J Korean Neurosurg Soc.
2013 Sep;54(3):225-231. 10.3340/jkns.2013.54.3.225.
Analysis of Risk Factors and Management of Cerebrospinal Fluid Morbidity in the Treatment of Spinal Dysraphism
- Affiliations
-
- 1Department of Neurosurgery, Inje University Ilsan Paik Hospital, College of Medicine, Goyang, Korea. mjsohn@paik.ac.kr
- 2Department of Family Medicine, Inje Univeristy Seoul Paik Hospital, College of Medicine, Seoul, Korea.
- 3Bagram Korean Hospital, Bagram Airfield, Afghanistan.
- KMID: 2190902
- DOI: http://doi.org/10.3340/jkns.2013.54.3.225
Abstract
OBJECTIVE
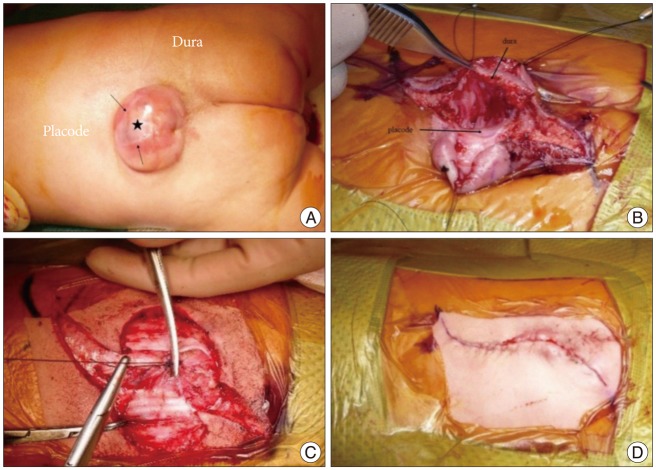
Spinal dysraphism defects span wide spectrum. Wound dehiscence is a common postoperative complication, and is a challenge in the current management of cerebrospinal fluid (CSF) leaks and wound healing. The purpose of this study is to evaluate the risks of CSF-related morbidity in the surgical treatment of spinal dysraphism.
METHODS
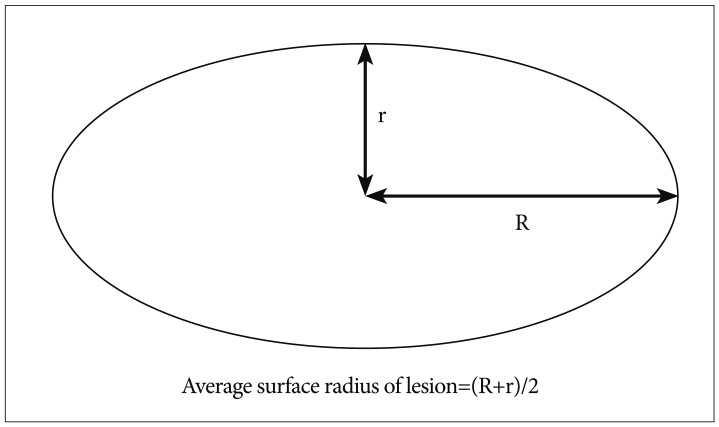
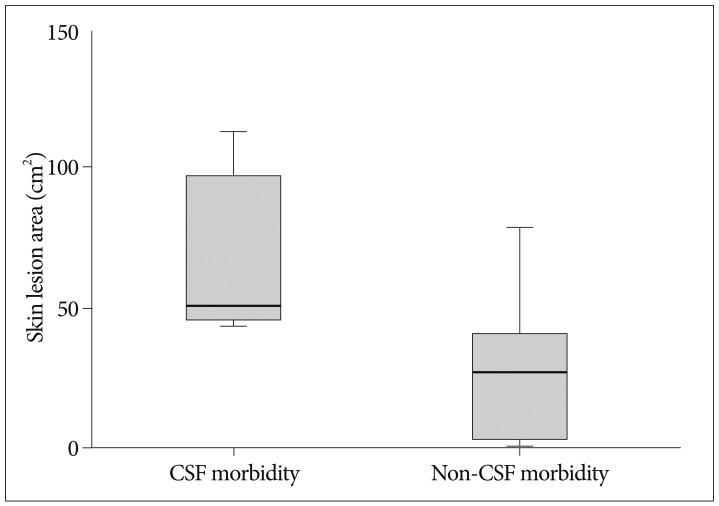
Ten patients with spinal dysraphism were included in this retrospective study. The median age of the cohort was 4.8 months. To assess the risk of CSF morbidity, we measured the skin lesion area and the percentage of the skin lesion area relative to the back surface for each patient. We then analyzed the relationship between morbidity and the measured skin lesion area or related factors.
