J Korean Ophthalmol Soc.
2008 May;49(5):858-864. 10.3341/jkos.2008.49.5.858.
Two Cases of Occult Macular Dystrophy in a Family
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea. jiani4@snu.ac.kr
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Gyeonggi, Korea.
- KMID: 2211720
- DOI: http://doi.org/10.3341/jkos.2008.49.5.858
Abstract
-
PURPOSE: We report two familial cases of occult macular dystrophy (OMD) presenting with a progressive decrease in central vision.
CASE SUMMARY
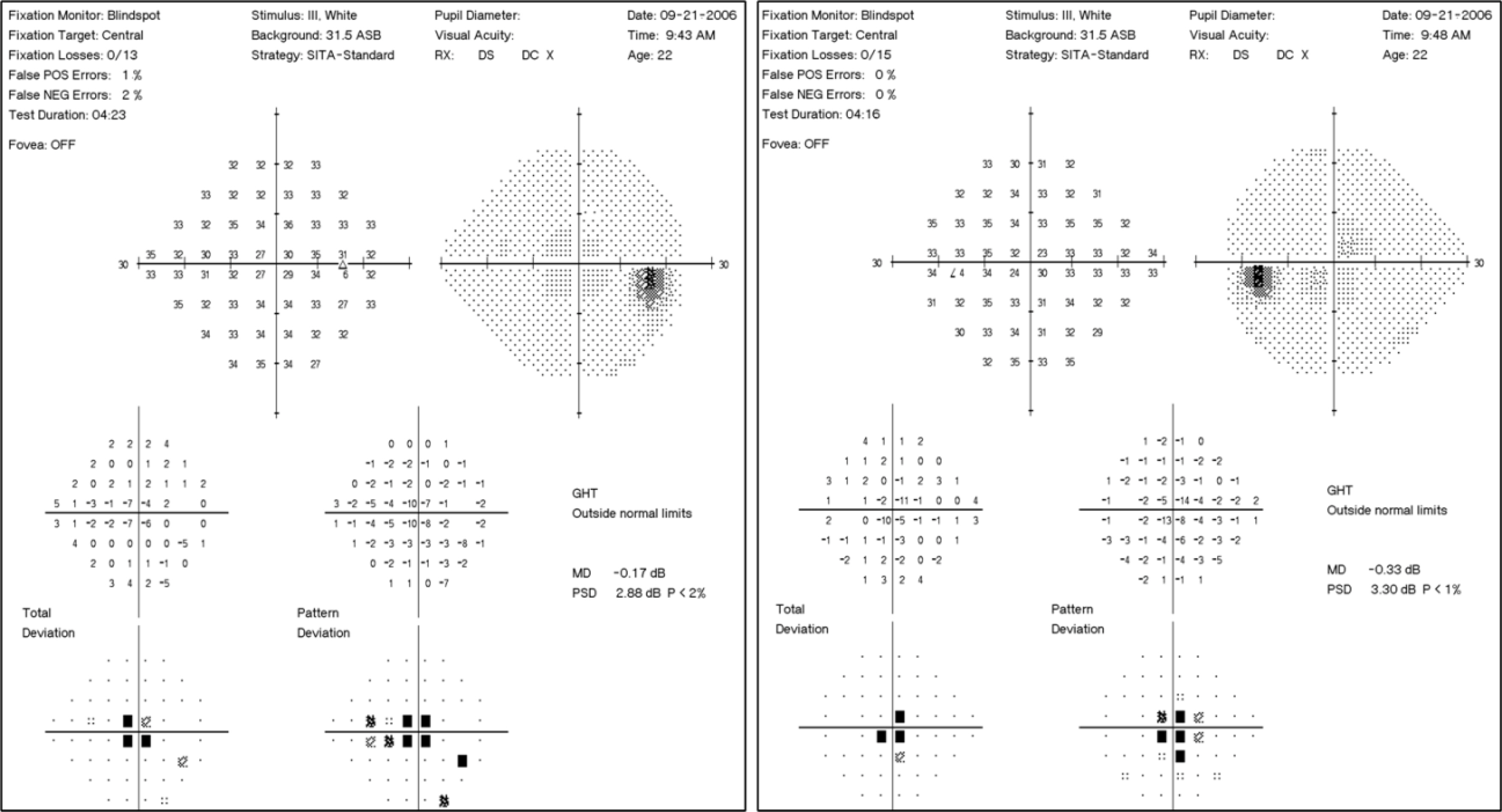
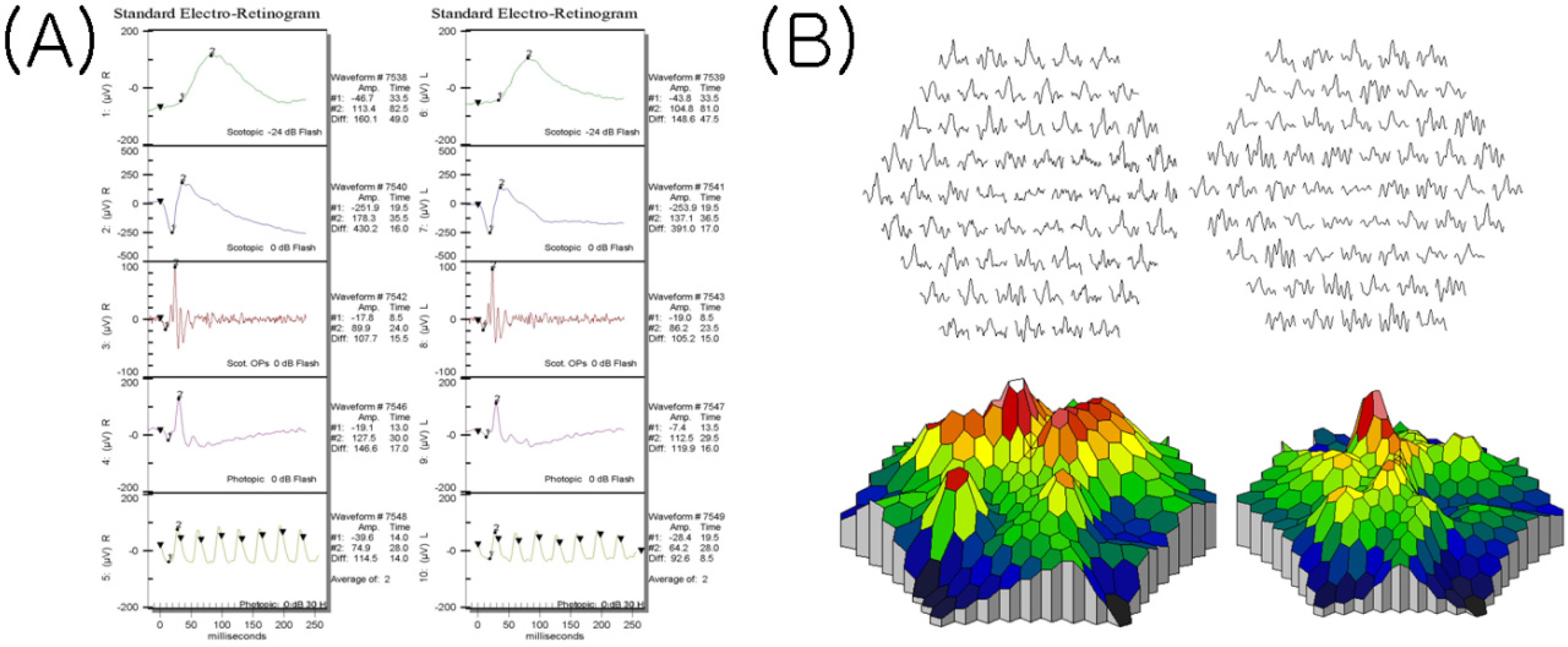
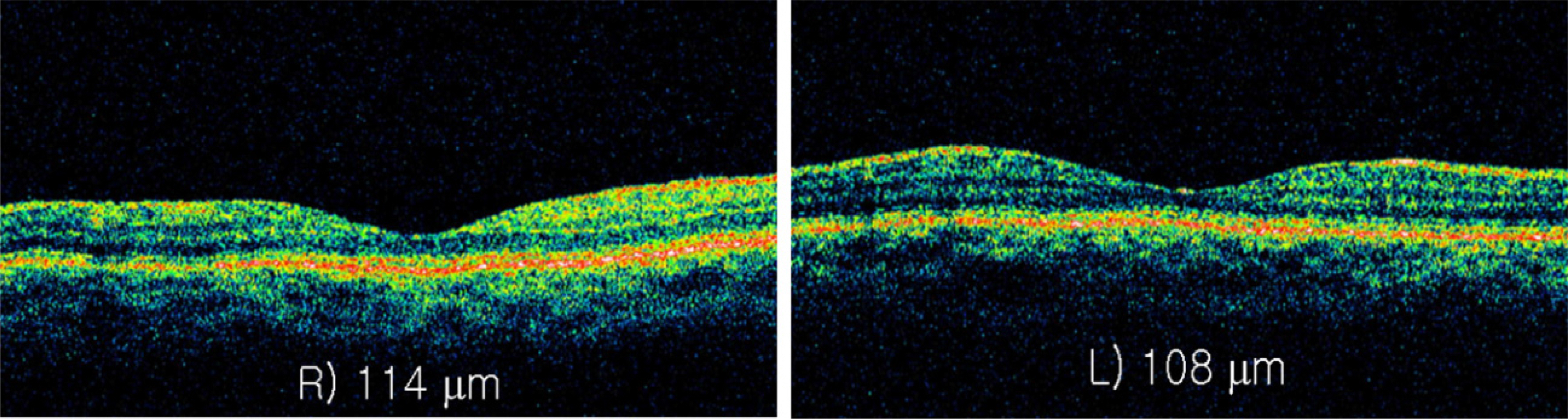
