J Korean Ophthalmol Soc.
2009 Sep;50(9):1427-1431. 10.3341/jkos.2009.50.9.1427.
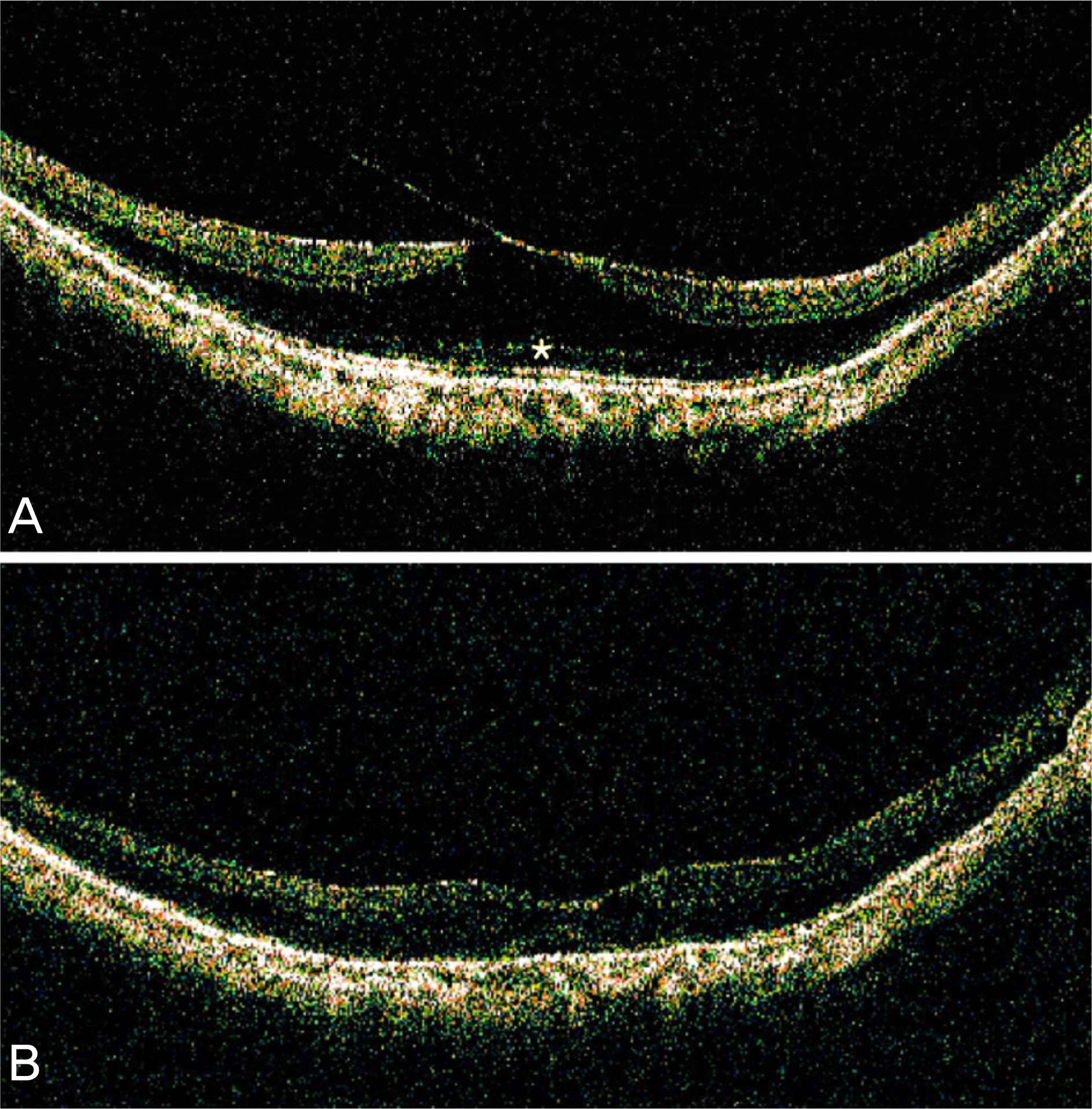
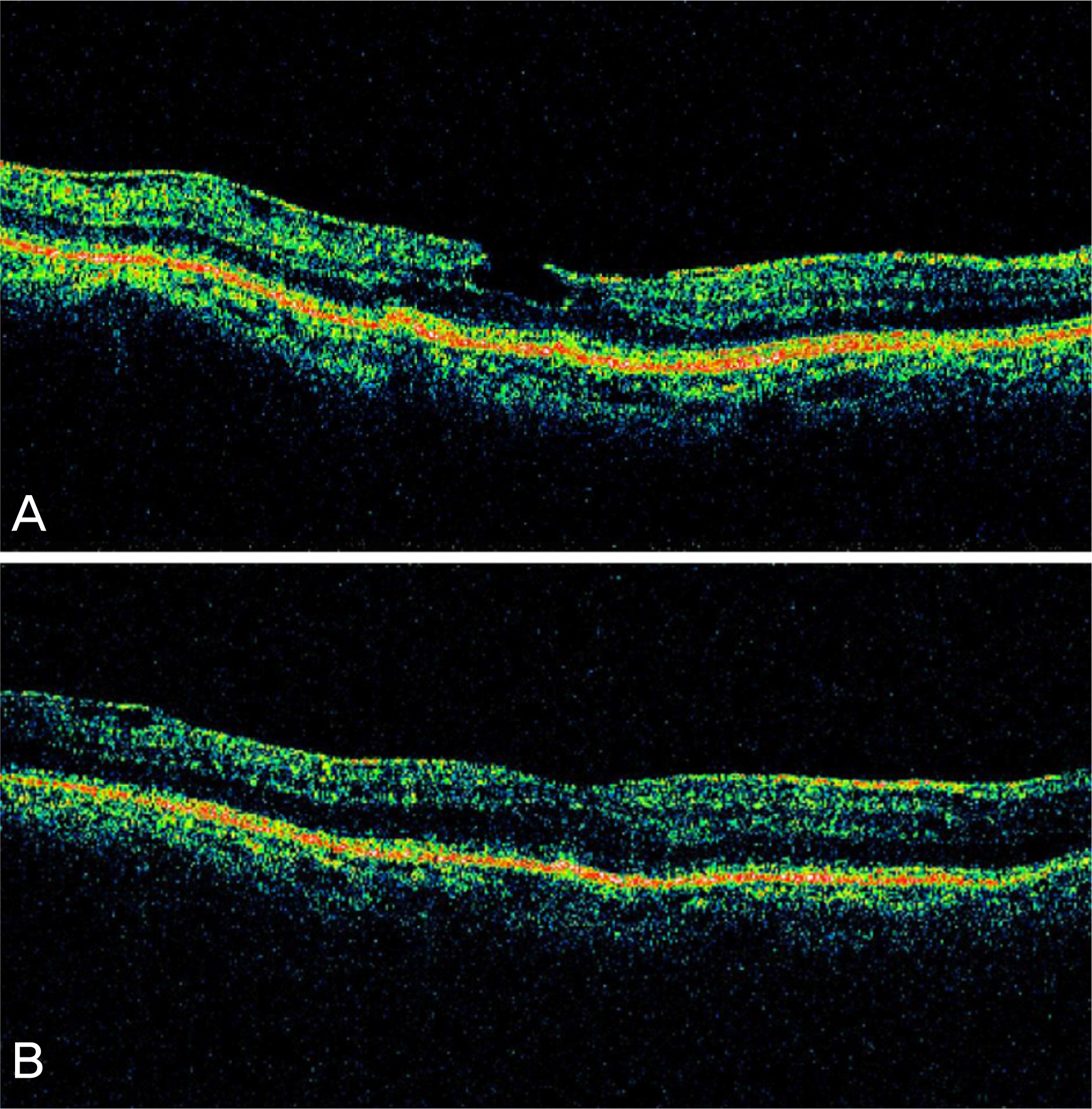
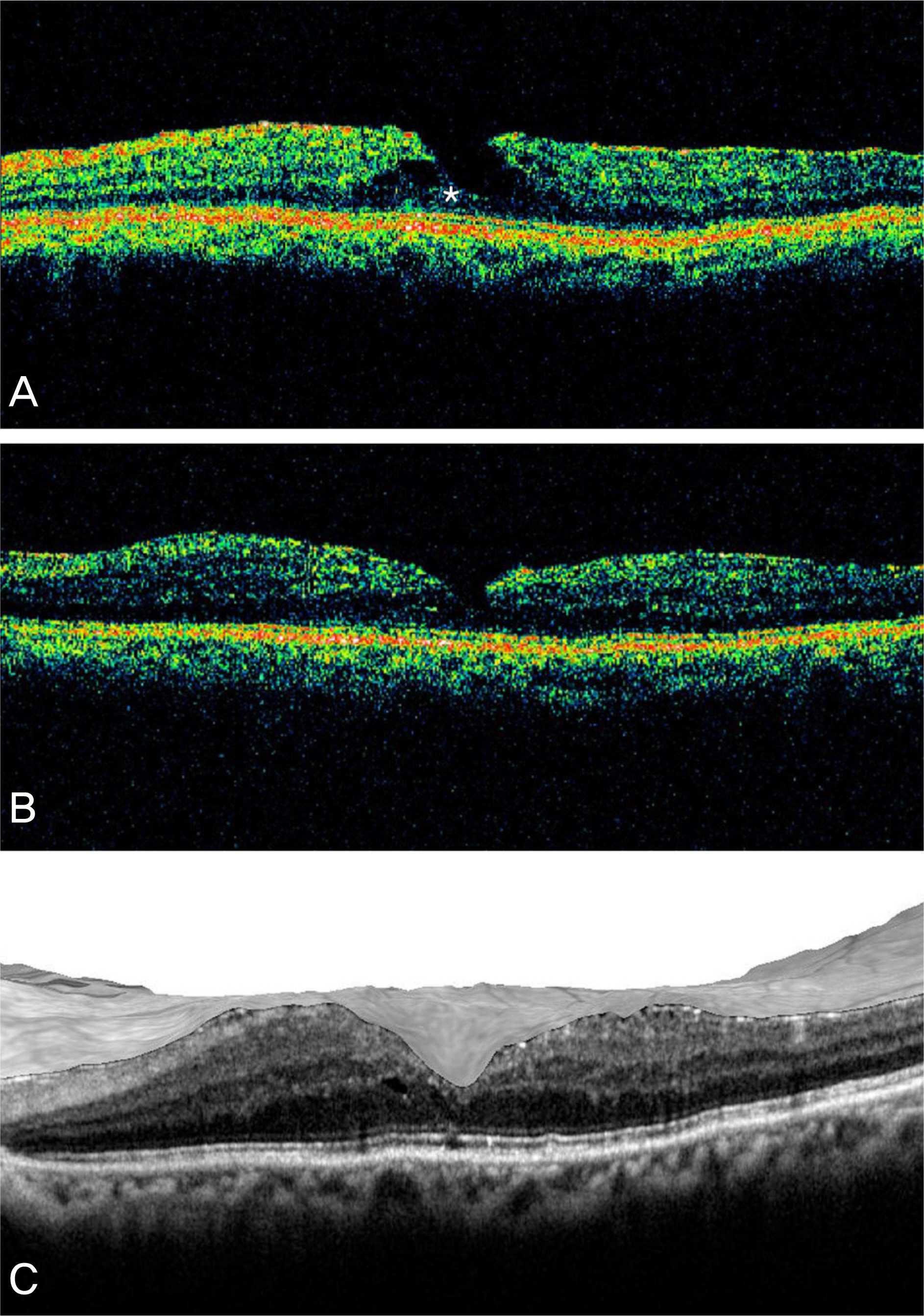
Four Cases of Pars Plana Vitrectomy for Treatment of Symptomatic Lamellar Macular Holes
- Affiliations
-
- 1Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. eyekim@kuh.ac.kr
- KMID: 2212630
- DOI: http://doi.org/10.3341/jkos.2009.50.9.1427
Abstract
- PURPOSE
To report the results of pars plana vitrectomy for the treatment of symptomatic lamellar macular holes. CASE SUMMARY: Pars plana vitrectomy with epiretinal membrane (ERM) and internal limiting membrane (ILM) stripping was performed for the treatment of lamellar holes in four patients who complained of vision loss or metamorphopsia. In three out of four patients, fluid-gas exchange with 14% C3F8 was performed and patients were instructed to maintain