RESULTS
The overall median skin lesion area was 36.2 cm2 (n=10). The percentage of the skin lesion area relative to the back surface ranged from 0.6% to 18.1%. During surgical reconstruction, 4 patients required subsequent operations to repair CSF morbidity. The comparison of the mean area of skin lesions between the CSF morbidity group and the non-CSF morbidity group was statistically significant (average volume skin lesion of 64.4+/-32.5 cm2 versus 27.7+/-27.8 cm2, p<0.05). CSF morbidity tended to occur either when the skin lesion area was up to 44.2 cm2 or there was preexisting fibrosis before revision with an accompanying broad-based dural defect.
CONCLUSION
Measuring the lesion area, including the skin, dura, and related surgical parameters, offers useful information for predicting wound challenges and selecting appropriate reconstructive surgery methods.
Keyword
MeSH Terms
Figure
Reference
-
1. Adzick NS, Thom EA, Spong CY, Brock JW 3rd, Burrows PK, Johnson MP, et al. A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med. 2011; 364:993–1004. PMID: 21306277.
Article2. Bowman RM, Boshnjaku V, McLone DG. The changing incidence of myelomeningocele and its impact on pediatric neurosurgery : a review from the Children's Memorial Hospital. Childs Nerv Syst. 2009; 25:801–806. PMID: 19326126.
Article3. Chapman PH, Davis KR. Surgical treatment of spinal lipomas in childhood. Pediatr Neurosurg. 1993; 19:267–275. discussion 274-274. PMID: 8398852.
Article4. Ghozlan NA, Eisa AM. Reconstruction of broad-based myelomeningocele defects : a modified technique. Egypt J Plast Reconstr Surg. 2007; 31:213–219.5. Kim P, Kim HJ. S-plasty--clinical applications for skin surgery. Aust Fam Physician. 2011; 40:224–225. PMID: 21597534.6. La Marca F, Grant JA, Tomita T, McLone DG. Spinal lipomas in children : outcome of 270 procedures. Pediatr Neurosurg. 1997; 26:8–16. PMID: 9361112.
Article7. Müller F, O'Rahilly R. The development of the human brain, the closure of the caudal neuropore, and the beginning of secondary neurulation at stage 12. Anat Embryol (Berl). 1987; 176:413–430. PMID: 3688450.
Article8. Narotam PK, José S, Nathoo N, Taylon C, Vora Y. Collagen matrix (DuraGen) in dural repair : analysis of a new modified technique. Spine (Phila Pa 1976). 2004; 29:2861–2867. discussion 2868-2869. PMID: 15599291.
Article9. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode : part I-surgical technique. Neurosurgery. 2009; 65:511–528. discussion 528-529. PMID: 19687697.10. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II : outcome analysis and preoperative profiling. Neurosurgery. 2010; 66:253–272. discussion 272-273. PMID: 20042988.11. Quiñones-Hinojosa A, Schmidek HH. Schmidek & Sweet operative neurosurgical techniques : indications, methods, and results. Philadelphia, PA: Elsevier/Saunders;2012.12. Rossi A, Cama A, Piatelli G, Ravegnani M, Biancheri R, Tortori-Donati P. Spinal dysraphism : MR imaging rationale. J Neuroradiol. 2004; 31:3–24. PMID: 15026728.13. Salam GA, Amin JP. The basic Z-plasty. Am Fam Physician. 2003; 67:2329–2332. PMID: 12800961.14. Sebastian S, Bang RH, Padilla RS. A simple approach to the S-plasty in cutaneous surgery. Dermatol Surg. 2009; 35:1277–1279. PMID: 19469794.
Article15. Siasios J, Kapsalaki EZ, Fountas KN. Surgical management of patients with Chiari I malformation. Int J Pediatr. 2012; 2012:640127. PMID: 22811732.
Article16. Spears CP. Volume doubling measurement of spherical and ellipsoidal tumors. Med Pediatr Oncol. 1984; 12:212–217. PMID: 6727778.
Article17. Turhan Haktanir N, Eser O, Demir Y, Aslan A, Köken R, Melek H. Repair of wide myelomeningocele defects with the bilateral fasciocutaneous flap method. Turk Neurosurg. 2008; 18:311–315. PMID: 18814125.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Dysraphism and Tethered Cord Syndrome
- Intramedullary Spinal Cord Lipoma without Spinal Dysraphism
- Subarachnoid Hemorrhage Presenting with Seizure due to Cerebrospinal Fluid Leakage after Spinal Surgery
- Superior mediastinal widening from traumatic cerebrospinal fluid leak with spinal fracture
- Endoscopic Management of Cerebrospinal Fluid Rhinorrhea