J Korean Soc Radiol.
2014 Nov;71(5):249-253. 10.3348/jksr.2014.71.5.249.
Solitary Axillary Lymph Node Metastasis without Breast Involvement from Ovarian Cancer: Case Report and Brief Literature Review
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. ksj1567@hanmail.net
- 2Department of Pathology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2208794
- DOI: http://doi.org/10.3348/jksr.2014.71.5.249
Abstract
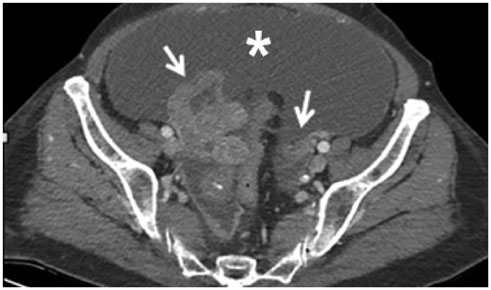
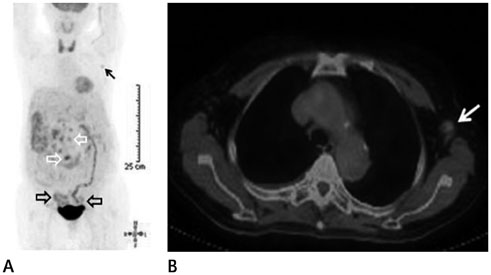
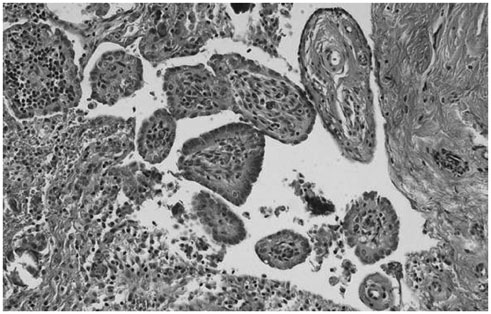
- Axillary lymph node metastasis without breast involvement from ovarian cancer is rare. We report a case of a 68-year-old woman proven as ovarian serous papillary carcinoma and metastatic papillary carcinoma of the omentum on surgical diagnostic laparoscopy. In addition, a hypermetabolic lymph node was detected in left axilla and was considered a reactive benign lesion. Mammography and ultrasonography showed no focal lesion in both breasts, but ultrasonography-guided core needle biopsy for the lymph node revealed metastatic serous papillary carcinoma from ovarian origin. Even with a low incidence of axillary lymph node metastasis without breast involvement from ovarian cancer and only marginally elevated standardized uptake value in positron emission tomography, the possibility of metastasis at axillary lymph node in patients with known primary ovarian cancer must be considered.
MeSH Terms
Figure
Reference
-
1. Recine MA, Deavers MT, Middleton LP, Silva EG, Malpica A. Serous carcinoma of the ovary and peritoneum with metastases to the breast and axillary lymph nodes: a potential pitfall. Am J Surg Pathol. 2004; 28:1646–1651.2. Aydin C, Unalp HR, Baloğlu A, Inci AG, Yiğit S, Yavuzcan A. Axillary lymph node metastasis from serous ovarian cancer: a case report and review of the literature. Arch Gynecol Obstet. 2009; 279:203–207.3. Moore DH, Wilson DK, Hurteau JA, Look KY, Stehman FB, Sutton GP. Gynecologic cancers metastatic to the breast. J Am Coll Surg. 1998; 187:178–181.4. Murray ME, Given-Wilson RM. The clinical importance of axillary lymphadenopathy detected on screening mammography. Clin Radiol. 1997; 52:458–461.5. Görkem SB, O'Connell AM. Abnormal axillary lymph nodes on negative mammograms: causes other than breast cancer. Diagn Interv Radiol. 2012; 18:473–479.6. Shetty MK, Carpenter WS. Sonographic evaluation of isolated abnormal axillary lymph nodes identified on mammograms. J Ultrasound Med. 2004; 23:63–71.7. Singer C, Blankstein E, Koenigsberg T, Mercado C, Pile-Spellman E, Smith SJ. Mammographic appearance of axillary lymph node calcification in patients with metastatic ovarian carcinoma. AJR Am J Roentgenol. 2001; 176:1437–1440.8. Lee CH, Giurescu ME, Philpotts LE, Horvath LJ, Tocino I. Clinical importance of unilaterally enlarging lymph nodes on otherwise normal mammograms. Radiology. 1997; 203:329–334.9. Lin EC, Alavi A. PET and PET/CT: A Clinical Guide. 2nd ed. New York: Thieme Medical Publishers Inc.;2005.10. Blanchard DK, Farley DR. Retrospective study of women presenting with axillary metastases from occult breast carcinoma. World J Surg. 2004; 28:535–539.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Recurrence of Ovarian Carcinoma Presenting as Only Axillary Lymphatic Metastasis: A Case Report
- Metachronous Contralateral Axillary Lymph Node Metastasis from Invasive Breast Carcinoma: A Case Report with Imaging Findings
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Ipsilateral Breast Tumor Recurrence with Metachronous Contralateral Axillary Lymph Node Metastasis after Breast-Conserving Surgery with Axillary Lymph Node Dissection
- Clinical Significance of Rotter's Nodes in Patients with Breast Carcinomas