aprone position for 7 days after surgery. Postoperatively, the improvement of visual acuity, foveal contour, and disappearance of metamorphopsia were achieved in three patients. However, full-thickness macular hole (FTMH) developed in one patient after vitrectomy. Repeated fluid-gas exchange was performed and the patient was instructed to maintain a prone position, however, the FTMH did not close. CONCLUSIONS: In patients with visual loss or metamorphopsia, vitrectomy with ERM and ILM stripping appears to be a beneficial treatment. FTMH developed after surgery in one patient, therefore further study is needed to elucidate the prognostic factors for the development of FTMH.
MeSH Terms
Figure
Cited by 1 articles
-
The Effect of Internal Limiting Membrane Peeling in Epiretinal Membrane Including Pseudolamellar Macular Hole
Shin Yeop Oh, Soo Jung Lee, Jung Min Park
J Korean Ophthalmol Soc. 2013;54(7):1038-1045. doi: 10.3341/jkos.2013.54.7.1038.
Reference
-
References
1. Gass JD. Lamellar macular hole: a complication of cystoid macular edema after cataract extraction: a clinicopathologic case report. Trans Am Ophthalmol Soc. 1975; 73:231–50.2. Tanner V, Chauhan DS, Jackson TL, Williamson TH. Optical coherence tomography of the vitreoretinal interface in macular hole formation. Br J Ophthalmol. 2001; 85:1092–7.
Article3. Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995; 119:752–9.
Article4. Witkin AJ, Ko TH, Fujimoto JG, et al. Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology. 2006; 113:388–97.
Article5. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol. 1991; 109:654–9.
Article6. Hirakawa M, Uemura A, Nakano T, Sakamoto T. Pars plana vitrectomy with gas tamponade for lamellar macular holes. Am J Ophthalmol. 2005; 140:1154–5.
Article7. Kokame GT, Tokuhara KG. Surgical management of inner lamellar macular hole. Ophthalmic Surg Lasers Imaging. 2007; 38:61–3.
Article8. Garretson BR, Pollack JS, Ruby AJ, et al. Sarrafizadeh R. Vitrectomy for a symptomatic lamellar macular hole. Ophthalmology. 2008 May; 115:884–6.9. Haouchine B, Massin P, Tadayoni R, et al. Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am J Ophthalmol. 2004; 138:732–9.
Article10. Chen JC, Lee LR. Clinical applications and new developments of optical coherence tomography: an evidence-based review. Clin Exp Optom. 2007; 90:317–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vitreous Surgery for Macular Hole
- Optical Coherence Tomographic Evaluation of Impending Idiopathic Macular Hole Repaired by Vitrectomy
- Three Cases of Macular Buckling for Retinal Detachment due to Macular Hole in Highly Myopic Eyes
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis
- Pars Plana Vitrectomy in Pars Planitis and Posterior Uveitis