J Korean Ophthalmol Soc.
2009 Aug;50(8):1242-1246. 10.3341/jkos.2009.50.8.1242.
Trabeculectomy for Medically Uncontrolled Acute Primary Angle-Closure Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. yongykim@mail.korea.ac.kr
- KMID: 2212542
- DOI: http://doi.org/10.3341/jkos.2009.50.8.1242
Abstract
- PURPOSE
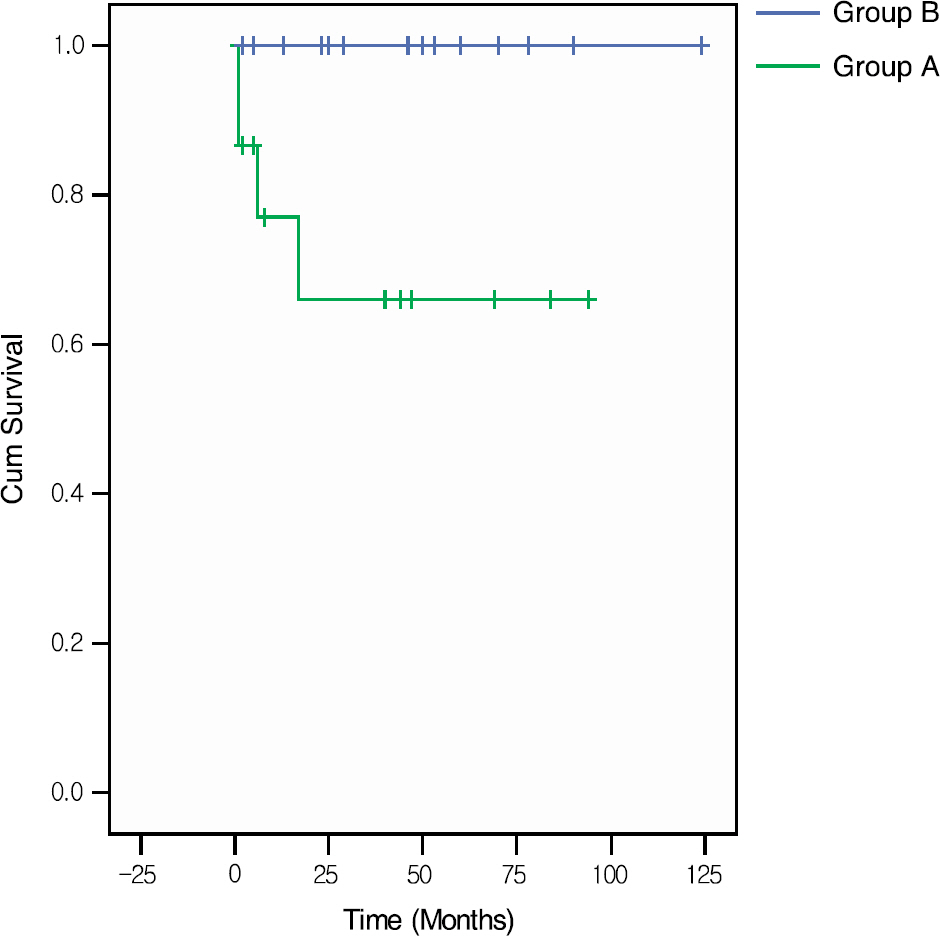
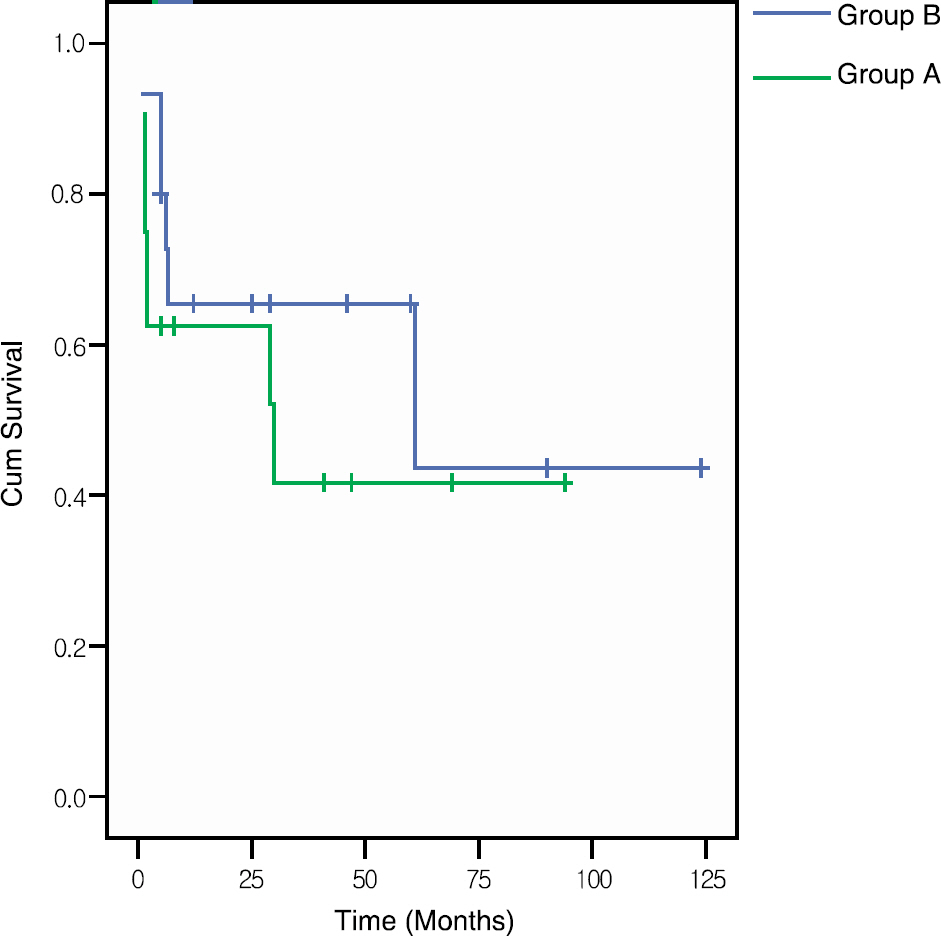
To evaluate the outcomes of trabeculectomy performed on eyes with medically uncontrolled acute angle closure glaucoma (AACG). METHODS: The authors reviewed 31 eyes of 30 acute primary angle-closure glaucoma patients who had undergone trabeculectomy. The eyes were divided into two groups: eyes which did not respond to medical and/or laser treatment (Group A, 16 eyes) and those which initially responded to medical and/or laser treatment and later had an intraocular pressure (IOP) increase (Group B, 15 eyes). Complete success was defined as a final IOP below 21 mmHg without medication, and qualified success was defined as a final IOP below 21 mmHg with medication. Patients whose postoperative IOP was 22 mmHg or greater on at least two serial measurements or who required additional glaucoma surgery were classified as failures. RESULTS: The mean follow-up was 43.1+/-32.3 months. The five-year qualified success rate was 56.3% in Group A and 100% in Group B (log-rank test, p=0.02). The preoperative IOP was significantly higher in Group A (38.0+/-11.5 mmHg) than in Group B (21.8+/-12.2 mmHg) (p<0.01). Factors found not to be significant included age, gender, peripheral anterior synechiae, a glaucomatous optic disc, and visual field damage. The postoperative complications were similar between the two groups (p>0.05). CONCLUSIONS: The medically uncontrolled AACG appears to have an adverse effect on the outcome of trabeculectomy. Success of trabeculectomy in AACG seems to be inversely related with elevated preoperative intraocular pressure.
