J Korean Soc Hypertens.
2012 Dec;18(4):166-175. 10.5646/jksh.2012.18.4.166.
Influences of Dry Weight Adjustment Based on Bioimpedance Analysis on Ambulatory Blood Pressure in Hemodialysis Patients
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. shyu3cau@gmail.com
- KMID: 2196543
- DOI: http://doi.org/10.5646/jksh.2012.18.4.166
Abstract
- BACKGROUND
Hypertension is a common problem for hemodialysis patients and is associated with an increased cardiovascular mortality. We analyzed ambulatory blood pressure (ABP) in hemodialysis patients and investigated if an adjustment of dry weight can be used to control blood pressure.
METHODS
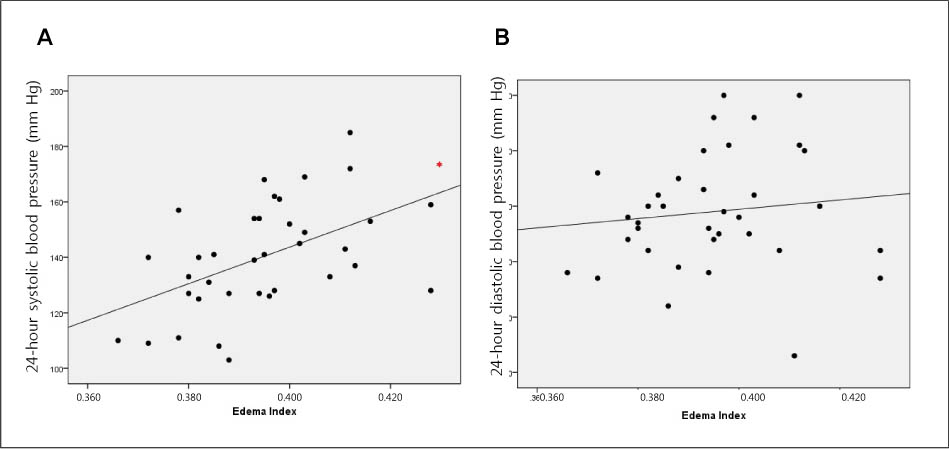
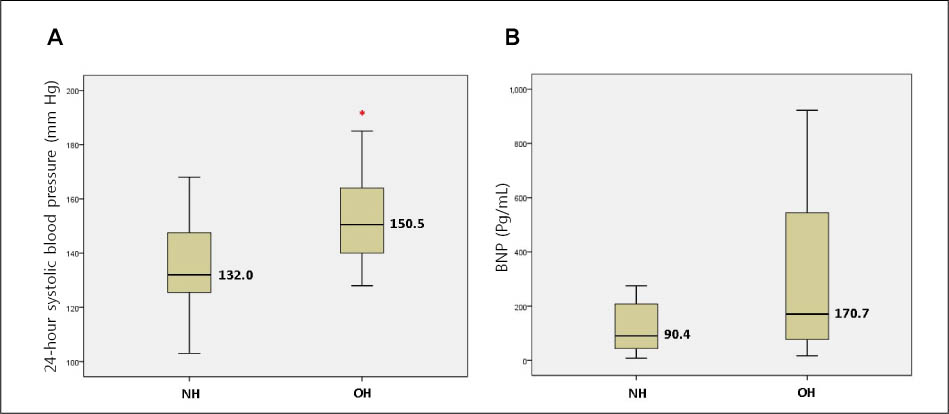
ABP was measured for twenty-four hours after hemodialysis. A bioimpedance Analysis (BIA) was conducted. Patients were divided into two groups by the edema index. A normohydration (NH) group included patients with the edema index less than 0.40, and an overhydration (OH) group included patients with the edema index 0.40 or more. We accordingly adjusted the dry weight based on BIA results.
