J Korean Surg Soc.
2010 May;78(5):298-304. 10.4174/jkss.2010.78.5.298.
Clinicopathologic Analysis of Mesorectal Spread of Rectal Cancer with Whole Mount Section
- Affiliations
-
- 1Department of Surgery, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea. kangski1004@yahoo.co.kr
- 2Department of Pathology, National Health Insurance Corporation Ilsan Hospital, Goyang, Korea.
- KMID: 2211956
- DOI: http://doi.org/10.4174/jkss.2010.78.5.298
Abstract
- PURPOSE
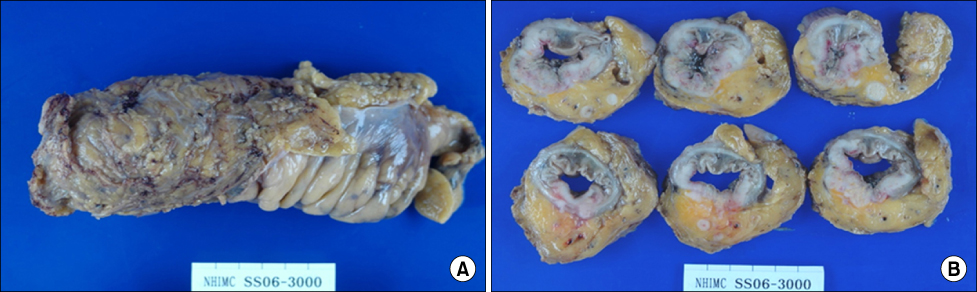
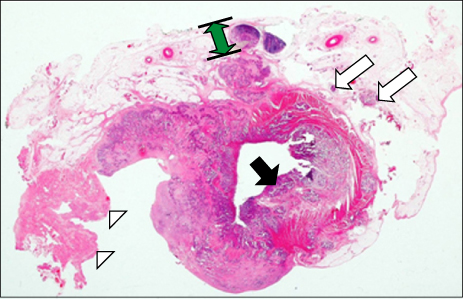
Total mesorectal excision (TME) has been widely accepted as the principal method in rectal cancer surgery and demonstrates good oncologic and functional outcome. The recurrence rate of mid-low rectal cancer surgery with TME is reported as 5~6%. Concerning local recurrence, remaining microscopic nodules in mesorectum are a major issue. In this study, we investigated mesorectal spread of tumors and exact lateral resection margin using whole mount section (WMS) to obtain correlations with other clinico-pathological variables.
METHODS
63 rectal cancer patients underwent surgery with TME and WMS at National Health Insurance Corporation Ilsan Hospital between December 2005 and October 2008. Preoperative study was made by computed tomography (CT), magnetic resonance imaging (MRI). We measured the distance from the largest cut section of the primary tumor to the nearest circumferential margin using MRI and compared them to lateral resection margins in WMS.
RESULTS
Among 63 patients, the sex ratio was 1:1.17 and the median age was 62.7 years. There were 34 patients in TNM stage III (54.0%), 21 patients in stage II (33.3%) and 8 patients in stage I (12.7%). Lateral margin involvement was predicted in 4 cases pre-operatively and confirmed in 3 cases with WMS. Micrometastasis in mesorectum was detected in 6 patients (9.5%) and all were in stage III. N stage was statistically correlated with micrometastasis (P=0.016).
CONCLUSION
WMS offers precise lateral resection margin and mesorectal spread of microscopic tumor nodules. WMS is best considered in stage III cancer to evaluate mesorectal micrometastasis. The mid-low rectal cancer cases with predicted lateral margin involvements using MRI should be operated on with great care.