MeSH Terms
Figure
Reference
-
References
1. Aung T, Ang LP, Chan SP, Chew PT. Acute primary angle− closure: long-term intraocular pressure outcome in Asian eyes. Am J Ophthalmol. 2001; 131:7–12.2. Nolan WP, Foster PJ, Devereux JG, et al. YAG laser iridotomy treatment for primary angle closure in east Asian eyes. Br J Ophthalmol. 2000; 84:1255–9.
Article3. Aung T, Tow SL, Yap EY, et al. Trabeculectomy for acute primary angle closure. Ophthalmology. 2000; 107:1298–302.
Article4. Alsagoff Z, Aung T, Ang LP, Chew PT. Long-term clinical course of primary angle-closure glaucoma in an Asian population. Ophthalmology. 2000; 107:2300–4.
Article5. Chew P, Aung T. Controversies in acute primary angle closure glaucoma in Chinese people. Aust N Z J Ophthalmol. 1999; 27:358–9.
Article6. Yoon JS, Kim CY, Hong YJ. Primary trabeculectomy with Mitomycin C for medically uncontrolled angle closure glaucoma. J Korean Ophthalmol Soc. 2004; 45:783–9.7. Uhm KB, Song YJ, Han JI, Hong C. The factors influencing the outcome of trabeculectomy in the medically uncontrolled primary angle-closure glaucoma. J Korean Ophthalmol Soc. 2002; 43:1451–60.8. Sawada A, Aoyama A, Yamamoto T, Takatsuka N. Long-term therapeutic outcome of acute primary angle closure in Japanese. Jpn J Ophthalmol. 2007; 51:353–9.
Article9. Chung JH, Park JS, Choi YI. Long-term intraocular pressure outcome after successful laser iridotomy for the acute primary angle-closure glaucoma. J Korean Ophthalmol Soc. 2003; 44:1102–6.10. Jacobi PC, Dietlein TS, Krieglstein GK. Adjunctive mitomycinC in primary trabeculectomy in young adults: a long-term study of case-matched young patients. Graefes Arch Clin Exp Ophthalmol. 1998; 236:652–7.11. Robin AL, Ramakrishnan R, Krishnadas R, et al. A long-term dose-response study of mitomycin in glaucoma filtration surgery. Arch Ophthalmol. 1997; 115:969–74.
Article12. Nuijts RM, Vermimmen RC, Webers CA. Mitomycin C primary trabeculectomy in primary glaucoma of white patients. J Glaucoma. 1997; 6:293–7.
Article13. Cheung JC, Wright MM, Murali S, Pederson JE. Intermediate-term outcome of variable dose mitomycin C filtering surgery. Ophthalmology. 1997; 104:143–9.
Article14. Miets H, Krieglstein GK. Three-year follow-up of trabeculec-tomies performed with different concentrations of mitomycin C. Ophthalmic Surg Lasers. 1998; 29:628–34.15. Sanders SP, Cantor LB, Dobler AA, Hoop JS. Mitomycin C in higher risk trabeculectomy: a prospective comparison of 0.2 to 0.4 mg/ml disease. J Glaucoma. 1999; 8:193–8.16. Mietz H, Krieglstein GK. Short term clinical results and compli-cations of trabeculectomies performed with mitomycin C using different concentrations. Int Ophthalmol. 1995; 19:51–6.17. Kim YY, Sexton RM, Shin DH, et al. Outcomes of primary phakic trabeculectomies without versus with 0.5 to 1 minute versus 3 to 5 minute mitomycin C. Am J Ophthalmol. 1998; 126:755–62.18. Costa VP, Comegno PE, Vasconcelos JP, et al. Low-dose mitomycin C trabeculectomy in patient with advanced glaucoma. J Glaucoma. 1996; 5:193–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Trabeculectomy with Mitomycin C for Medically Uncontrolled Angle Closure Glaucoma
- The Factors Influencing the Outcome of Trabeculectomy in the Medically Uncontrolled Primary Angle-Closure Glaucoma
- A Clinical Evaluations of Trabeculectomy
- Clinical Results of Trabeculectomy
- The Factors Affect on the Success Rate of the Trabeculectomy