RESULTS
Thirty-six patients were recruited, comprising twenty-two men and fourteen women. In regard to the ABP, 24-hour systolic and diastolic blood pressures were 140.2 +/- 19.7 mm Hg and 79.0 +/- 10.6 mm Hg, respectively. There was a significant association between 24-hour systolic blood pressure and the edema index (r = 0.501, p = 0.002). Twenty four-hour systolic blood pressure was significantly different between the NH and OH groups (median value, 132.0 vs. 150.5 mm Hg; p = 0.008). In OH group, after adjustment of the dry weight, the edema index was decreased from 0.411 +/- 0.009 to 0.389 +/- 0.047 and office systolic blood pressure was also decreased from 144.7 +/- 32.7 mm Hg to 125.3 +/- 15.4 mm Hg in OH group (p = 0.028 and p = 0.018, respectively).
CONCLUSIONS
The edema index obtained by the bioimpedance analysis is significantly correlated with 24-hour systolic blood pressure in hemodialysis patients. Also, an adjustment of dry weight can be used to control blood pressure in hemodialysis patients.
MeSH Terms
Figure
Cited by 1 articles
-
Utility of Volume Assessment Using Bioelectrical Impedance Analysis in Critically Ill Patients Receiving Continuous Renal Replacement Therapy: A Prospective Observational Study
Ki Hyun Park, Jung-ho Shin, Jin Ho Hwang, Su Hyun Kim
Korean J Crit Care Med. 2017;32(3):256-264. doi: 10.4266/kjccm.2017.00136.
Reference
-
1. Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003. 115:291–297.
Article2. Ihm CG. Treatment of hypertension in the patients with chronic kidney disease: focusing on the issues under debate. J Korean Soc Hypertens. 2007. 13:1–7.3. Fagard RH, Staessen JA, Thijs L, Bulpitt CJ, Clement D, de Leeuw PW, et al. Relationship between ambulatory blood pressure and follow-up clinic blood pressure in elderly patients with systolic hypertension. J Hypertens. 2004. 22:81–87.
Article4. Shimizu M, Kario K. Perfect 24-hour BP management for high-risk hypertension. J Korean Soc Hypertens. 2010. 16:1–8.5. Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006. 354:2368–2374.
Article6. Alpert MA, Huting J, Twardowski ZJ, Khanna R, Nolph KD. Continuous ambulatory peritoneal dialysis and the heart. Perit Dial Int. 1995. 15:6–11.
Article7. Gunal AI, Karaca I, Aygen B, Yavuzkir M, Dogukan A, Celiker H. Strict fluid volume control and left ventricular hypertrophy in hypertensive patients on chronic haemodialysis: a cross-sectional study. J Int Med Res. 2004. 32:70–77.
Article8. Chazot C. Managing dry weight and hypertension in dialysis patients: still a challenge for the nephrologist in 2009? J Nephrol. 2009. 22:587–597.9. Chamney PW, Kramer M, Rode C, Kleinekofort W, Wizemann V. A new technique for establishing dry weight in hemodialysis patients via whole body bioimpedance. Kidney Int. 2002. 61:2250–2258.
Article10. Wabel P, Chamney P, Moissl U, Jirka T. Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif. 2009. 27:75–80.
Article11. Mitra S, Chandna SM, Farrington K. What is hypertension in chronic haemodialysis? The role of interdialytic blood pressure monitoring. Nephrol Dial Transplant. 1999. 14:2915–2921.
Article12. Staessen JA, Asmar R, De Buyzere M, Imai Y, Parati G, Shimada K, et al. Task Force II: blood pressure measurement and cardiovascular outcome. Blood Press Monit. 2001. 6:355–370.13. Leary AC, Struthers AD, Donnan PT, MacDonald TM, Murphy MB. The morning surge in blood pressure and heart rate is dependent on levels of physical activity after waking. J Hypertens. 2002. 20:865–870.
Article14. Kikuya M, Hozawa A, Ohokubo T, Tsuji I, Michimata M, Matsubara M, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000. 36:901–906.15. Scharfetter H, Wirnsberger GH, Holzer H, Hutten H. Influence of ionic shifts during dialysis on volume estimations with multifrequency impedance analysis. Med Biol Eng Comput. 1997. 35:96–102.
