J Korean Ophthalmol Soc.
2009 Jul;50(7):976-983. 10.3341/jkos.2009.50.7.976.
Long-Term Results of Reconstruction of Orbital Wall Fracture With Resorbable Copolymer Mesh
- Affiliations
-
- 1Department of Ophthalmology, Wallace Memorial Baptist Hospital, Busan, Korea. Kwak7513@lycos.co.kr
- 2Elephant Eye Clinic, Busan, Korea.
- KMID: 2212480
- DOI: http://doi.org/10.3341/jkos.2009.50.7.976
Abstract
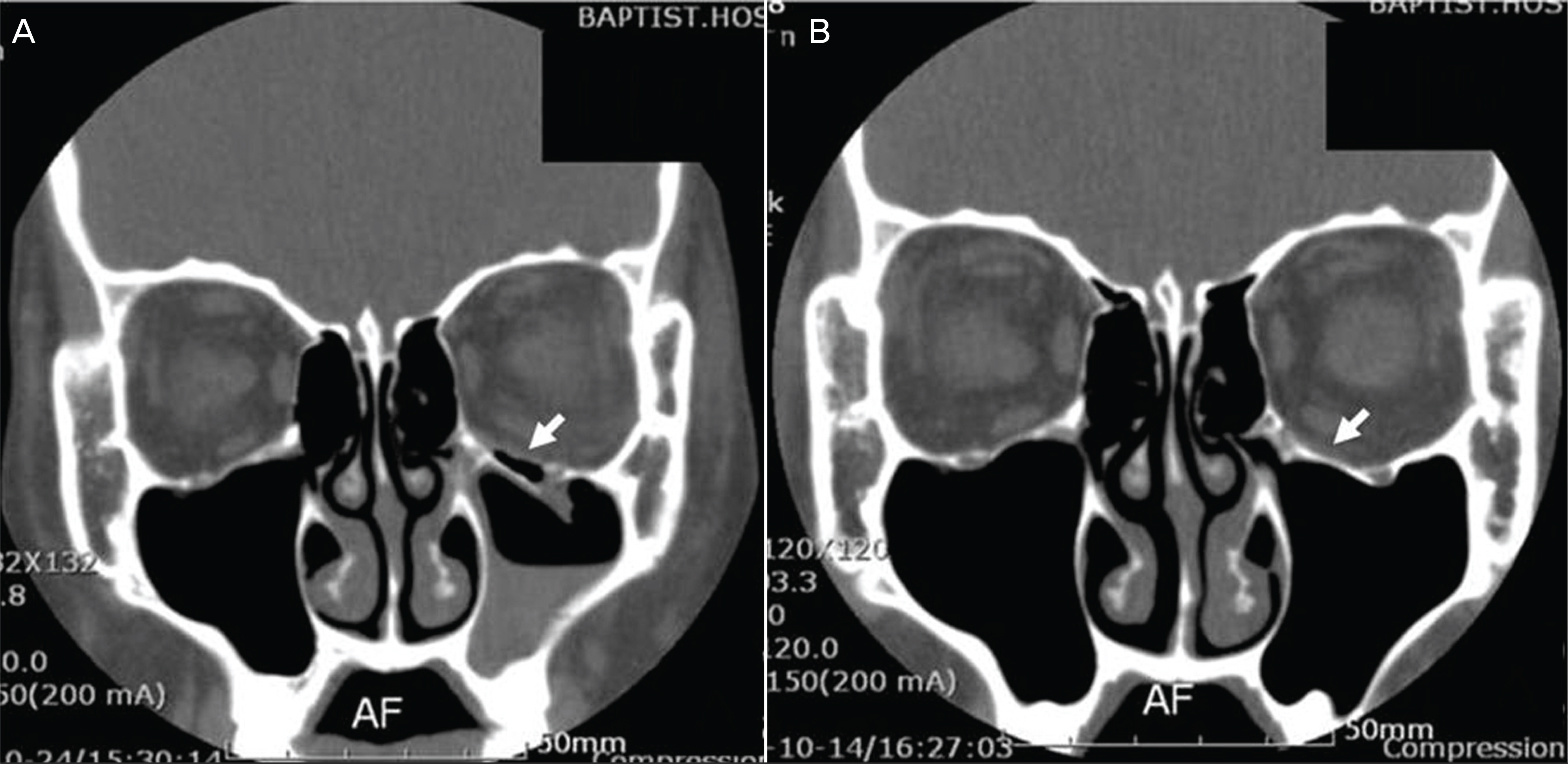
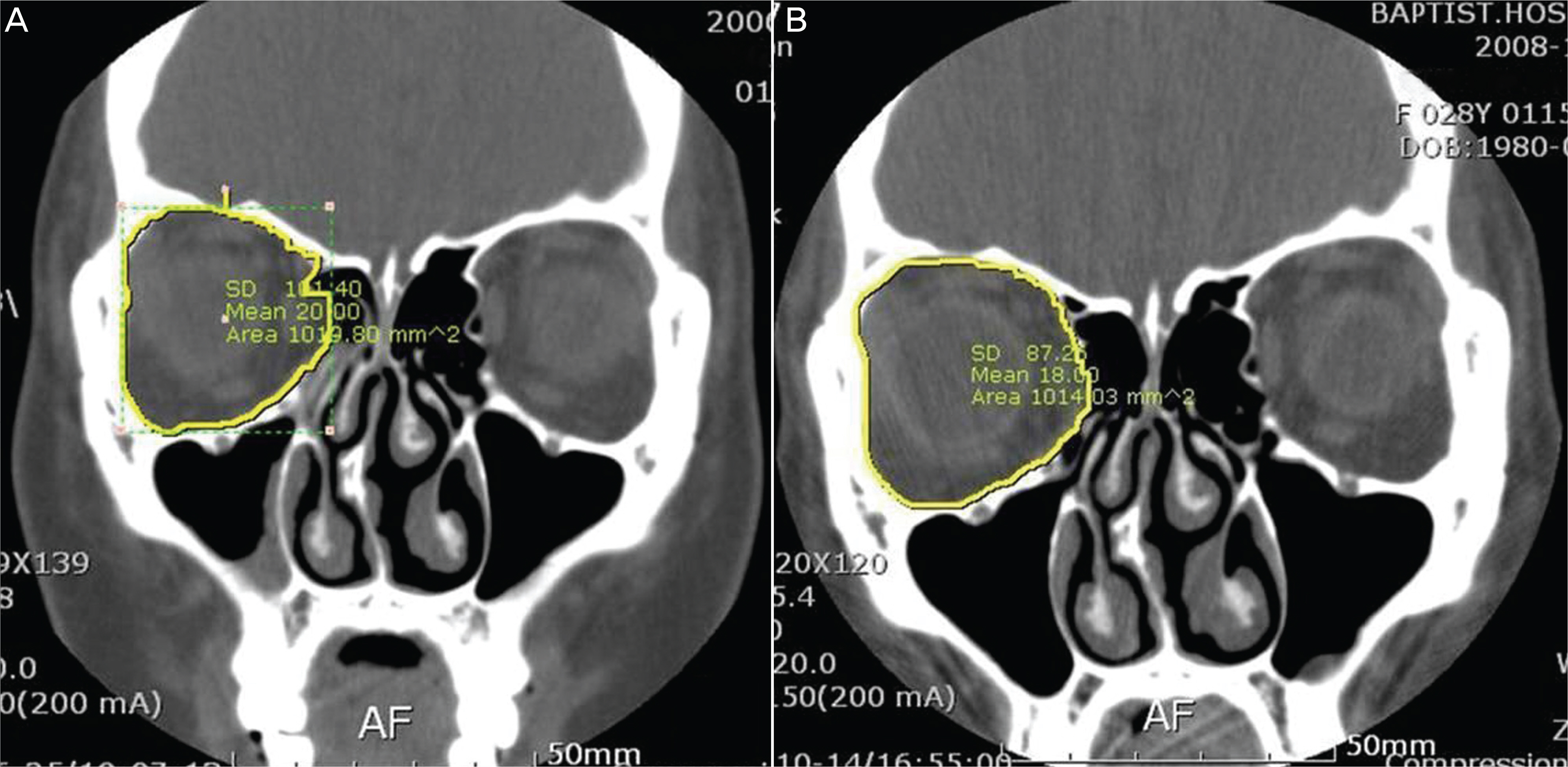
- PURPOSE
This study examined the postoperative long-term results of the reconstruction of orbital wall fracture using Macropore(R). METHODS: The long-term results for 10 patients who were diagnosed with orbital wall fracture and received the repair of orbital wall fracture using Macropore(R), were examined postoperatively after an average of 23.5 months. RESULTS: The mean difference in orbital volume between the fractured orbit and the unaffected orbit after an average of 23.5 months postoperatively was 1.01+/-0.70 cm3 (4.75+/-2.92%), which slightly increased compared to 0.70+/-0.52 cm3 (3.26+/-2.10%) immediately