J Korean Neurosurg Soc.
2015 Jun;57(6):465-468. 10.3340/jkns.2015.57.6.465.
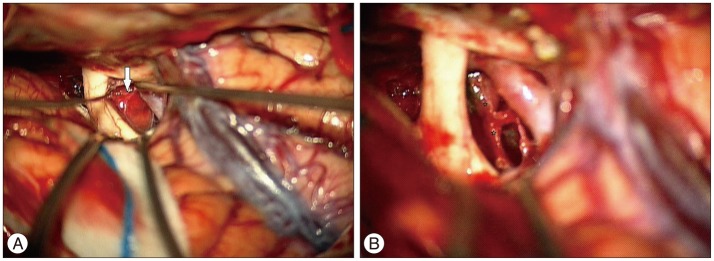
Sporadic Hemangioblastoma in the Pituitary Stalk: A Case Report and Review of the Literature
- Affiliations
-
- 1Department of Neurosurgery, Hanyang University Guri Hospital, Guri, Korea. kjm2323@hanyang.ac.kr
- KMID: 2191256
- DOI: http://doi.org/10.3340/jkns.2015.57.6.465
Abstract
- Hemangioblastomas in the pituitary stalk are especially rare. Most pituitary stalk hemangioblastomas reported in the literature were associated with von Hippel-Lindau (VHL) disease. Here, we report only the 3rd case of sporadic pituitary stalk hemangioblastoma diagnosed in a 60-year-old woman. Despite the danger of potential complications due to excessive vascularity or proximity to important neural structures, the tumor in our case was successfully removed while preserving pituitary function. In this case, complete surgical excision was shown to be an effective treatment option for symptomatic pituitary stalk hemangioblastoma, and we suggest careful evaluation of any highly enhancing mass with a signal void in the pituitary stalk preoperatively, even if no VHL disease is evident.
Keyword
Figure
Cited by 1 articles
-
A Case of Sporadic Suprasellar Hemangioblastoma Mimicking Meningioma
Byung-moo Kang, Sang Min Youn
Brain Tumor Res Treat. 2019;7(2):147-150. doi: 10.14791/btrt.2019.7.e40.
Reference
-
1. Bachmann K, Markwalder R, Seiler RW. Supratentorial haemangioblastoma. Case report. Acta Neurochir (Wien). 1978; 44:173–177. PMID: 570343.2. Cao Y, Gao P, Wang S, Zhao J. Pituitary infundibulum hemangioblastoma detected by dynamic enhancement MRI. Can J Neurol Sci. 2010; 37:697–699. PMID: 21059523.
Article3. Chandler HC Jr, Friedman WA. Radiosurgical treatment of a hemangioblastoma : case report. Neurosurgery. 1994; 34:353–355. discussion 355PMID: 8177399.4. Ding XH, Zhou LF, Tan YZ, Zhao Y, Zhu JJ. Histologic and histogenetic investigations of intracranial hemangioblastomas. Surg Neurol. 2007; 67:239–245. discussion 245PMID: 17320626.
Article5. Fomekong E, Hernalsteen D, Godfraind C, D'Haens J, Raftopoulos C. Pituitary stalk hemangioblastoma : the fourth case report and review of the literature. Clin Neurol Neurosurg. 2007; 109:292–298. PMID: 17187928.
Article6. Goto T, Nishi T, Kunitoku N, Yamamoto K, Kitamura I, Takeshima H, et al. Suprasellar hemangioblastoma in a patient with von Hippel-Lindau disease confirmed by germline mutation study : case report and review of the literature. Surg Neurol. 2001; 56:22–26. PMID: 11546565.
Article7. Grisoli F, Gambarelli D, Raybaud C, Guibout M, Leclercq T. Suprasellar hemangioblastoma. Surg Neurol. 1984; 22:257–262. PMID: 6540482.
Article8. Hoff JT, Ray BS. Cerebral hemangioblastoma occurring in a patient with von Hippel-Lindau disease. Case report. J Neurosurg. 1968; 28:365–368. PMID: 5643929.
Article9. Lee KM, Kim EJ, Choi WS, Kim TS. Pituitary stalk hemangioblastoma in a von Hippel-Lindau patient : clinical course follow-up over a 20-year period. J Korean Neurosurg Soc. 2013; 53:297–299. PMID: 23908704.
Article10. Lonser RR, Butman JA, Kiringoda R, Song D, Oldfield EH. Pituitary stalk hemangioblastomas in von Hippel-Lindau disease. J Neurosurg. 2009; 110:350–353. PMID: 18834262.
Article11. Neumann HP, Eggert HR, Weigel K, Friedburg H, Wiestler OD, Schollmeyer P. Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel-Lindau syndrome. J Neurosurg. 1989; 70:24–30. PMID: 2909683.12. Neumann HP, Wiestler OD. Clustering of features of von Hippel-Lindau syndrome : evidence for a complex genetic locus. Lancet. 1991; 337:1052–1054. PMID: 1673491.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Hemangioblastoma in the Pituitary Stalk: An Extremely Rare Case
- Pituitary Stalk Hemangioblastoma in a von Hippel-Lindau Patient : Clinical Course Follow-Up Over a 20-Year Period
- Pituitary Adenoma Confined Within the Pituitary Stalk: A Case Report and Literature Review
- Neurocysticercosis Involving the Pituitary Stalk : Case Report and Literature Review
- Pituitary Stalk Transection Syndrome