J Korean Ophthalmol Soc.
2011 Mar;52(3):315-324. 10.3341/jkos.2011.52.3.315.
Effects of Digital Ocular Massage in Patients in a Hypertensive Phase after Ahmed Glaucoma Valve Implantation
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. kcs61@cnu.ac.kr
- 2Research Institute for Medical Science, Chungnam National University, Daejeon, Korea.
- KMID: 2214296
- DOI: http://doi.org/10.3341/jkos.2011.52.3.315
Abstract
- PURPOSE
To evaluate the course of the hypertensive phase (HP) after Ahmed glaucoma valve (AGV) implantation and the effects of digital ocular massage.
METHODS
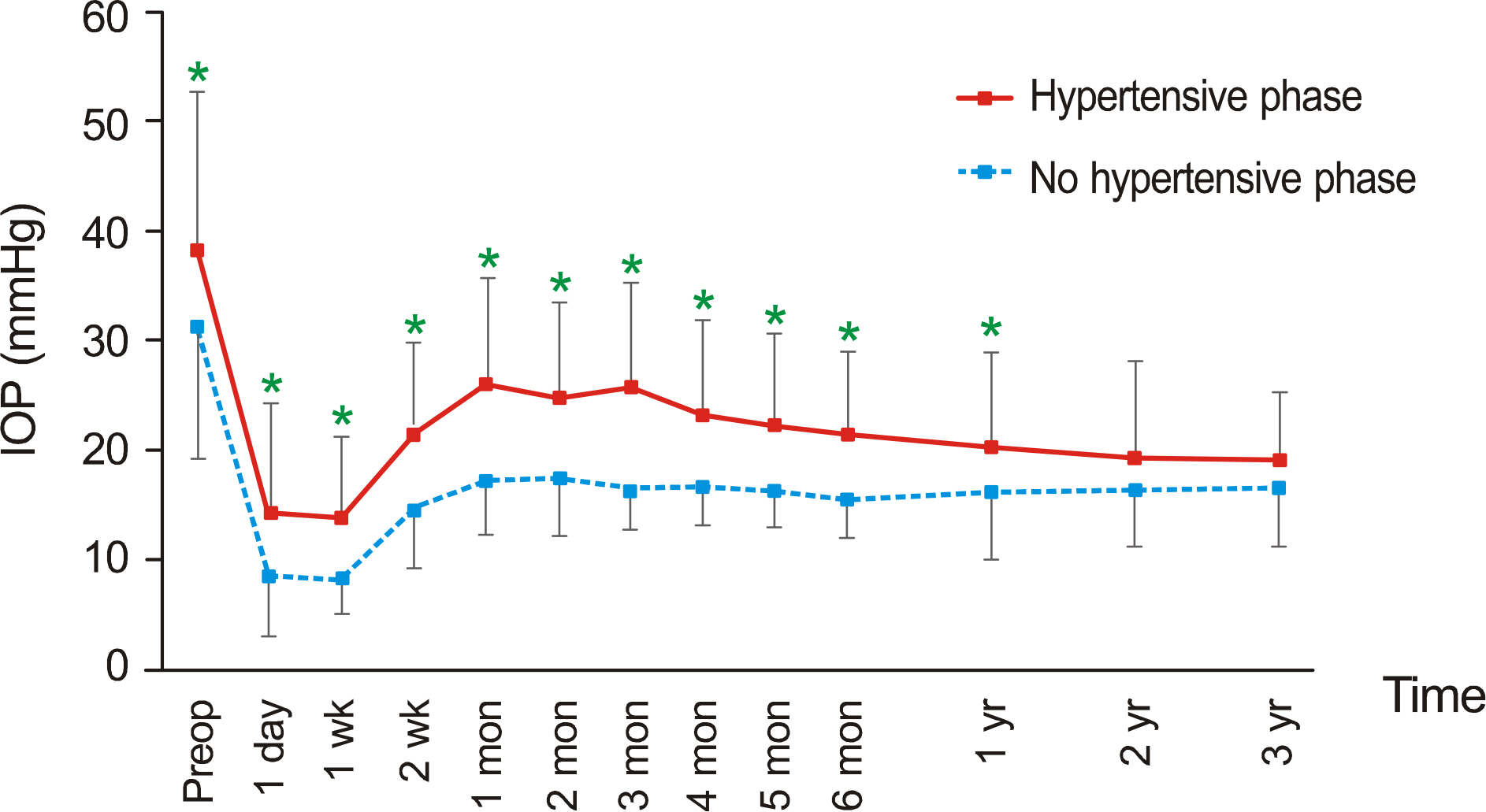