MeSH Terms
Figure
Reference
-
1. Reynolds JV, Joyce WP, Dolan J, Sheahan K, Hyland JM. Pathological evidence in support of total mesorectal excision in the management of rectal cancer. Br J Surg. 1996. 83:1112–1115.2. Soreide O, Norstein J. Local recurrence after operative treatment of rectal carcinoma: a strategy for change. J Am Coll Surg. 1997. 184:84–92.3. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982. 69:613–616.4. Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986. 1:1479–1482.5. Lee KY, Kim SM, Kim NK, Park JK, Sohn SK, Min JS. Pattern of recurrence after curative resection for rectal cancer. J Korean Surg Soc. 2001. 61:588–592.6. Andreola S, Leo E, Belli F, Gallino G, Sirizzotti G, Sampietro G. Adenocarcinoma of the lower third of the rectum: metastases in lymph nodes smaller than 5 mm and occult micrometastases; preliminary results on early tumor recurrence. Ann Surg Oncol. 2001. 8:413–417.7. Baik SH, Kim NK, Lee KY, Sohn SK, Cho CH, Kim HG, et al. Prognostic significance of circumferential resection margin following a total mesorectal excision in rectal cancer. J Korean Soc Coloproctol. 2005. 21:307–313.8. Lee SH, Hernandez de Anda E, Finne CO, Madoff RD, Garcia-Aguilar J. The effect of circumferential tumor location in clinical outcomes of rectal cancer patients treated with total mesorectal excision. Dis Colon Rectum. 2005. 48:2249–2257.9. Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008. 26:303–312.10. Ono C, Yoshinaga K, Enomoto M, Sugihara K. Discontinuous rectal cancer spread in the mesorectum and the optimal distal clearance margin in situ. Dis Colon Rectum. 2002. 45:744–749.11. Wang Z, Zhou ZG, Wang C, Zhao GP, Chen YD, Gao HK, et al. Microscopic spread of low rectal cancer in regions of mesorectum: pathologic assessment with whole-mount sections. World J Gastroenterol. 2004. 10:2949–2953.12. Zhao GP, Zhou ZG, Lei WZ, Yu YY, Wang C, Wang Z, et al. Pathological study of distal mesorectal cancer spread to determine a proper distal resection margin. World J Gastroenterol. 2005. 11:319–322.13. Williams NS. The rationale for preservation of the anal sphincter in patients with low rectal cancer. Br J Surg. 1984. 71:575–581.14. Shirouzu K, Isomoto H, Kakegawa T. Distal spread of rectal cancer and optimal distal margin of resection for sphincter-preserving surgery. Cancer. 1995. 76:388–392.15. Glass RE, Ritchie JK, Thompson HR, Mann CV. The results of surgical treatment of cancer of the rectum by radical resection and extended abdomino-iliac lymphadenectomy. Br J Surg. 1985. 72:599–601.16. Quirke P, Durdey P, Dixon MF, Williams NS. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986. 2:996–999.17. Quirke P, Dixon MF. The prediction of local recurrence in rectal adenocarcinoma by histopathological examination. Int J Colorectal Dis. 1988. 3:127–131.18. Paty PB, Enker WE, Cohen AM, Lauwers GY. Treatment of rectal cancer by low anterior resection with coloanal anastomosis. Ann Surg. 1994. 219:365–373.19. Ueno H, Mochizuki H, Tamakuma S. Prognostic significance of extranodal microscopic foci discontinuous with primary lesion in rectal cancer. Dis Colon Rectum. 1998. 41:55–61.20. Cawthorn SJ, Gibbs NM, Marks CG. Clearance technique for the detection of lymph nodes in colorectal cancer. Br J Surg. 1986. 73:58–60.21. Scott N, Jackson P, al-Jaberi T, Dixon MF, Quirke P, Finan PJ. Total mesorectal excision and local recurrence: a study of tumour spread in the mesorectum distal to rectal cancer. Br J Surg. 1995. 82:1031–1033.22. Ng IO, Luk IS, Yuen ST, Lau PW, Pritchett CJ, Ng M, et al. Surgical lateral clearance in resected rectal carcinomas. A multivariate analysis of clinicopathologic features. Cancer. 1993. 71:1972–1976.23. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patient's survival. Br J Surg. 1983. 70:150–154.24. Penfold JC. A comparison of restorative resection of carcinoma of the middle third of the rectum with abdominoperineal excision. Aust N Z J Surg. 1974. 44:354–356.25. Cawthorn SJ, Parums DV, Gibbs NM, A'Hern RP, Caffarey SM, Broughton CI, et al. Extent of mesorectal spread and involvement of lateral resection margin as prognostic factors after surgery for rectal cancer. Lancet. 1990. 335:1055–1059.26. Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001. 345:638–646.27. Camma C, Giunta M, Fiorica F, Pagliaro L, Craxi A, Cottone M. Preoperative radiotherapy for resectable rectal cancer: A meta-analysis. JAMA. 2000. 284:1008–1015.28. Koyama Y, Moriya Y, Hojo K. Effects of extended systematic lymphadenectomy for adenocarcinoma of the rectum--significant improvement of survival rate and decrease of local recurrence. Jpn J Clin Oncol. 1984. 14:623–632.29. Moriya Y, Hojo K, Sawada T, Koyama Y. Significance of lateral node dissection for advanced rectal carcinoma at or below the peritoneal reflection. Dis Colon Rectum. 1989. 32:307–315.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nodal metastasis in the distal mesorectum: need for total mesorectal excision of rectal cancer
- Robotic Total Mesorectal Excision for Rectal Cancer: Current Evidences and Future Perspectives
- Total Mesorectal Excision and Preservation of Autonomic Nerves
- Lymph Node Metastases and Tumor Deposits in the Mesorectum Distal to Rectal Cancer: A Need of Total Mesorectal Excision
- Transanal Total Mesorectal Excision for Rectal Cancer: Perioperative and Oncological Outcomes