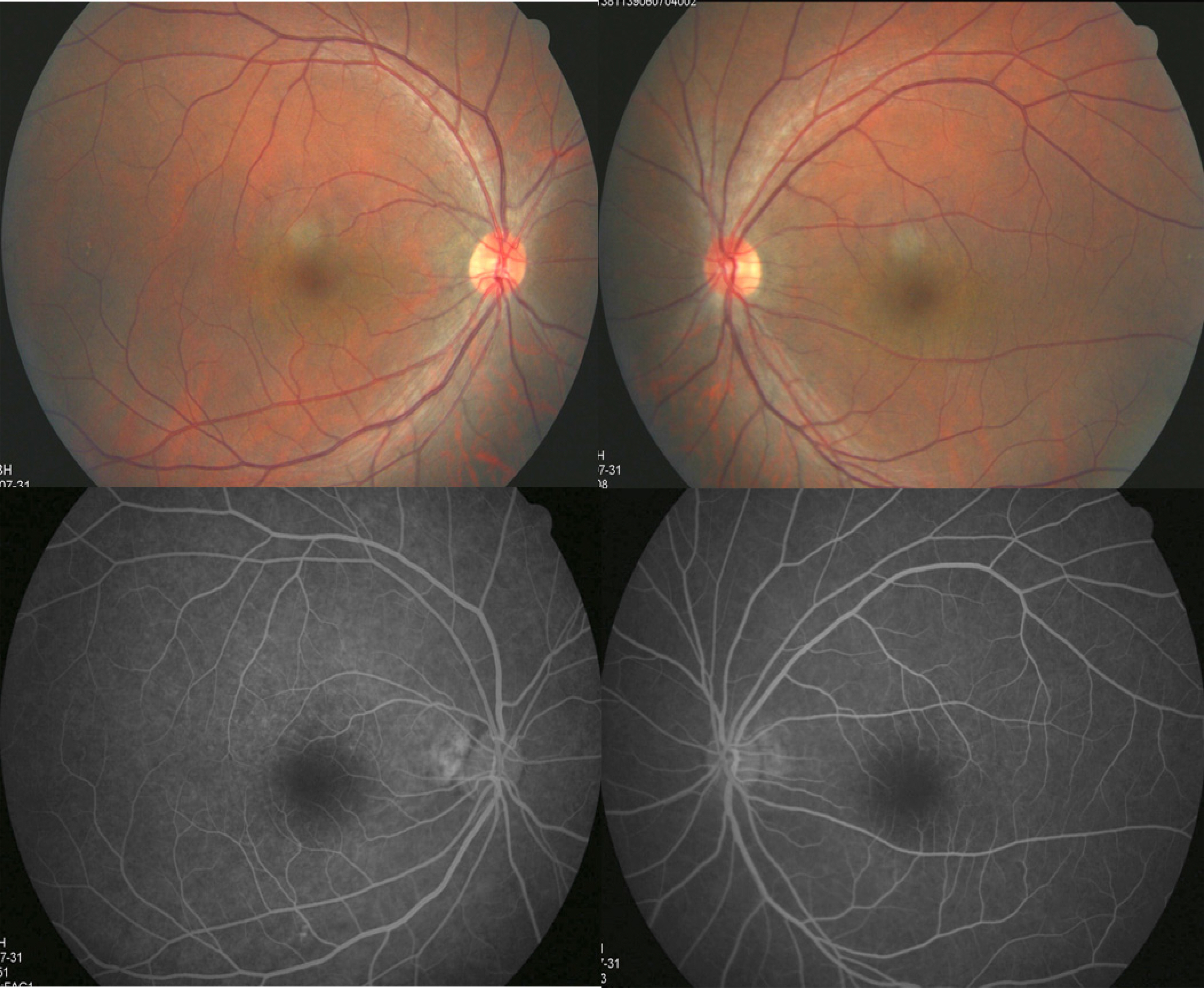
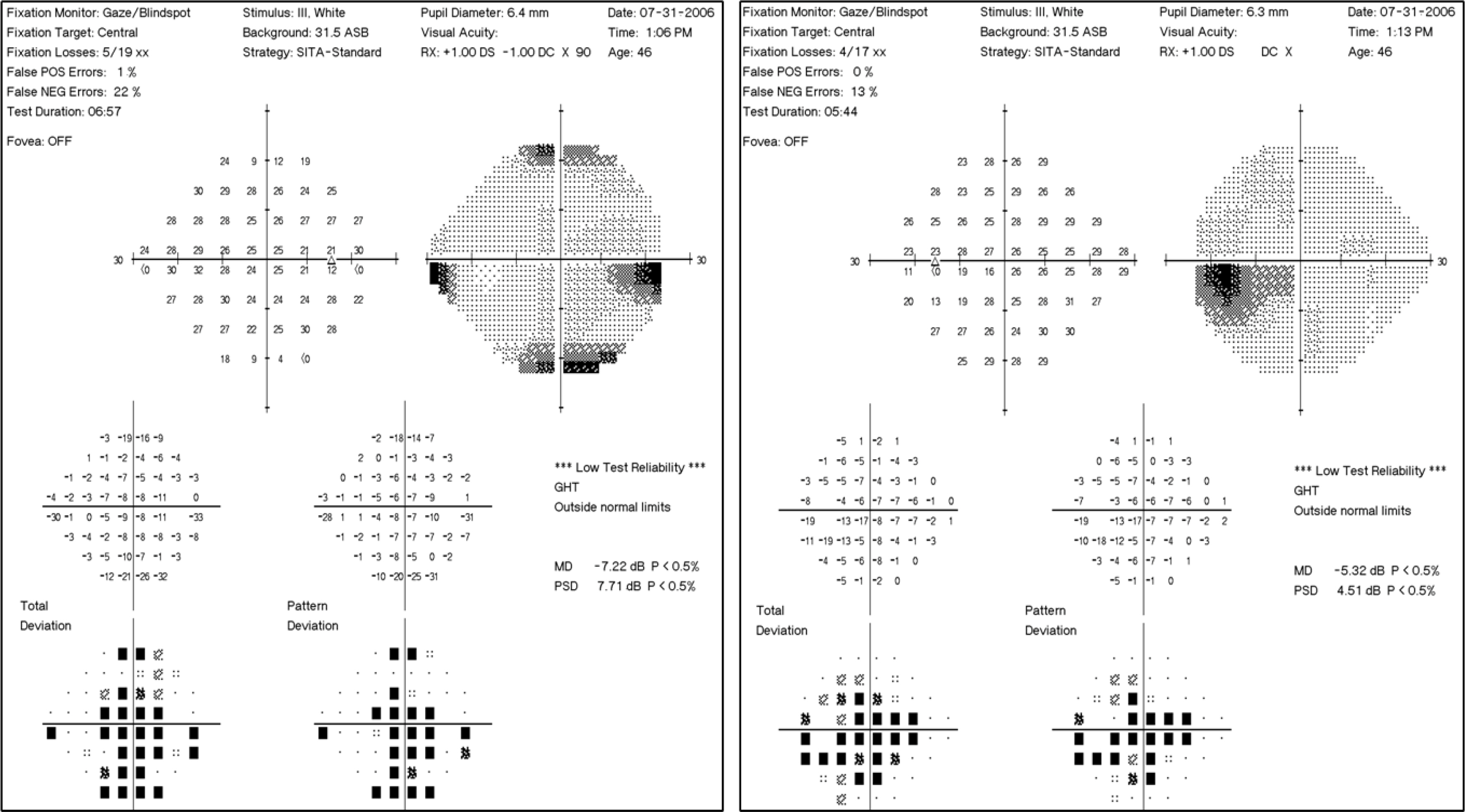
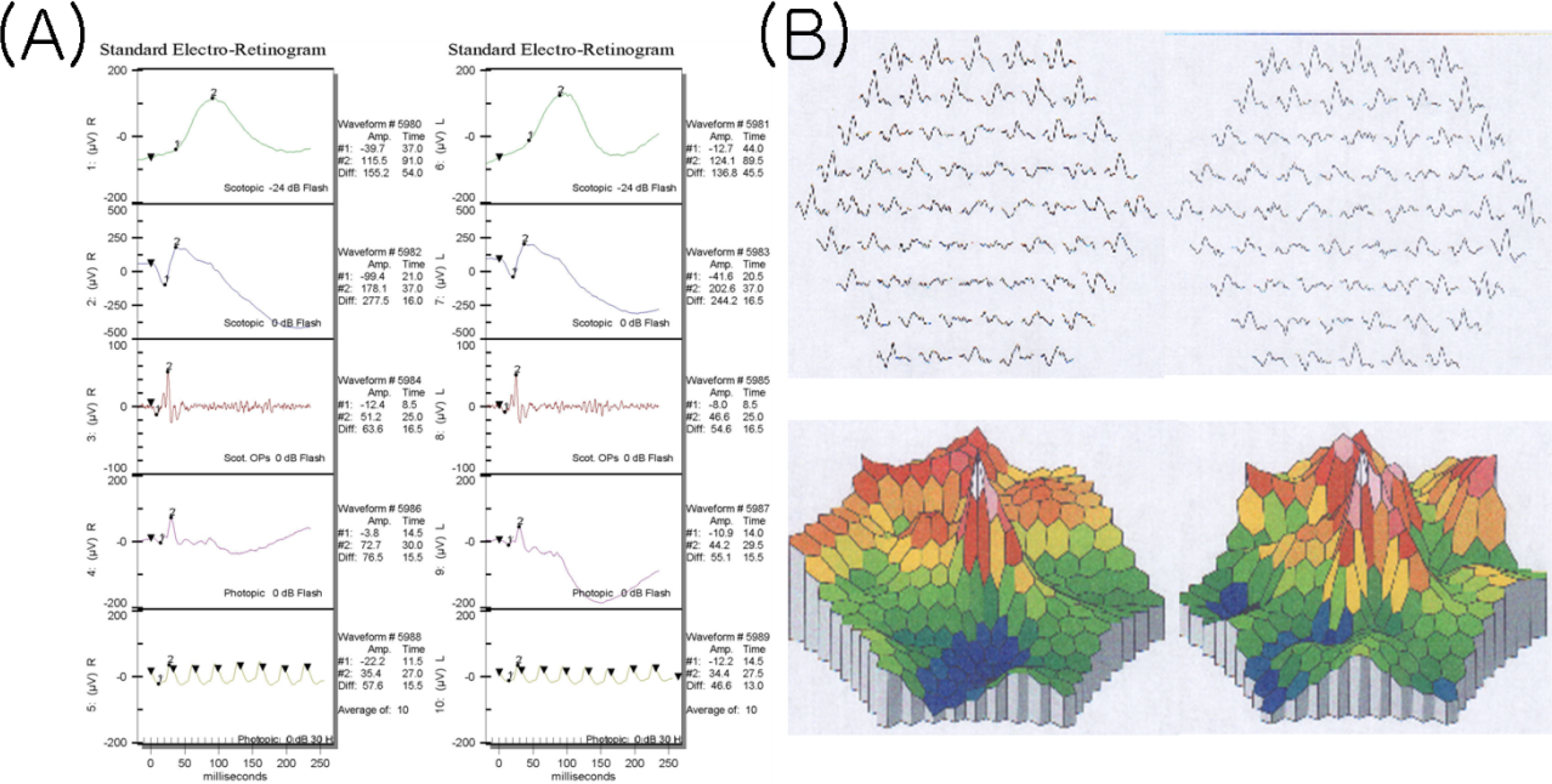
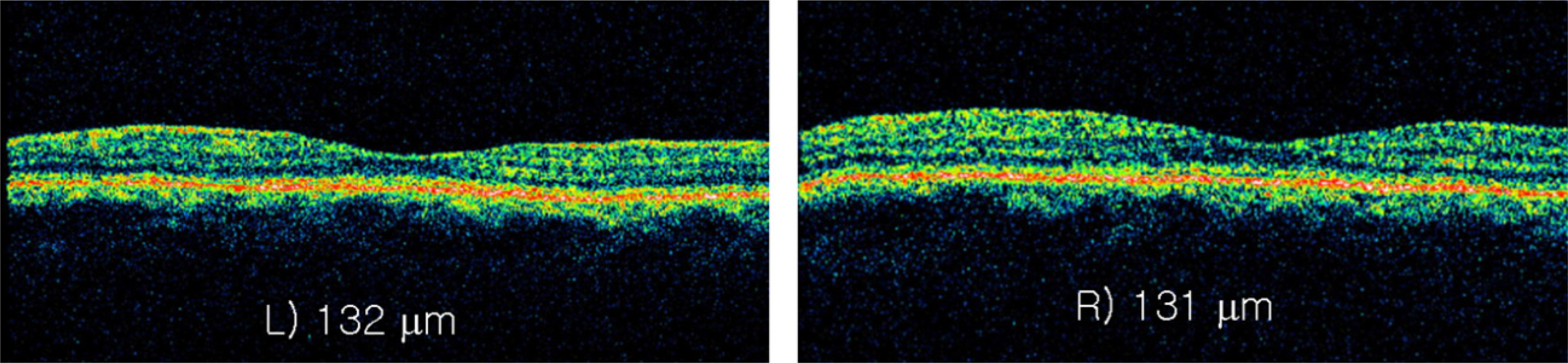
Both patients exhibited a normal ophthalmologic examination including slit lamp biomicroscope, fundus examination, fluorescein angiography, and full-field electroretinogram. However, there were central visual field defects on a Humphrey static visual field test (C 24-2) and abnormal multifocal electroretinogram (mfERG) findings affecting the central portion of the test field. Foveal thinning was also observed by