J Korean Ophthalmol Soc.
2010 Feb;51(2):286-291. 10.3341/jkos.2010.51.2.286.
Orbital Apex Syndrome with Nasal Type Natural Killer(NK)/T-cell Lymphoma of Sphenoid and Ethmoid Sinus
- Affiliations
-
- 1Department of Ophthalmology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. ophmoon@hanmail.net
- 2Department of Pathology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2213154
- DOI: http://doi.org/10.3341/jkos.2010.51.2.286
Abstract
- PURPOSE
To report a case of nasal-type NK/T cell lymphoma occurring in the sphenoid and ethmoid sinuses of an orbital apex syndrome patient.
CASE SUMMARY
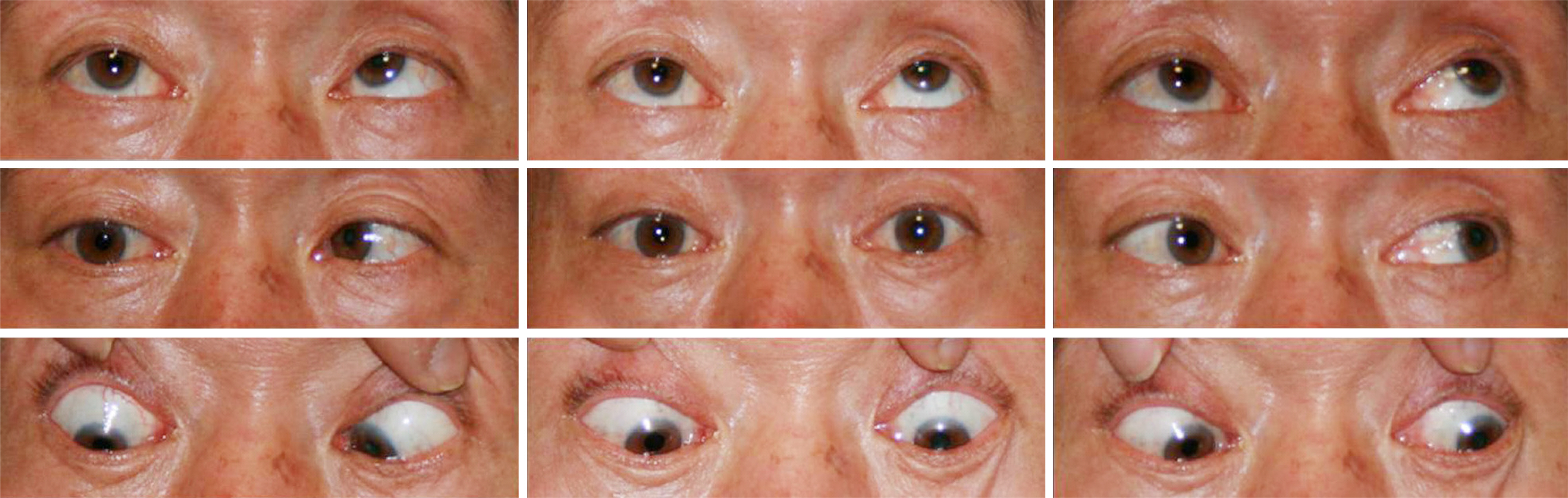
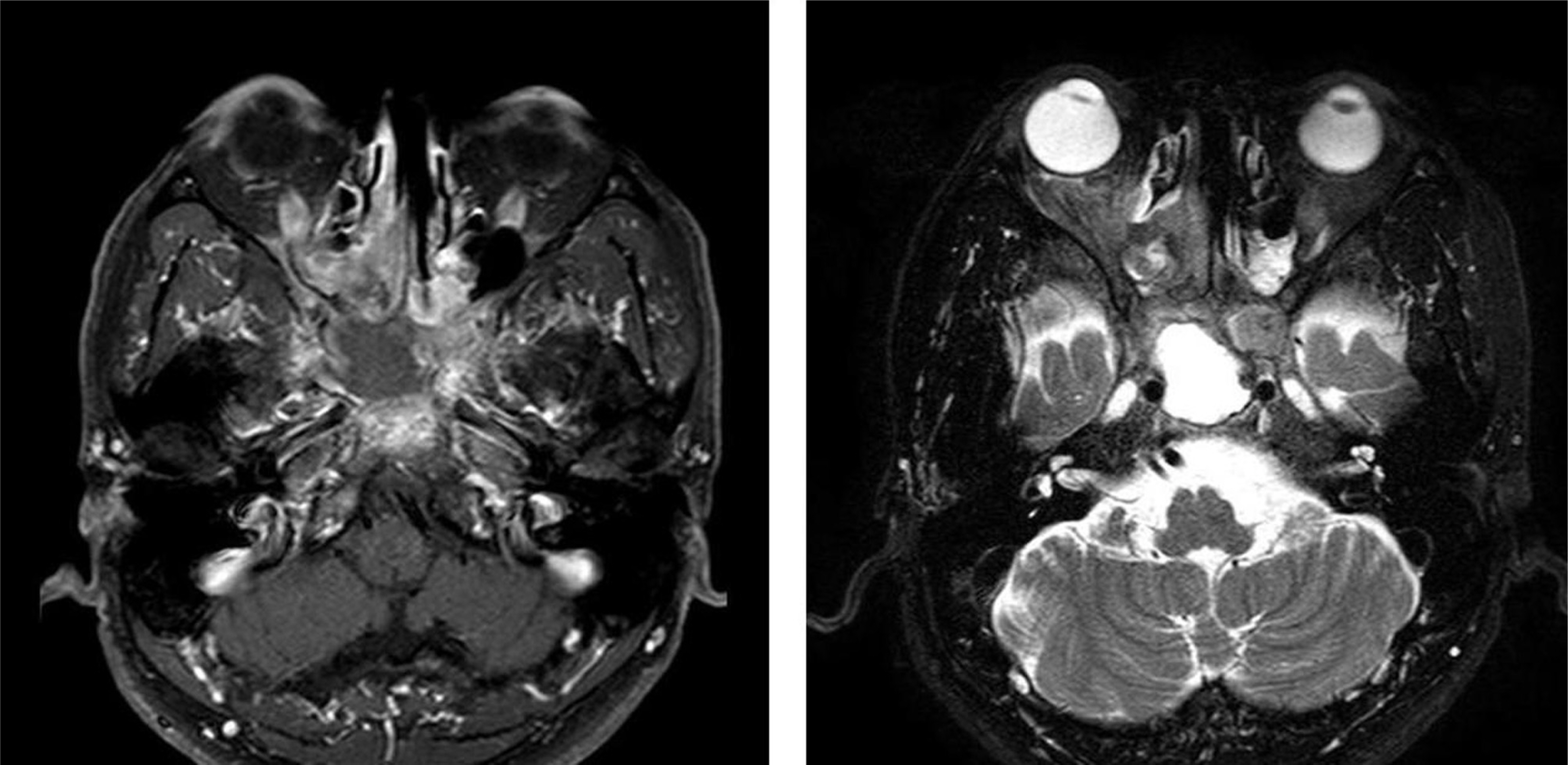
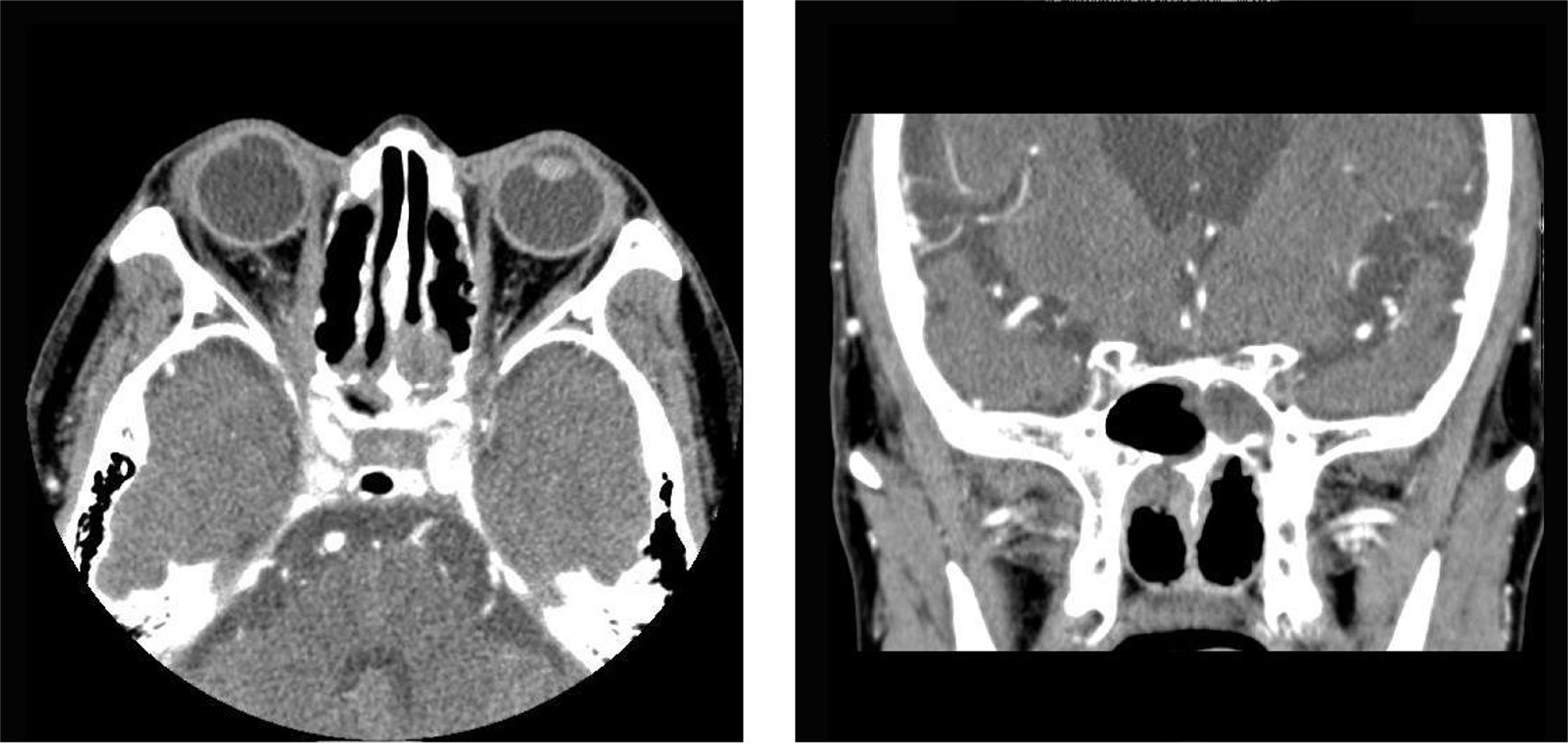
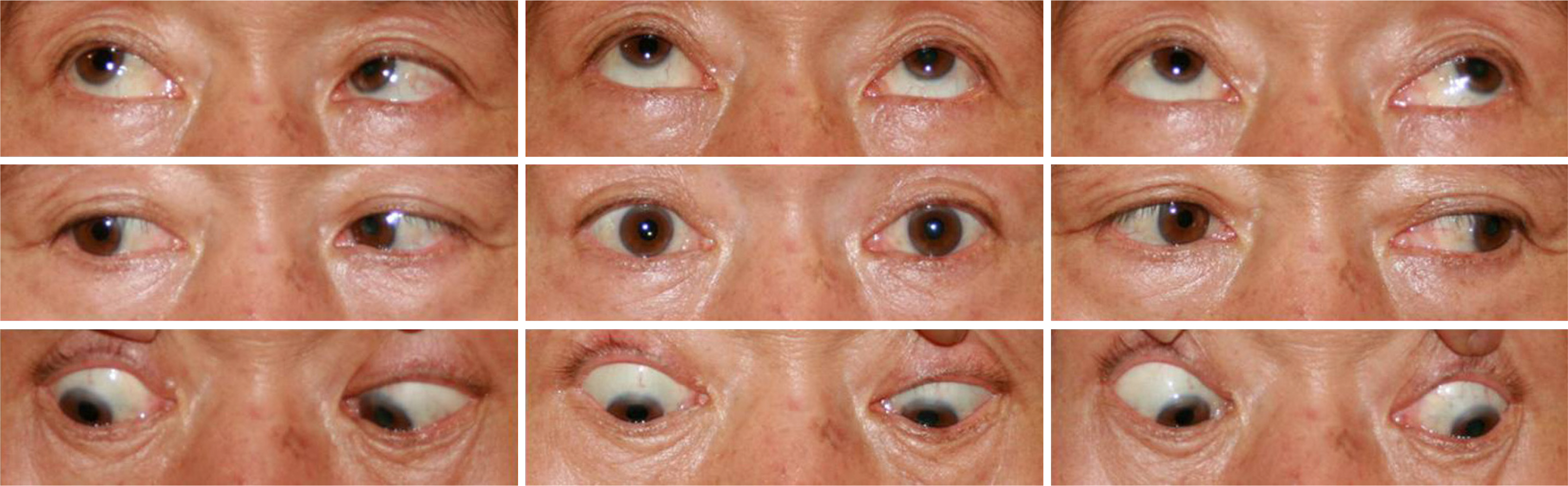
A 61-year-old male patient visited our hospital for the impairment of vision in the right eye for the previous month, and for right-side blepharoptosis, pain around the eyeball, and limitation of extraocular movement in the right eye for three days earlier. In MRI (magnetic resonance image) and CT (computed tomography), shades with vague boundaries were observed in the right sphenoid and ethmoid sinuses, and open biopsy and decompression were performed for the lesions. After the surgery, the vision of the right eye increased, and improvement was observed in the right blepharoptosis, the pain around the eyeball, and in the limitation of motility of the extraocular muscle in the right eye. The patient was diagnosed with nasal type NK/T cell lymphoma in biopsy, and radiotherapy and chemotherapy were performed.