Article16. Oe B, de Fijter CW, Geers TB, Vos PF, Donker AJ, de Vries PM. Diameter of inferior caval vein and impedance analysis for assessment of hydration status in peritoneal dialysis. Artif Organs. 2000. 24:575–577.17. Coresh J, Wei GL, McQuillan G, Brancati FL, Levey AS, Jones C, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: findings from the third National Health and Nutrition Examination Survey (1988-1994). Arch Intern Med. 2001. 161:1207–1216.18. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003. 289:2560–2572.
Article19. European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003. 21:1011–1053.20. Bakris GL, Williams M, Dworkin L, Elliott WJ, Epstein M, Toto R, et al. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000. 36:646–661.
Article21. Triolo L, Cattaruzza MS, Sicoli R, Ansali F, Malaguti M, Osborn J, et al. Blood pressure control and comorbidity in a nephrology clinic. J Nephrol. 2004. 17:808–812.22. Rahman M, Griffin V, Kumar A, Manzoor F, Wright JT Jr, Smith MC. A comparison of standardized versus "usual" blood pressure measurements in hemodialysis patients. Am J Kidney Dis. 2002. 39:1226–1230.
Article23. Agarwal R, Peixoto AJ, Santos SF, Zoccali C. Pre- and post-dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol. 2006. 1:389–398.
Article24. Santos SF, Mendes RB, Santos CA, Dorigo D, Peixoto AJ. Profile of interdialytic blood pressure in hemodialysis patients. Am J Nephrol. 2003. 23:96–105.
Article25. Agarwal R, Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol. 2006. 26:503–510.
Article26. Jacob P, Hartung R, Bohlender J, Stein G. Utility of 24-h ambulatory blood pressure measurement in a routine clinical setting of patients with chronic renal disease. J Hum Hypertens. 2004. 18:745–751.
Article27. Fukuda M, Mizuno M, Yamanaka T, Motokawa M, Shirasawa Y, Nishio T, et al. Patients with renal dysfunction require a longer duration until blood pressure dips during the night. Hypertension. 2008. 52:1155–1160.
Article28. Bankir L, Bochud M, Maillard M, Bovet P, Gabriel A, Burnier M. Nighttime blood pressure and nocturnal dipping are associated with daytime urinary sodium excretion in African subjects. Hypertension. 2008. 51:891–898.
Article29. Fagugli RM, Reboldi G, Quintaliani G, Pasini P, Ciao G, Cicconi B, et al. Short daily hemodialysis: blood pressure control and left ventricular mass reduction in hypertensive hemodialysis patients. Am J Kidney Dis. 2001. 38:371–376.
Article30. Sherwood A, Steffen PR, Blumenthal JA, Kuhn C, Hinderliter AL. Nighttime blood pressure dipping: the role of the sympathetic nervous system. Am J Hypertens. 2002. 15(2 Pt 1):111–118.
Article31. Ishikawa J, Shimizu M, Hoshide S, Eguchi K, Pickering TG, Shimada K, et al. Cardiovascular risks of dipping status and chronic kidney disease in elderly Japanese hypertensive patients. J Clin Hypertens (Greenwich). 2008. 10:787–794.
Article32. Agarwal R, Kariyanna SS, Light RP. Circadian blood pressure classification scheme and the health of patients with chronic kidney disease. Am J Nephrol. 2009. 30:536–546.
Article33. Mizuno M, Fukuda M, Miura T, Wakamatsu T, Naito T, Sato R, et al. Morning hypertension in chronic kidney disease is sustained type, but not surge type. Blood Press Monit. 2012. 17:20–23.
Article34. Rothwell PM, Howard SC, Dolan E, O'Brien E, Dobson JE, Dahlof B, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010. 375:895–905.
Article35. Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010. 375:938–948.
Article36. Webb AJ, Rothwell PM. Blood pressure variability and risk of new-onset atrial fibrillation: a systematic review of randomized trials of antihypertensive drugs. Stroke. 2010. 41:2091–2093.37. Mitsuhashi H, Tamura K, Yamauchi J, Ozawa M, Yanagi M, Dejima T, et al. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis. 2009. 207:186–190.
