with at least 3 months of follow-up. Patients were retrospectively analyzed to compare the effect of correction and its prognosis. Inferior oblique muscle overaction was graded as +1 to +4 according to the severity. Successful surgery was defined as postoperative inferior oblique muscle overaction from 0 to +1 and failure as above +2. Hypertropia in primary gaze was also recorded to evaluate the effect of correction.
RESULTS
Twenty-six (35 eyes) and 15 (18 eyes) patients with primary and secondary inferior oblique muscle overaction due to superior oblique muscle palsy, respectively, received transposition of inferior oblique muscle. Patients with primary inferior oblique muscle overaction showed correction of 2.1 +/- 0.9 with preoperative inferior oblique muscle overaction of 2.0 +/- 0.7. Patients with secondary inferior oblique muscle overaction showed a correction of 2.3 +/- 0.9 with preoperative value of 2.3 +/- 0.8. Each 3.2 +/- 4.1 prism diopters (PD) and 6.5 +/- 5.3 PD of hypertropia at primary gaze showed correction of 3.0 +/- 7.4 PD and 6.3 +/- 5.1 PD, respectively, in each group.
CONCLUSIONS
Primary and secondary inferior oblique muscle overaction due to superior oblique muscle palsy showed no difference in correction of overaction and hypertropia after transposition of inferior oblique muscle. Except for presence of inferior oblique muscle underaction, the correction appears effective with good prognosis.
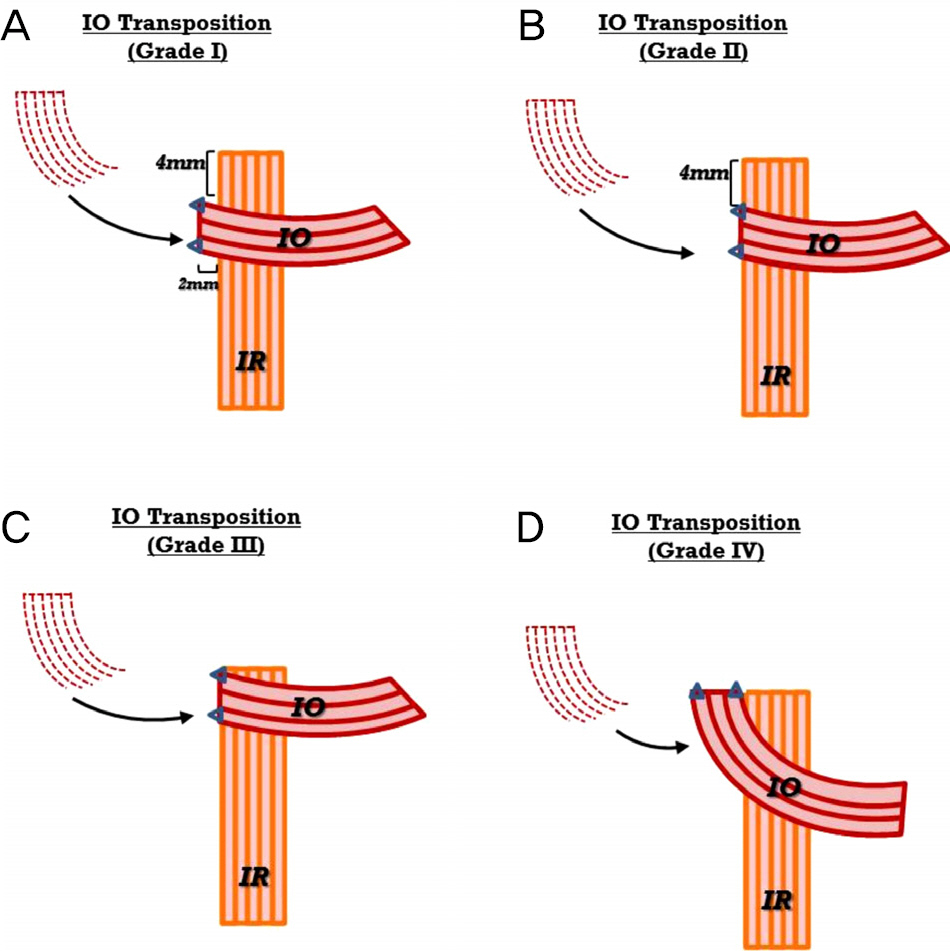
Figure
Reference
-
References
1. Muchnick RS, McCullough DH, Strominger MB. Comparison of anterior transposition and recession of the inferior oblique muscle in unilateral superior oblique paresis. J AAPOS. 1998; 2:340–3.