MeSH Terms
Figure
Cited by 3 articles
-
A Case of Paranasal Diffuse Large B-Cell Lymphoma with the Orbital Invasion Masquerading as Chronic Sinusitis
Young Ji Lee, Ji He Lim, Helen Lew
J Korean Ophthalmol Soc. 2011;52(11):1351-1356. doi: 10.3341/jkos.2011.52.11.1351.Presumed Intraocular Natural Killer/T-cell Lymphoma Combined with Nasal Lymphoma
Hoon Seok Jeong, Sang Hui Park, Jae Hoon Lee, Dae Yeong Lee, Dong Heun Nam
J Korean Ophthalmol Soc. 2011;52(7):871-875. doi: 10.3341/jkos.2011.52.7.871.A Case of Orbital Apex Syndrome Induced by Penetrating Orbital Injury with Long-Term Results
Sung Uk Baek, Min Joung Lee
J Korean Ophthalmol Soc. 2013;54(8):1275-1281. doi: 10.3341/jkos.2013.54.8.1275.
Reference
-
References
1. Yeh S, Foroozan R. Orbital apex syndrome. Curr Opin aberrations. 2004; 15:490–8.
Article2. Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Arch Neurol. 1996; 53:967–71.
Article3. Lenzi GL, Fieschi C. Superior orbital fissure syndrome. Review of 130 cases. Eur Neurol. 1977; 16:23–30.4. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphoma. Cancer. 1972; 29:252–60.5. Reddy S, Pellettiere E, Saxena V, Hendrickson FR. Extranodal non-Hodgkin's lymphoma. Cancer. 1980; 46:1925–31.
Article6. Rudders RA, Ross ME, Delellis RA. Primary extranodal aberrations. Response to treatment and factors influencing prognosis. Cancer. 1978; 42:406–16.7. Frierson HF Jr, Mills SE, Innes DJ Jr. Non-Hodgkin's aberrationss of the sinonasal region: Histologic subtypes and their aberrations features. Am J Clin Pathol. 1984; 81:721–7.8. Deleu D, Lagopoulos M, al Moundhry M, Katchy K. Isolated bilateral abducens nerve palsy in primary sphenoidal sinus non-Hodgkin lymphoma. Acta Neurol Belg. 2000; 100:103–6.9. Ferrario F, Roselli R, Piantanida R, et al. Primary lymphoma of the sphenoid sinus. Report of a case and review of the literature. Ann Otolaryngol Chir Cervicofac. 1995; 112:298–302.10. Métellus P, Fuentes S, Figarella-Branger D, et al. Sphenoid sinus lymphoma. Case report and review of the literature. Neurochirurgie. 2002; 48:522–6.11. Roth DB, Siatkowski RM. Bilateral blindness as the initial aberrations of lymphoma of the sphenoid sinus. Am J Ophthalmol. 2000; 129:256–8.12. Ueba T, Miyatake S, Hashimoto N, Kikuchi H. Primary aberrations lymphoma in the sphenoid sinus with orbital apex aberrations: a case report. No Shinkei Geka. 1992; 20:283–7.13. Weber AL, Loewenheim H. Lymphoma of the sphenoid sinus presenting as an expansile mass. Ann Otol Rhinol Laryngol. 1993; 102:318–21.
