J Lung Cancer.
2012 Dec;11(2):97-101. 10.6058/jlc.2012.11.2.97.
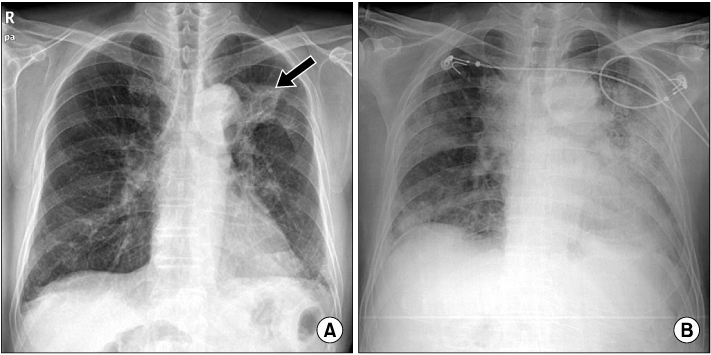
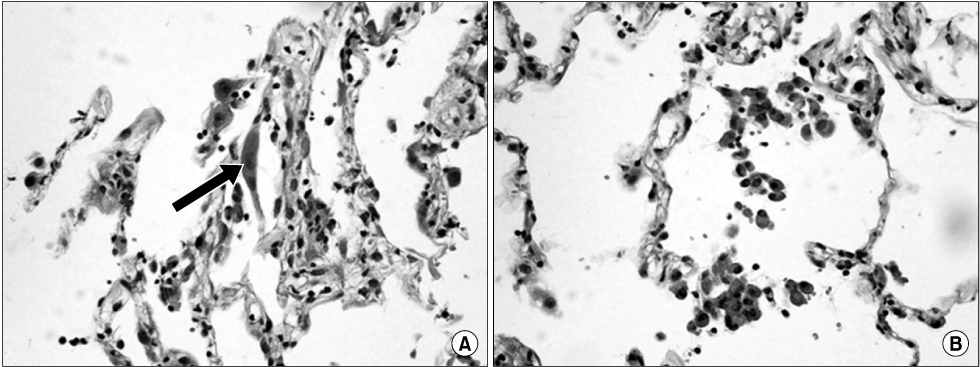
Bilateral Diffuse Radiation Pneumonitis Caused by Unilateral Thoracic Irradiation: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Cheju Halla General Hospital, Jeju, Korea. cohen71@naver.com
- 2Department of Pathology, Cheju Halla General Hospital, Jeju, Korea.
- 3Department of Radiation Oncology, Cheju Halla General Hospital, Jeju, Korea.
- KMID: 2199837
- DOI: http://doi.org/10.6058/jlc.2012.11.2.97
Abstract
- Radiation therapy is one of the most important therapeutic modalities for the treatment of lung cancer. Radiation pneumonitis is one of the important complications associated with radiotherapy for lung cancer. Radiation pneumonitis is generally limited to the irradiated lung and is manifested by the insidious onset of dry cough, dyspnea, and mild fever, resulting in damage and edematous changes of alveolar structures on histologic inspection. Clinically, diffuse bilateral radiation pneumonitis accompanied with acute symptoms after unilateral thoracic irradiation appears very rarely. Histopathologic examinations for the diagnosis of out-of-field radiation pneumonitis are rarely performed. We herein describe a case of extensive bilateral radiation pneumonitis which developed acutely after salvage radiotherapy for squamous cell carcinoma in the left upper lobe of the lung. The condition was confirmed by a diagnostic help of histopathologic findings.
Keyword
Figure
Reference
-
1. Pastores SM, Voigt LP. Acute respiratory failure in the patient with cancer: diagnostic and management strategies. Crit Care Clin. 2010. 26:21–40.
Article2. Oh YT. Radiation induced lung damage: mechanisms and clinical implications. J Lung Cancer. 2008. 7:9–18.
Article3. Morgan GW, Breit SN. Radiation and the lung: a reevaluation of the mechanisms mediating pulmonary injury. Int J Radiat Oncol Biol Phys. 1995. 31:361–369.
Article4. Hassaballa HA, Cohen ES, Khan AJ, Ali A, Bonomi P, Rubin DB. Positron emission tomography demonstrates radiation-induced changes to nonirradiated lungs in lung cancer patients treated with radiation and chemotherapy. Chest. 2005. 128:1448–1452.
Article5. Lo MK, Iupati D, Quddus Z, Carter J, Chander S. A case of sporadic radiation pneumonitis. Am J Clin Oncol. 2006. 29:643–644.
Article6. Park KJ, Chung JY, Chun MS, Suh JH. Radiation-induced lung disease and the impact of radiation methods on imaging features. Radiographics. 2000. 20:83–98.
Article7. Gross NJ. Radiation pneumonitis in mice. Some effects of corticosteroids on mortality and pulmonary physiology. J Clin Invest. 1980. 66:504–510.
Article8. Abdollahi A, Li M, Ping G, et al. Inhibition of platelet-derived growth factor signaling attenuates pulmonary fibrosis. J Exp Med. 2005. 201:925–935.
Article9. Martín C, Romero S, Sánchez-Payá J, Massuti B, Arriero JM, Hernández L. Bilateral lymphocytic alveolitis: a common reaction after unilateral thoracic irradiation. Eur Respir J. 1999. 13:727–732.
Article10. Kim TH, Cho KH, Pyo HR, et al. Dose-volumetric parameters for predicting severe radiation pneumonitis after three-dimensional conformal radiation therapy for lung cancer. Radiology. 2005. 235:208–215.
Article11. Robnett TJ, Machtay M, Vines EF, McKenna MG, Algazy KM, McKenna WG. Factors predicting severe radiation pneumonitis in patients receiving definitive chemoradiation for lung cancer. Int J Radiat Oncol Biol Phys. 2000. 48:89–94.
Article12. Yamada M, Kudoh S, Hirata K, Nakajima T, Yoshikawa J. Risk factors of pneumonitis following chemoradiotherapy for lung cancer. Eur J Cancer. 1998. 34:71–75.
Article13. Schaake-Koning C, van den Bogaert W, Dalesio O, et al. Effects of concomitant cisplatin and radiotherapy on inoperable non-small-cell lung cancer. N Engl J Med. 1992. 326:524–530.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation Induced Lung Damage : Mechanisms and Clinical Implications
- An expermental study of radiation pneumonitis
- An Experimental Study on the Radiation-induced Injury of the Rabbit Lung: Correlation of Soft-tissue Radiograph and High-Resolution CT Findings with Pathologic Findings
- The Studies on the Development of Radiation Pneumonitis and Its Related Factors
- Factors predicting radiation pneumonitis in locally advanced non-small cell lung cancer