after the operation, although the difference was not statistically significant (p-value=0.190). At the last follow-up, the shape of Macropore(R) was not observed in 3 out of the 10 patients, and intense ossification was observed at the site of fracture in 6 patients. At the last follow-up, one patient showed 1.5 mm enophthalmos, and the other patients did not show the occurrence of diplopia or the progress of enophthalmos. CONCLUSIONS: According to the long-term results of the reconstruction of orbital wall fracture, Macropore(R) is considered an implant that produces a safe and satisfactory effect without notable complications.
Figure
Reference
-
References
1. Courtney DJ, Thomas S, Whitfield PH. Isolated orbital blow out fractures: Survey and review. Br J Oral Maxillofac Surg. 2000; 38:496–504.2. Enislidis G. Treatment of orbital fractures. The case for treatment with resorbable materials. J Oral Maxillofac Surg. 2004; 62:869–72.
Article3. Kontio R. Treatment of orbital fractures. The case for reconstruction with autogenous bone. J Oral Maxillofac Surg. 2004; 62:863–8.
Article4. Potter JK, Ellis E. Biomaterials for reconstruction of the internal orbit. J Oral Maxillofac Surg. 2004; 62:1280–97.
Article5. Rubin PA, Bilyk JR, Shore JW. Orbital Reconstruction using porous polyethylene sheets. Ophthalmology. 1994; 101:1679–708.
Article6. Lin KY, Bartlett SP, Yaremchuk MJ, et al. The effect of rigid fixation on the survival of onlay bone graft: An experimental study. Plast Reconstr Surg. 1990; 86:449–56.7. Converse JM, Smith B, Obear MF, Wood-Smith D. Blowout fracture of the floor of the orbit: a ten year survey. Plast Reconstr Surg. 1967; 39:20–36.8. Bae JH, Kwak MS. Clinical experience of orbital wall reconstruction using Medpor barrier sheet implant. J Korean Ophthalmol Soc. 2001; 42:1515–22.9. Lee SH, Cho KS. Clinical experience with Medpor implant through transconjunctival incision in blowout fractures. J Korean Ophthalmol Soc. 1998; 39:823–9.10. Kim HK, Lim HS, Chung HS. Surgical effect of Medpor in the reconstruction of orbital wall fracture. J Korean Ophthalmol Soc. 1998; 39:623–30.11. Raz S. Gelfilm and blowout fractures. J Laryngol Otol. 1976; 90:699–702.
