J Korean Surg Soc.
2012 Oct;83(4):246-249. 10.4174/jkss.2012.83.4.246.
Liver abscess developed after cadaveric liver transplantation due to ligation of an accessory right hepatic artery of the donor graft
- Affiliations
-
- 1Division of Hepato-bilio-pancreas Surgery & Liver Transplantation, Department of Surgery, Korea University College of Medicine, Seoul, Korea. kimds1@korea.ac.kr
- KMID: 2212318
- DOI: http://doi.org/10.4174/jkss.2012.83.4.246
Abstract
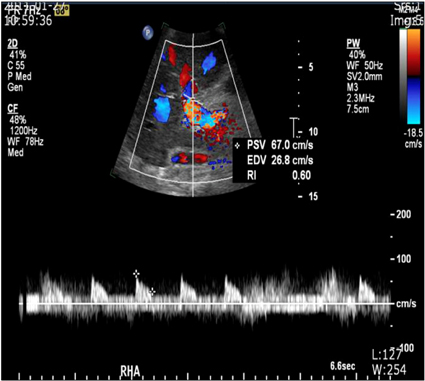
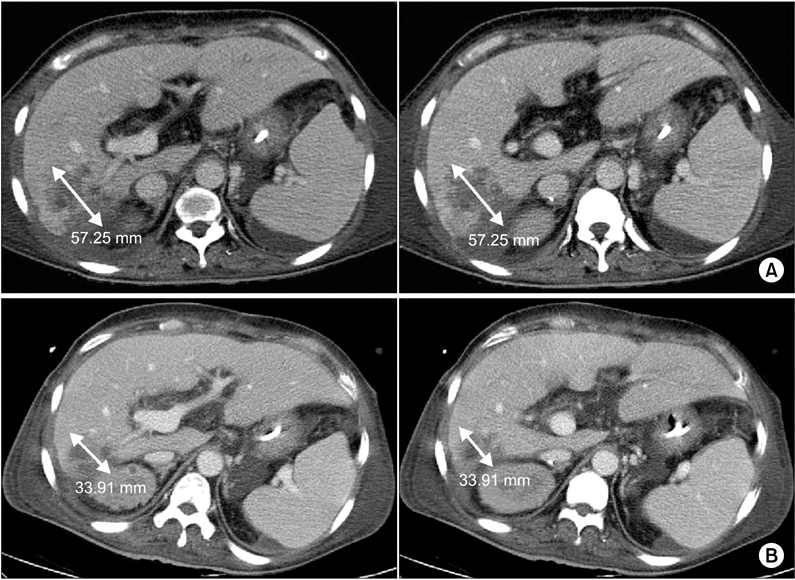
- It is important that extrahepatic arteries are identified precisely at the time of graft procurement. We present a case where the accessory right hepatic artery of the liver was ligated leading to postoperative liver abscess formation in the liver graft. A forty-seven-year-old female patient diagnosed with liver cirrhosis underwent orthotopic cadaveric liver transplantation due to altered mentality. The donor graft showed a variant of the hepatic artery anatomy where an accessory right hepatic artery arose from the superior mesenteric artery. This artery was accidentally transected during procurement. Since the back bleeding test using perfusion fluid was good, the artery was ligated. Postoperative abdominal computed tomography scan revealed a 6 cm low attenuating lesion in the liver. The patient underwent conservative treatment. We believe that even small accessory arteries (1 to 2 mm) should be reconstructed whenever possible to avoid postoperative complications such as liver abscess.
MeSH Terms
Figure
Reference
-
1. Tzakis AG, Gordon RD, Shaw BW Jr, Iwatsuki S, Starzl TE. Clinical presentation of hepatic artery thrombosis after liver transplantation in the cyclosporine era. Transplantation. 1985. 40:667–671.2. Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966. 112:337–347.3. Nelson TM, Pollak R, Herand OJ. Anatomic variants of the celiac, superior mesenteric, and inferior mesenteric arteries and their clinical relevance. Clin Anat. 1988. 1:75–91.4. Hiatt JR, Gabbay J, Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994. 220:50–52.5. Yang SH, Yin YH, Jang JY, Lee SE, Chung JW, Suh KS, et al. Establishment of a guideline for the safe management of anatomical hepatic artery variations while performing major hepato-pancreatico-biliary surgery. J Korean Surg Soc. 2009. 76:100–108.6. Proposito D, Loinaz Segurola C, Garcia Garcia I, Jimenez C, Gonzales Pinto I, Gomez Sanz R, et al. Role of anatomic variations and methods of hepatic artery reconstruction in the incidence of thrombosis following liver transplantation. Ann Ital Chir. 2001. 72:303–314.7. Jones RM, Hardy KJ. The hepatic artery: a reminder of surgical anatomy. J R Coll Surg Edinb. 2001. 46:168–170.8. Di Benedetto F, Cautero N, De Ruvo N, Masetti M, Montalti R, Gerunda GE, et al. A new reconstruction of the accessory donor right hepatic artery with interposition of the SMA in liver transplantation. Surgery. 2006. 140:835.9. Ikegami T, Kawasaki S, Matsunami H, Hashikura Y, Nakazawa Y, Miyagawa S, et al. Should all hepatic arterial branches be reconstructed in living-related liver transplantation? Surgery. 1996. 119:431–436.10. Yanaga K, Tzakis AG, Starzl TE. Partial dearterialization of the liver allograft. Transpl Int. 1990. 3:185–188.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Variations in the origin of middle hepatic artery: a cadaveric study and implications for living donor liver transplantation
- Hepatic Artery Reconstruction Using the Right Gastroepiploic Artery for Hepatic Artery Inflow in a Living Donor Liver Transplantation
- Salvage aorto-hepatic jump graft for hepatic artery thrombosis following living donor liver transplantation: a case report with 10-year follow-up
- The Feasibility of Right Posterior Sector Graft in the Adult Living Donor Liver Transplantation
- Salvage aorto-hepatic jump graft for hepatic artery thrombosis following living donor liver transplantation: a case report with 10-year follow-up