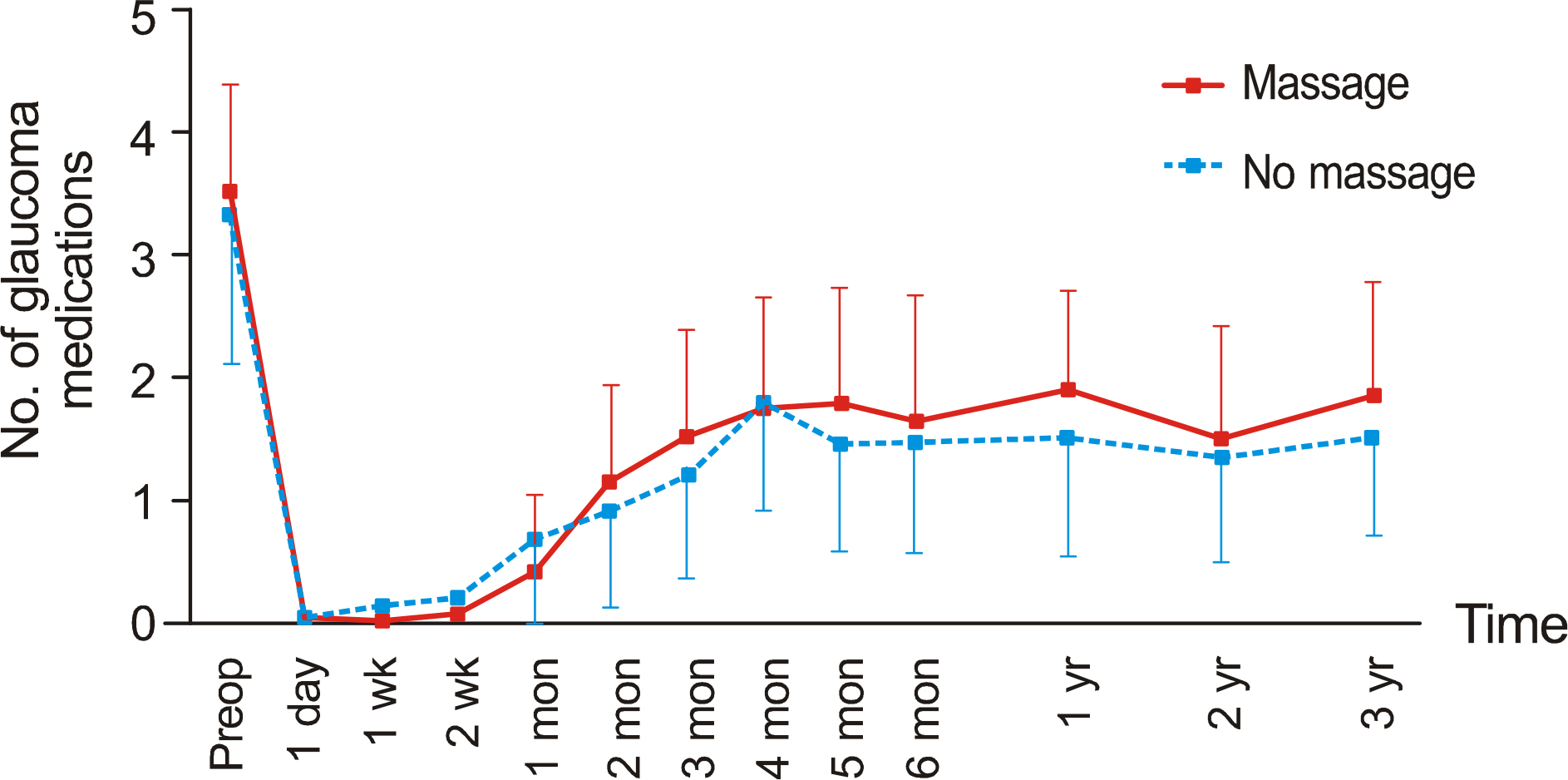
A total of 131 eyes of 131 patients, who underwent AGV implantation surgery, were studied retrospectively. HP was defined as an IOP (intraocular pressure) > or = 22 mm Hg within 6 months after surgery. Various clinical factors related to the occurrence of HP were analyzed. The HP group was compared to the non-HP group. Ocular massage was performed in patients showing acute elevation of IOP at a relatively early postoperative period, and the effects were compared with the non-massage group. The patients who received ocular massage were divided, based on its effects, and compared.
