J Korean Soc Magn Reson Med.
2014 Dec;18(4):279-289. 10.13104/jksmrm.2014.18.4.279.
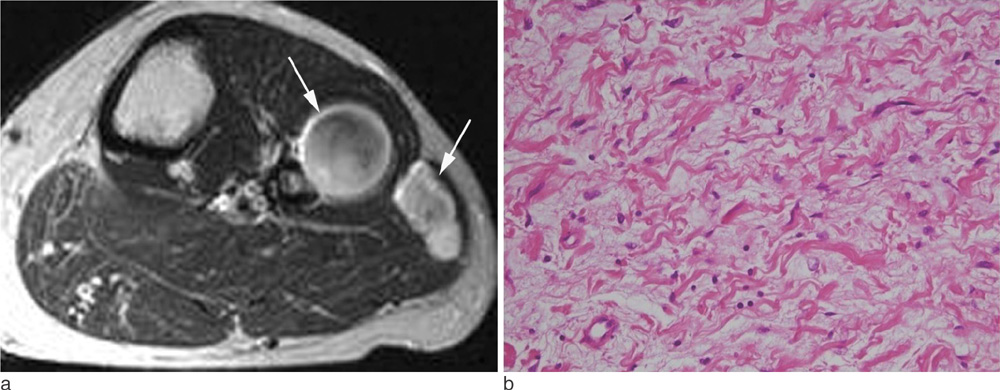
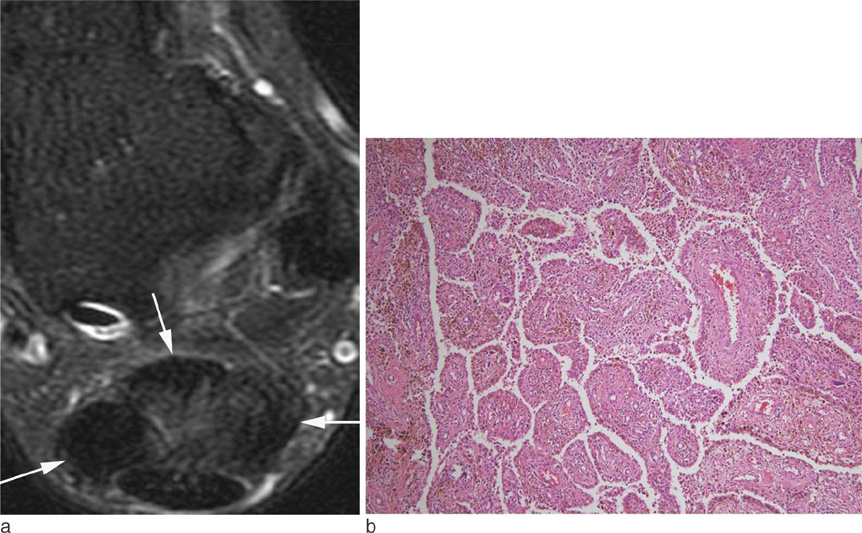
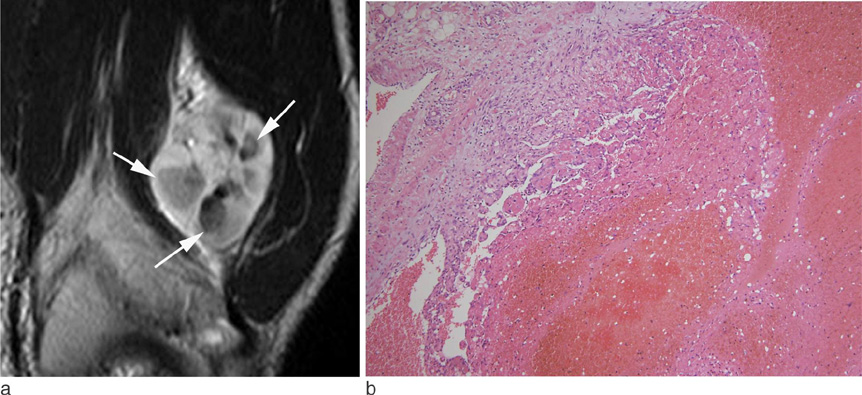
Soft Tissue Masses Showing Low Signal Intensity on T2-weighted Images: Correlation with Pathologic Findings
- Affiliations
-
- 1Department of Radiology, Pusan National University Hospital, Busan, Korea. lis@pusan.ac.kr
- 2Department of Pathology, Pusan National University Hospital, Busan, Korea.
- 3Department of Radiology, Yeungnam University Hospital, Daegu, Korea.
- 4Department of Radiology, Keimyung University School of Medicine, Dongsan Medical Center, Daegu, Korea.
- 5Department of Radiology, Catholic Universiry of Daegu Hospital, Daegu, Korea.
- 6Department of Orthopedic Surgery, Pusan National University Hospital, Busan, Korea.
- KMID: 2206925
- DOI: http://doi.org/10.13104/jksmrm.2014.18.4.279
Abstract
OBJECTIVE
The aims of this article are to differentiate soft tissue masses showing low signal intensity on T2-weighted images (T2WIs) according to the histopathologic findings.
CONCLUSION
To know relatively small numbered soft tissue masses with low signal intensities on T2WIs adding characteristic location, morphology, signal intensities on other sequences might be helpful for differential diagnosis of mostly nonspecific soft tissue tumors on MRI.
Keyword
Figure
Cited by 1 articles
-
Focal Xanthogranulomatous Pyelonephritis Associated with Xanthogranulomatous Cholecystitis: A Case Report
Soong Moon Cho, Ho Kyun Kim, Hye Kyung Lee, Byungmo Lee, Ki Hwan Kim, Kyoung Eun Lee, Jae-Chan Shim, Dae Hyun Hwang, Ghi Jai Lee
J Korean Soc Radiol. 2020;81(1):190-196. doi: 10.3348/jksr.2020.81.1.190.
