J Korean Neurosurg Soc.
2013 Jun;53(6):380-382. 10.3340/jkns.2013.53.6.380.
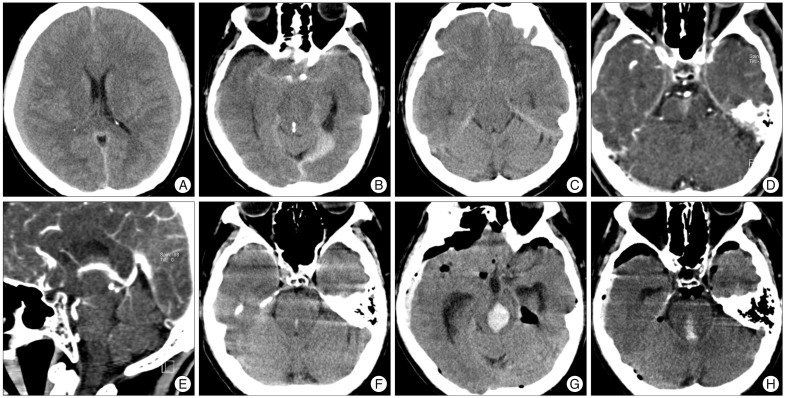
Precedence of Parenchymal Enhancement on CT Angiography to a Fatal Duret Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Jeju National University College of Medicine, Jeju, Korea.
- 2Human Medical Imaging and Intervention Center, Seoul, Korea.
- 3Department of Radiology, Jeju National University College of Medicine, Jeju, Korea. jkcontrast@naver.com
- KMID: 2190830
- DOI: http://doi.org/10.3340/jkns.2013.53.6.380
Abstract
- We report a case of fatal duret hemorrhage (DH) in a patient with acute tentorial subdural hematoma and bilateral chronic subdural hematoma along the cerebral hemispheres. Preoperative CT angiography (CTA) revealed prominent parenchymal enhancement in the ventral pontomesencephalic area. After burr-hole drainage, a large hemorrhage developed in this area. The parenchymal enhancement in the CTA may reflect the pontomensencephalic perforating vessel injury, and may be a sign of impending DH of acute transtentorial downward herniation. Previous use of aspirin and warfarin might have potentiated the process of DH and increase the extent of the bleed.
Keyword
MeSH Terms
Figure
Reference
-
1. Friede RL, Roessmann U. The pathogenesis of secondary midbrain hemorrhages. Neurology. 1966; 16:1210–1216. PMID: 5951398.
Article2. Gean AD. Imaging of head trauma. New York: Raven Press;1994. p. 211–215.3. Hjort N, Wu O, Ashkanian M, Sølling C, Mouridsen K, Christensen S, et al. MRI detection of early blood-brain barrier disruption : parenchymal enhancement predicts focal hemorrhagic transformation after thrombolysis. Stroke. 2008; 39:1025–1028. PMID: 18258832.
Article4. Johnson RT, Yates PO. Brain stem haemorrhages in expanding supratentorial conditions. Acta radiol. 1956; 46:250–256. PMID: 13361934.
Article5. Kim EY, Na DG, Kim SS, Lee KH, Ryoo JW, Kim HK. Prediction of hemorrhagic transformation in acute ischemic stroke : role of diffusion-weighted imaging and early parenchymal enhancement. AJNR Am J Neuroradiol. 2005; 26:1050–1055. PMID: 15891158.6. Klintworth GK. The pathogenesis of secondary brainstem hemorrhages as studied in an experimental model. Am J Pathol. 1965; 47:525–536. PMID: 5837730.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pontine Hemorrhage after Surgical Evacuation of Nontraumatic Subdural Hematoma
- Concept Analysis of Comfort
- Computed tomographic findings in posterior cranial fossa tumors: correlation between angiographic vascularityand CT enhancement
- Fatal Brain Herniation in Bilateral Chronic Subdural Hematoma
- Wedge-shaped Parenc hymal Enhancement Peripheral to the Hepatic Hemangioma: Two-phase Spiral CT Findings