Article12. McVicar I, Hatton PV, Brook IM. Self-reinforced polyglycolic acid membrane: A bioresorbable material for orbital floor repair. Br J Oral Maxillofac Surg. 1995; 33:220–3.13. Iizuka T, Mikkonen P, Paukku P, et al. Reconstruction of orbital floor with polydioxanone plate. Int J Oral Maxillofac Surg. 1991; 20:83–7.14. Kontio R, Suuronen R, Salonen O, et al. Effectiveness of operative treatment of internal orbital wall fracture with polydioxanone implant. Int J Oral Maxillofac Surg. 2001; 30:278–85.
Article15. Park YJ, Chung IY, Seo SW. An analysis of orbital reconstruction with bioresorbable plate through orbital volume assessment. J Korean Ophthalmol Soc. 2008; 49:1046–53.
Article16. Al-Sukhun J, Törnwall J, Lindqvist C, et al. Bioresorbable poly-L /DL-lactide plates are reliable for repairing large inferior orbital wall bony defects: a pilot study. J Oral Maxillofac Surg. 2006; 64:47–55.17. Chi MJ, Jeung JW, Lee JH. Reconstruction of orbital wall fracture with resorbable copolymer mesh. J Korean Ophthalmol Soc. 2006; 47:1021–30.18. Fan X, Li J, Li H, Zhang D. Computer-assisted orbital volume measurement in the surgical correction of late enophthalmos caused by blowout fractures. Ophthal Plast Reconstr Surg. 2003; 19:207–211.
Article19. Kim TH, Jun HS, Byun YJ. The normal value of adult korean orbital volume in three-dimensional computerized tomography. J Korean Ophthalmol Soc. 2001; 42:1011–5.20. Ahlmann E, Patzakis M, Roidis N, et al. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am. 2002; 84:716–20.
Article21. Morrison AD, Sanderson RC, Moos KF. The use of Silastic as an orbital implant for reconstruction of orbital wall defects: review of 311 cases treated over 20 years. J Oral Maxillofac Surg. 1995; 53:412–7.22. Custer PL, Lind A, Trinkaus KM. Complication of Supramid orbital implants. Ophthal Plast Reconstr Surg. 2003; 19:62–7.23. Romano JJ, Iliff NT, Manson PN. Use of Medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993; 4:142–7.
Article24. Ng SG, Madill SA, Inkster CF, et al. Medpor porous polyethylene implants in orbital blowout fracture repair. Eye. 2001; 15:578–82.
Article25. Cutright DE, Hunsuck EE. The repair of fractures of the orbital floor using biodegradable polylactic acid. Oral Surg. 1972; 33:28–34.
Article26. Cordewener FW, Bos RR, Rozema FR, et al. Poly (L-lactide) implants for repair of human orbital floor defects: clinical and magnetic resonance imaging evaluation of long-term results. J Oral Maxillofac Surg. 1996; 54:9–13.27. Suuronen R, Pohjonen T, Hietanen J, et al. A 5-year in vitro and in vivo study of the biodegradation of polylactide plates. J Oral Maxillofac Surg. 1998; 56:604–14.
Article28. Peltoniemi HH, Tulamo RM, Pihlajamäki HK, et al. Conso-lidation of craniotomy lines after resorbable polylactide and titanium plating: a comparative experimental study in sheep. Plast Reconstr Surg. 1998; 101:123–33.
Article29. Al-Sukhun J, Lindqvist C. A comparative study of 2 implants used to repair inferior orbital wall bony defects: autogenous bone graft versus bioresorbable poly-L/DL-lactide plate. J Oral Maxillofac Surg. 2006; 64:1038–48.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of Orbital Wall Fracture with Resorbable Copolymer Mesh
- Comparison of Titanium Micro Mesh(R) with Titanium Mesh Screen 1.3(R) in the Reconstruction of Medial Orbital wall Fracture
- The Inferior Orbital Wall Reconstruction by Titanium Micro-mesh Remodeling
- Reconstruction of Orbital bone Fractures with Titanium Mesh
- Orbital wall restoring surgery with resorbable mesh plate