RESULTS
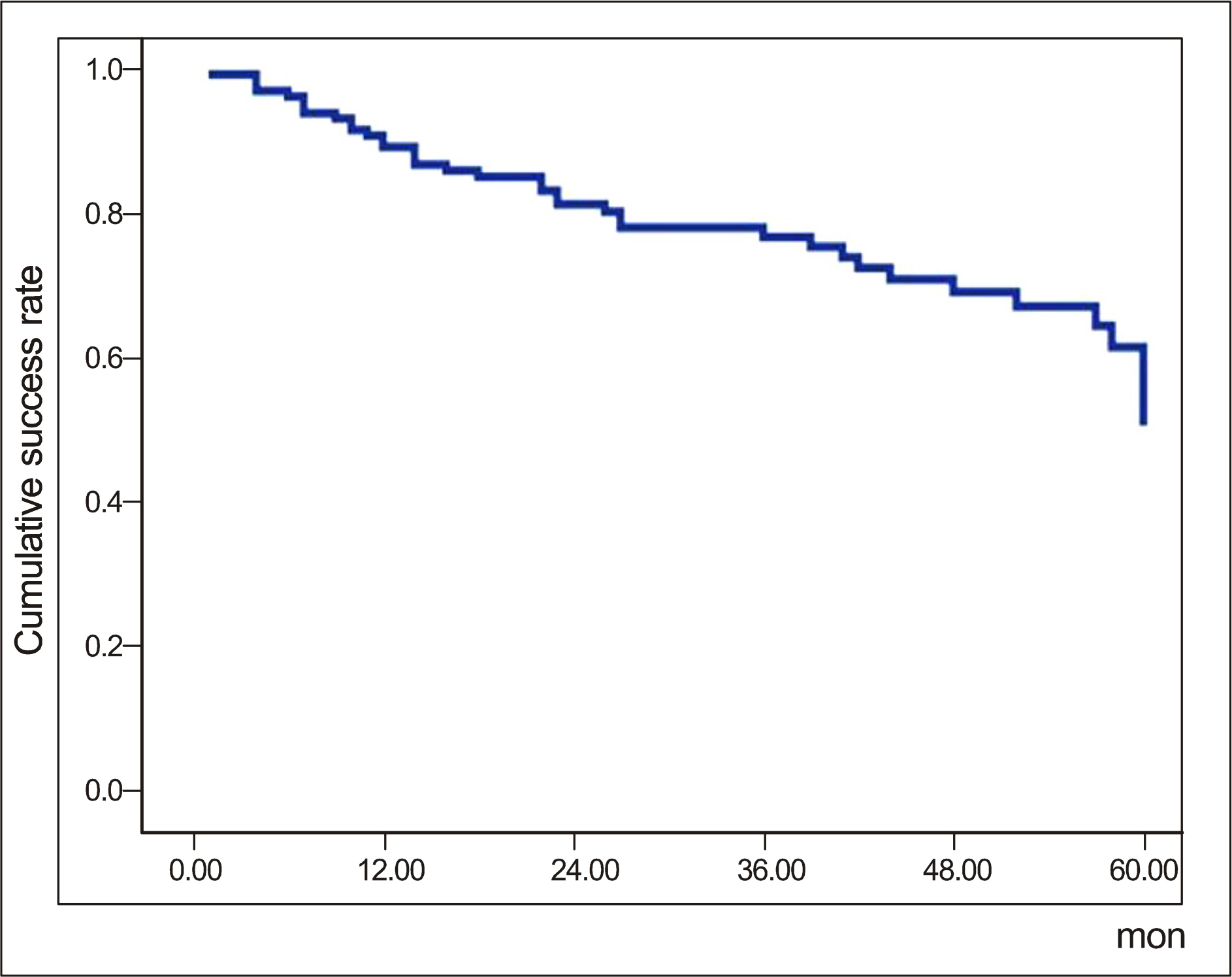
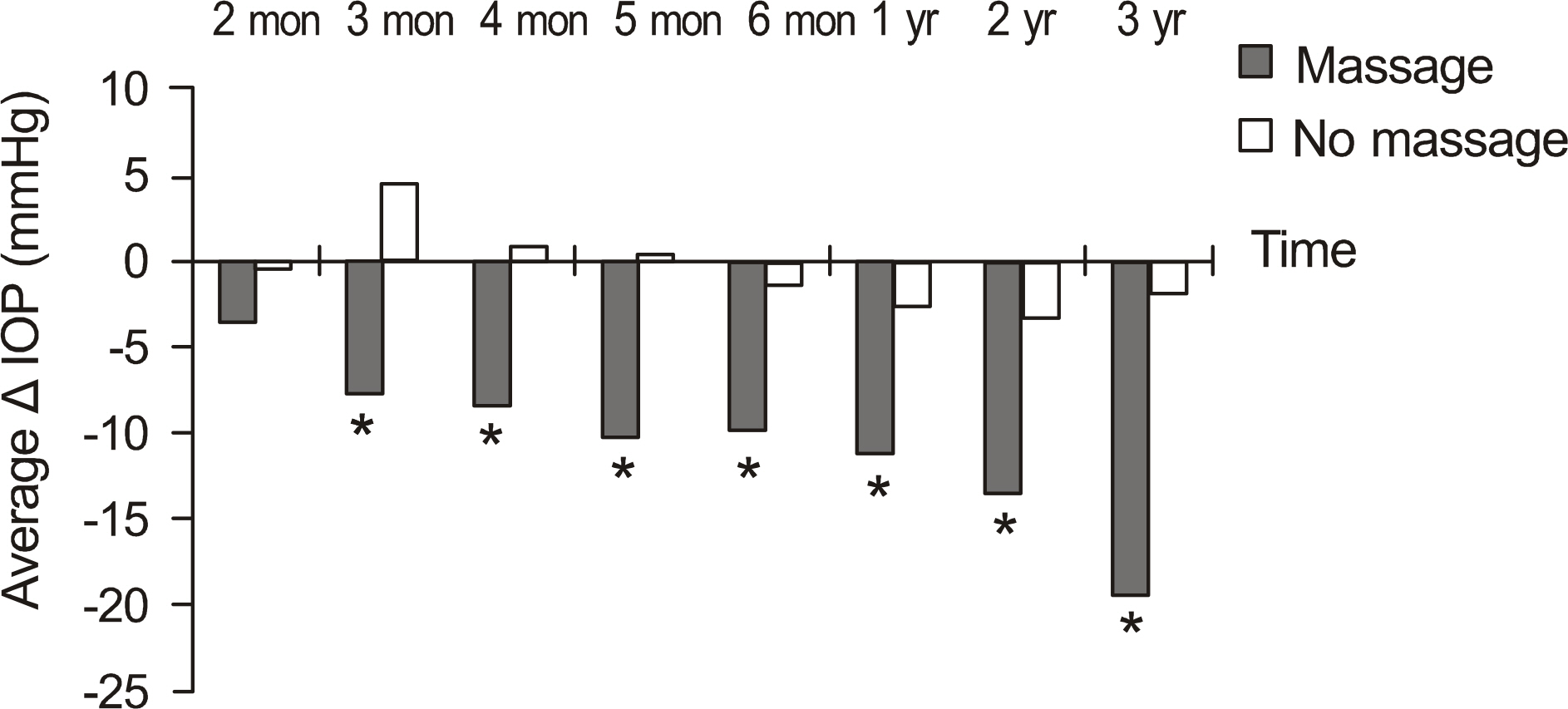
HP developed in 62.6% of the patients after AGV surgery, and the success rate was significantly lower in the HP group. HP occurred more often in males and in patients with high IOP before surgery. HP developed in 82 eyes at 3.3 weeks after surgery in average. Ocular massage was performed in 30 eyes that showed acute IOP increase. The amount of IOP reduction, compared to 1 month after surgery, was greater in massage group than no massage group from 2 months to 3 years after surgery. Successful IOP control by ocular massage was observed in 14 eyes (46.7%), and the success rate was higher in these patients than the patients who showed no significant IOP reduction by ocular massage. But, the difference was not significant (p = 0.072).
CONCLUSIONS
HP is related to the final outcome of surgery. Digital ocular massage can be used as an effective method to control HP and prevent further glaucomatous damage.
Figure
Cited by 1 articles
-
Long-Term Results of Ahmed Valve Implantation in Neovascular Glaucoma and the Effects of Intracameral Bevacizumab
Jong Jin Kim, Jae Pil Shin
J Korean Ophthalmol Soc. 2013;54(5):757-765. doi: 10.3341/jkos.2013.54.5.757.
Reference
-
References
1. Molteno ACB. New implant for drainage in glaucoma: clinical trial. Br J Ophthalmol. 1969; 53:606–15.
Article2. Schocket SS, Lakhanpal V, Richards RD. Anterior chamber tube shunt to an encircling band in the treatment of neovascular glaucoma. Ophthalmology. 1982; 89:1188–94.
Article3. Lloyd MA, Baerveldt G, Heuer DK, et al. Initial clinical experience with the baerveldt implant in complicated glaucomas. Ophthalmology. 1994; 101:640–50.