Article14. Chen SM, Chang CN, Wei KC, et al. Sellar lymphoma mimicking sphenoid infection presenting with cavernous sinus syndrome. J Clin Neurosci. 2008; 15:1148–51.
Article15. Park YM, Cho JH, Cho J-Y, et al. Non-Hodgkin's lymphoma of the sphenoid sinus presenting as isolated oculomotor nerve palsy. World J Surg Oncol. 2007; 5:86–9.
Article16. Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood. 2005; 105:3768–85.
Article17. Mehta V, Balachandran C, Bhat S, et al. Nasal NK/T cell aberrations presenting as a lethal midline granuloma. Indian J Dermatol Venereol Leprol. 2008; 74:145–7.18. Cheung MM, Chan JK, Lau WH, et al. Primary non-Hodgkin's lymphoma of the nose and nasopharynx: clinical features, tumor immunophenotype, and treatment outcome in 113 patients. J aberrations Oncol. 1998; 16:70–7.
Article19. Choi KH, Lee SJ, Suh YL, Kim YD. Nasal type natural killer/ T-cell lymphoma of the orbit. J Korean Ophthalmol Soc. 2004; 45:2145–50.20. Jaffe ES, Chan JK, Su IJ, et al. Report of the workshop on nasal and related extranodal angiocentric T/natural killer cell aberrationss. Definitions, differential diagnosis, and epidemiology. Am J Surg Pathol. 1996; 20:103–11.21. Arber DA, Weiss LM, Albújar PF, et al. Nasal lymphomas in Peru high incidence of T cell immunophenotype and Epstein-Barr virus infection. Am J Surg Pathol. 1993; 17:392–9.22. Chan JK, Ng CS, Lau WH, Lo ST. Most nasal/nasopharyngeal lymphomas are peripheral T-cell neoplasms. Am J Surg Pathol. 1987; 11:418–29.
Article23. Suzuki R, Takeuchi K, Ohshima K, Nakamura S. Extranodal NK/T cell lymphoma: diagnosis and treatment cues. Hematol Oncol. 2008; 26:66–72.24. Ohshima K, Suzumiya J, Shimazaki K, et al. Nasal T/NK cell aberrations commonly express perforin and Fas ligand: important mediators of tissue damage. Histopathology. 1997; 31:444–50.25. Mori N, Yatabe Y, Oka K, et al. Expression of perforin in nasal lymphoma. Am J Pathol. 1996; 149:699–705.26. Barrionuevo C, Zaharia M, Martinez MT, et al. Extranodal NK/T-cell lymphoma, nasal type: study of clinicopathologic and prognosis factors in a series of 78 cases from peru. Appl Immunohistochem Mol Morphol. 2007; 15:38–44.
Article27. Kuo TT, Shih LY, Tsang NM. Nasal NK/T cell lymphoma in Taiwan: a clinicopathologic study of 22 cases, with analysis of histologic subtypes, Epstein-Barr virus LMP-1 gene association, and treatment modalities. Int J Surg Pathol. 2004; 12:375–87.
Article28. Ng CS, Chan JK, Lo ST. Expression of natural killer cell markers in non-Hodgkin's lymphomas. Hum Pathol. 1987; 18:1257–62.
Article29. Wolfsberger S, Ba-Ssalamah A, Pinker K, et al. Application of three-tesla magnetic resonance imaging for diagnosis and surgery of sellar lesions. J Neurosurg. 2004; 100:278–86.
Article30. Weber AL, Rahemtullah A, Ferry JA. Hodgkin and non-Hodgkin lymphoma of the head and neck: clinical, pathologic, and imaging evaluation. Neuroimaging Clin N Am. 2003; 13:371–92.31. Bisdas S, Fetscher S, Feller AC, et al. Primary B cell lymphoma of the sphenoid sinus: CT and MRI characteristics with correlation to perfusion and spectroscopic imaging features. Eur Arch aberrations. 2007; 264:1207–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nasal CD56+ NK/T Cell Lymphoma Mimicking Cellulitis which Developed after Persistent Orbital Swelling
- A Case of Nasal Type NK/T-cell Lymphoma
- A Case of Primary Nasal CD56+ NK/T cell Lymphoma with Cutaneous Involvement
- A Case of Natural Killer T-cell Lymphoma of the Tongue
- A Case of Extranodall NK/T-cell Lymphoma, Nasal type