optical coherence tomography images in 1 case. These findings are consistent with the clinical characteristics of occult macular dystrophy, and close observation was recommended.
CONCLUSIONS
OMD is a disease characterized by a reduction in central visual acuity without visible fundus abnormalities and full field ERG. It may be misdiagnosed as optic nerve disease, a central nervous system problem, non-organic visual disorder or malingering; therefore, mfERG is essential for the diagnosis of this rare type of macular dystrophy.
MeSH Terms
Figure
Reference
-
References
1. Miyake Y, Ichikawa K, Shiose Y, Kawase Y. Hereditary macular dystrophy without visible fundus abnormality. Am J Ophthalmol. 1989; 108:292–9.
Article2. Wildberger H, Niemeyer G, Junghardt A. Multifocal electroretinogram (mfERG) in a family with occult macular dystrophy. Klin Monatsbl Augenheilkd. 2003; 220:111–5.3. Lyons JS. Non-familial occult macular dystrophy. Doc Ophthalmol. 2005; 111:49–56.
Article4. Miyake Y, Horiguchi M, Tomita N, et al. Occult macular dystrophy. Am J Ophthalmol. 1996; 122:644–53.
Article5. Sandberg MA, Brockhurst RJ, Gaudio AR, Berson EL. The association between visual acuity and central retinal thickness in retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2005; 46:3349–54.
Article6. Kondo M, Ueno S, Piao CH, et al. Occult macular dystrophy in an 11 year old boy. Br J Ophthalmol. 2004; 88:1602–3.
Article7. Piao CH, Kondo M, Tanikawa A, et al. Multifocal electroretinogram in occult macular dystrophy. Invest Ophthalmol Vis Sci. 2000; 41:513–7.8. Kondo M, Ito Y, Ueno S, et al. Foveal thickness in occult macular dystrophy. Am J Ophthalmol. 2003; 135:725–8.
Article9. Brockhurst RJ, Sandberg MA. Optical coherence tomography findings in occult macular dystrophy. Am J Ophthalmol. 2007; 143:516–8.
Article10. Ergun E, Hermann B, Wirtitsch M, et al. Assessment of central visual function in Stargardt disease/fundus flavimaculatus with ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci. 2005; 46:310–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cases of Macular Corneal Dystrophy with a Family History
- Granular Corneal Dystrophy
- A Korean Family with an Early-Onset Autosomal Dominant Macular Dystrophy Resembling North Carolina Macular Dystrophy
- A Case of Macular Dystrophy of the Cornea
- Two Cases of Oculopharyngeal Muscular Dystrophy in One Family