Article38. Murashima M, Kumar D, Doyle AM, Glickman JD. Comparison of intradialytic blood pressure variability between conventional thrice-weekly hemodialysis and short daily hemodialysis. Hemodial Int. 2010. 14:270–277.
Article39. Di Iorio B, Pota A, Sirico ML, Torraca S, Di Micco L, Rubino R, et al. Blood pressure variability and outcomes in chronic kidney disease. Nephrol Dial Transplant. 2012. 27:4404–4410.
Article40. Wittke E, Fuchs SC, Fuchs FD, Moreira LB, Ferlin E, Cichelero FT, et al. Association between different measurements of blood pressure variability by ABP monitoring and ankle-brachial index. BMC Cardiovasc Disord. 2010. 10:55.
Article41. Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB. Relation of blood pressure variability to carotid atherosclerosis and carotid artery and left ventricular hypertrophy. Arterioscler Thromb Vasc Biol. 2001. 21:1507–1511.
Article42. Dionisio P, Valenti M, Bergia R, Caramello E, Stramignoni E, Berto IM, et al. Influence of the hydration state on blood pressure values in a group of patients on regular maintenance hemodialysis. Blood Purif. 1997. 15:25–33.
Article43. Fishbane S, Natke E, Maesaka JK. Role of volume overload in dialysis-refractory hypertension. Am J Kidney Dis. 1996. 28:257–261.
Article44. Kooman JP, Leunissen KM. Cardiovascular aspects in renal disease. Curr Opin Nephrol Hypertens. 1993. 2:791–797.
Article45. Mehta BR, Ireland MA, Shiu MF. Echocardiographic evaluation of cardiac size and function in dialysis patients. Clin Nephrol. 1983. 20:61–66.46. Chazot C, Charra B, Vo Van C, Jean G, Vanel T, Calemard E, et al. The Janus-faced aspect of 'dry weight'. Nephrol Dial Transplant. 1999. 14:121–124.
Article47. Ifudu O. The concept of "dry weight" in maintenance hemodialysis: flaws in clinical application. Int J Artif Organs. 1996. 19:384–386.
Article48. Sinha AD. Why assistive technology is needed for probing of dry weight. Blood Purif. 2011. 31:197–202.
Article49. Cataliotti A, Malatino LS, Jougasaki M, Zoccali C, Castellino P, Giacone G, et al. Circulating natriuretic peptide concentrations in patients with end-stage renal disease: role of brain natriuretic peptide as a biomarker for ventricular remodeling. Mayo Clin Proc. 2001. 76:1111–1119.
Article50. Um HJ, Kim H, Park EM, Park JS, Lee KB. Assessment of dry body weight in maintenance hemodialysis patients by plasma levels of ANP and cGMP. Korean J Nephrol. 2001. 20:51–58.51. Natori H, Tamaki S, Kira S. Ultrasonographic evaluation of ventilatory effect on inferior vena caval configuration. Am Rev Respir Dis. 1979. 120:421–427.52. Lee SW. Determination of dry weight in hemodialysis patients. Korean J Nephrol. 2008. 27:412–415.53. Kotanko P, Levin NW, Zhu F. Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant. 2008. 23:808–812.
Article54. Agarwal R. Role of home blood pressure monitoring in hemodialysis patients. Am J Kidney Dis. 1999. 33:682–687.
Article55. Luo YJ, Lu XH, Woods F, Wang T. Volume control in peritoneal dialysis patients guided by bioimpedance spectroscopy assessment. Blood Purif. 2011. 31:296–302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraocular Pressure Change by the Hemodialysis
- Clinical usefulness of bioimpedance analysis for assessing volume status in patients receiving maintenance dialysis
- Assessment of Fluid Shifts of Body Compartments using Both Bioimpedance Analysis and Blood Volume Monitoring
- A Comparison of Techniques in Assessment of Postdialysis Dry Weight: The Relationship Between Biochemical Markers(ANP and cGMP) and Multifrequency Bioelectric Impedance
- Assessment of Dry Body Weight in Maintenance Hemodialysis Patients by Plasma Levels of ANP and cGMP