Reference
-
1. Sundaram M, McGuire MH, Schajowicz F. Soft-tissue masses: histologic basis for decreased signal (short T2) on T2-weighted MR images. AJR Am J Roentgenol. 1987; 148:1247–1250.2. Sundaram M, McLeod RA. MR imaging of tumor and tumorlike lesions of bone and soft tissue. AJR Am J Roentgenol. 1990; 155:817–824.3. Hur J, Damron TA, Vermont AI, Mathur SC. Fibroma of tendon sheath of the infrapatellar fat pad. Skeletal Radiol. 1999; 28:407–410.4. Fox MG, Kransdorf MJ, Bancroft LW, Peterson JJ, Flemming DJ. MR imaging of fibroma of the tendon sheath. AJR Am J Roentgenol. 2003; 180:1449–1453.5. Wang XL, De Schepper AM, Vanhoenacker F, et al. Nodular fasciitis: correlation of MRI findings and histopathology. Skeletal Radiol. 2002; 31:155–161.6. Blacksin MF, Ha DH, Hameed M, Aisner S. Superficial softtissue masses of the extremities. Radiographics. 2006; 26:1289–1304.7. Miettinen M, Fetsch JF. Collagenous fibroma (desmoplastic fibroblastoma): a clinicopathologic analysis of 63 cases of a distinctive soft tissue lesion with stellate-shaped fibroblasts. Hum Pathol. 1998; 29:676–682.8. Robbin MR, Murphey MD, Temple HT, Kransdorf MJ, Choi JJ. Imaging of musculoskeletal fibromatosis. Radiographics. 2001; 21:585–600.9. Dinauer PA, Brixey CJ, Moncur JT, Fanburg-Smith JC, Murphey MD. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. Radiographics. 2007; 27:173–187.10. Murphey MD, Gross TM, Rosenthal HG. From the archives of the AFIP. Musculoskeletal malignant fibrous histiocytoma: radiologic-pathologic correlation. Radiographics. 1994; 14:807–826. quiz 827-828.11. Mahajan H, Kim EE, Wallace S, Abello R, Benjamin R, Evans HL. Magnetic resonance imaging of malignant fibrous histiocytoma. Magn Reson Imaging. 1989; 7:283–288.12. Kransdorf MJ, Meis JM, Montgomery E. Elastofibroma: MR and CT appearance with radiologic-pathologic correlation. AJR Am J Roentgenol. 1992; 159:575–579.13. Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple MT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999; 19:1253–1280.14. Llauger J, Palmer J, Monill JM, Franquet T, Bagué S, Rosón N. MR imaging of benign soft-tissue masses of the foot and ankle. Radiographics. 1998; 18:1481–1498.15. Hassell DS, Bancroft LW, Kransdorf MJ, et al. Imaging appearance of diffuse neurofibroma. AJR Am J Roentgenol. 2008; 190:582–588.16. Llauger J, Palmer J, Roson N, Cremades R, Baque S. Pigmented villonodular synovitis and giant cell tumors of the tendon sheath: radiologic and pathologic features. AJR Am J Roentgenol. 1999; 172:1087–1091.17. Sheldon PJ, Forrester DM, Learch TJ. Imaging of intraarticular masses. Radiographics. 2005; 25:105–119.18. Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics. 2007; 27:1465–1488.19. Kransdorf MJ, Meis JM, Jelinek JS. Myositis ossificans: MR appearance with radiologic-pathologic correlation. AJR Am J Roentgenol. 1991; 157:1243–1248.20. Parikh J, Hyare H, Saifuddin A. The imaging features of posttraumatic myositis ossificans, with emphasis on MRI. Clin Radiol. 2002; 57:1058–1066.21. De Beuckeleer LH, De Schepper AM, Neetens I. Magnetic resonance imaging of pilomatricoma. Eur Radiol. 1996; 6:72–75.22. Lee SH, Suh JS, Lim BI, Yang WI, Shin KH. Intravascular papillary endothelial hyperplasia of the extremities: MR imaging findings with pathologic correlation. Eur Radiol. 2004; 14:822–826.23. Clifford PD, Temple HT, Jorda M, Marecos E. Intravascular papillary endothelial hyperplasia (Masson's tumor) presenting as a triceps mass. Skeletal Radiol. 2004; 33:421–425.24. Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. From the archives of the AFIP. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. Radiographics. 1995; 15:893–917.25. Vilanova JC, Barcelo J, Smirniotopoulos JG, et al. Hemangioma from head to toe: MR imaging with pathologic correlation. Radiographics. 2004; 24:367–385.26. Jones BC, Sundaram M, Kransdorf MJ. Synovial sarcoma: MR imaging findings in 34 patients. AJR Am J Roentgenol. 1993; 161:827–830.27. Nakanishi K, Araki N, Yoshikawa H, Hashimoto T, Nakamura H. Alveolar soft part sarcoma. Eur Radiol. 1998; 8:813–816.28. Hong SH, Chung HW, Choi JY, Koh YH, Choi JA, Kang HS. MRI findings of subcutaneous epidermal cysts: emphasis on the presence of rupture. AJR Am J Roentgenol. 2006; 186:961–966.29. Ruzek KA, Wenger DE. The multiple faces of lymphoma of the musculoskeletal system. Skeletal Radiol. 2004; 33:1–8.30. ter Braak BP, Guit GL, Bloem JL. Case 111: Soft-tissue lymphoma. Radiology. 2007; 243:293–296.31. Boukobza M, Mazel C, Touboul E. Primary vertebral and spinal epidural non-Hodgkin's lymphoma with spinal cord compression. Neuroradiology. 1996; 38:333–337.