Article2. Hong JS, Kim MM. Long-term outcome of graded inferior oblique recession. J Korean Ophthalmol Soc. 2006; 47:127–32.3. Choi DK, Choi MY. Clinical manifestations of inferior oblique overaction in patients with horizontal strabismus. J Korean Ophthalmol Soc. 2012; 53:1493–9.
Article4. Paik HJ, Choi JS. Comparison of recession, anterior transposition, and myectomy for inferior oblique overaction. J Korean Ophthalmol Soc. 2006; 47:600–6.5. Song BY, Park SW, Park YG. The surgical effects of inferior obli-que anteriorization. J Korean Ophthalmol Soc. 2004; 45:995–1000.6. Stager DR, Weakley DR Jr, Stager D. Anterior transposition of the inferior oblique. Anatomic assessment of the neurovascular bundle. Arch Ophthalmol. 1992; 110:360–2.7. Guemes A, Wright KW. Effect of graded anterior transposition of the inferior oblique muscle on versions and vertical deviation in primary position. J AAPOS. 1998; 2:201–6.
Article8. Chang YH, Ma KT, Lee JB, Han SH. Anterior transposition of in-ferior oblique muscle for treatment of unilateral superior oblique muscle palsy with inferior oblique muscle overaction. Yonsei Med J. 2004; 45:609–14.
Article9. Farvardin M, Nazarpoor S. Anterior transposition of the inferior oblique muscle for treatment of superior oblique palsy. J Pediatr Ophthalmol Strabismus. 2002; 39:100–4.
Article10. Roh IH, Choi MY. The effect of myectomy on the grading of over-action of the inferior oblique muscle. J Korean Ophthalmol Soc. 2006; 47:437–42.11. Lee KH, Kyung SE. Chang MH. The effect of minimal amount in-ferior oblique recession in superior oblique palsy. J Korean Ophthalmol Soc. 2009; 50:253–9.12. Moon SH, Kim MM. The outcome of graded inferior oblique re-cession in the congenital unilateral superior oblique palsy. J Korean Ophthalmol Soc. 2013; 54:1882–7.
Article13. Min BM, Park JH, Kim SY, Lee SB. Comparison of inferior obli-que muscle weakening by anterior transposition or myectomy: a prospective study of 20 cases. Br J Ophthalmol. 1999; 83:206–8.14. Parvataneni M, Olitsky SE. Unilateral anterior transposition and resection of the inferior oblique muscle for the treatment of hypertropia. J Pediatr Ophthalmol Strabismus. 2005; 42:163–5.
Article15. Ghazawy S, Reddy AR, Kipioti A. . Myectomy versus anterior transposition for inferior oblique overaction. J AAPOS. 2007; 11:601–5.
Article16. Ahn JH, Lee SG. Comparison of inferior oblique myectomy, re-cession, and anterior transposition in unilateral congenital superior oblique palsy. J Korean Ophthalmol Soc. 2010; 51:76–80.
Article17. Mims JL, Wood RC. Antielevation syndrome after bilateral an-terior transposition of the inferior oblique muscles: incidence and prevention. J AAPOS. 1999; 3:333–6.
Article18. Cho YA, Kim JH, Kim S. Antielevation syndrome after unilateral anteriorization of the inferior oblique muscle. Korean J Ophthalmol. 2006; 20:118–23.
Article19. Del Monte MA, Parks MM. Denervation and extirpation of the in-ferior oblique. An improved weakening procedure for marked overaction. Ophthalmology. 1983; 90:1178–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Anteriorization of The Inferior Oblique Muscle in +3 or +4 Inferior Oblique Overaction
- The Effect of Anterior Transposition with J-Deformity for Overaction of the Inferior Oblique Muscle
- The Effect of Modified Anterior Transposition of the Inferior Oblique Muscle for Hypertropia in Superior Oblique Muscle Palsy with Inferior Oblique Muscle Overaction
- Secondary Superior Oblique Overaction after Inferior Oblique Muscle Myectomy in a Patient Misdiagnosed with Inferior Oblique Muscle Overaction
- A Study on the Anatomical Position of the Inferior Oblique Muscle Insertion in Primary Inferior Oblique Overaction