Article4. Ahn BH, Kim CS, Kim YB. Use of e-PTFE membrane for glaucoma drainage surgery. J Korean Ophthalmol Soc. 1990; 31:603–14.5. Coleman AL, Hill R, Wilson MR, et al. Initial clinical experience with the Ahmed Glaucoma Valve implant. Am J Ophthalmol. 1995; 120:23–31.
Article6. Krupin T, Podos SM, Becker B, Newkirk JB. Valve implants in filtering surgery. Am J Ophthalmol. 1976; 81:232–5.
Article7. Joseph NH, Sherwood MB, Trantas G, et al. A one-piece drainage system for glaucoma surgery. Trans Ophthalmol Soc U K. 1986; 105:657–64.8. White TC. Clinical results of glaucoma surgery using the White glaucoma pump shunt. Ann Ophthalmol. 1992; 24:365–73.9. Prata JA Jr, Mérmoud A, LaBree L, Minckler DS. In vitro and in vivo flow characteristics of glaucoma drainage implants. Ophthalmology. 1995; 102:894–904.
Article10. Molteno TE, Dempster AG. Methods of controlling bleb fibrosis around drainage implants. Mills KB, editor. AHMED GLAUCOMA VALVE 1007 Fourth International Symposium of the Northern Eye Institute. 1st ed.136. Manchester, UK: Pergamon Press;1988. p. 192–211.11. Nouri-Mahdavi K, Caprioli J. Evaluation of the hypertensive phase after insertion of the Ahmed Glaucoma Valve. Am J Ophthalmol. 2003; 136:1001–8.
Article12. Wu SC, Huang SC, Lin KK. Clinical experience with the Ahmed glaucoma valve implant in complicated glaucoma. Chang Gung Med J. 2003; 26:904–10.13. Ayyala RS, Zurakowski D, Smith JA, et al. A clinical study of the Ahmed glaucoma valve implant in advanced glaucoma. Ophthalmology. 1998; 105:1968–76.14. Buys YM, Trope GE. Massage: technique and complications. Trope GE, editor. Glaucoma Surgery. New York, NY: Taylor and Francis;2005. p. 139–44.15. Wieland M, Spaeth GL. Use of digital compression following glaucoma surgery. Ophthalmic Surg. 1988; 19:350–2.
Article16. Lerner SF, Parrish RK. Early postoperative trabeculectomy management: days 2-21. Lerner SF, Parrish RK, editors. Glaucoma Surgery. Philadelphia: Lippincortt Williams and Wilkins;2003. p. 63–75.17. Morgan KS, Black B, Ellis FD, Helveston EM. Treatment of congenital glaucoma. Am J Ophthalmol. 1981; 92:799–803.
Article18. deLuise VP, Anderson DR. Primary infantile glaucoma (congenital glaucoma). Surv Ophthalmol. 1983; 28:1–19.
Article19. Lee YW, Yim JH, Lee SB, Kim CS. The factors associated with the success of Ahmed glaucoma valve implantation. J Korean Ophthalmol Soc. 2005; 46:1509–17.20. Englert JA, Freedman SF, Cox TA. The Ahmed valve in refractory pediatric glaucoma. Am J Ophthalmol. 1999; 127:34–42.
Article21. Huang MC, Netland PA, Coleman AL, et al. Intermediate-term clinical experience with the Ahmed Glaucoma Valve implant. Am J Ophthalmol. 1999; 127:27–33.22. Fellenbaum PS, Almeida AR, Minckler DS, et al. Krupin disk implantation for complicated glaucomas. Ophthalmology. 1994; 101:1178–82.
Article23. Lieberman MF, Ewing RH. Drainage implant surgery for refractory glaucoma. Int Ophthalmol Clin. 1990; 30:198–208.
Article24. Ayyala RS, Zurakowski D, Monshizadeh R, et al. Comparison of double-plate Molteno and Ahmed glaucoma valve in patients with advanced uncontrolled glaucoma. Ophthalmic Surg Lasers. 2002; 33:94–101.
Article25. McIlraith I, Buys Y, Campbell RJ, Trope GE. Ocular massage for intraocular pressure control after Ahmed valve insertion. Can J Ophthalmol. 2008; 43:48–52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Needle Revision and Digital Ocular Massage for Treatment of Ocular Hypertension Phase after Ahmed Valve Implantation
- The Short Term Effect of Ocular Digital Massage and its Echographic Evaluation Following Ahmed Glaucoma Valve Implantation
- Effects of Early Postoperative Intraocular Pressure after Ahmed Glaucoma Valve Implantation on Long-term Surgical Outcomes
- Ahmed Valve Implantation for Refractory Glaucoma following Pars Plana Vitrectomy
- Ciliary Sulcus Ahmed Valve Implantation