J Korean Med Assoc.
2011 Jun;54(6):604-616. 10.5124/jkma.2011.54.6.604.
Perspectives on reconstructive microsurgery in Korea
- Affiliations
-
- 1Department of Plastic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. supramicro@gmail.com
- KMID: 2190742
- DOI: http://doi.org/10.5124/jkma.2011.54.6.604
Abstract
- With the advancement of modern medicine, there have been increasing demands for reconstructive surgeries. The operative technique using free flaps makes it possible for reconstructive surgeons to restore various defects and deformities more precisely. Furthermore, functional problems, such as facial paralysis and lymphedema, can be managed with microsurgical procedures. The need for the composite tissue allograft, including that of the face, has been noticed, and this transplantation surgery required complex microsurgical procedures. With the very high success rate of free flap and popularization of perforator flap, which provides improved outcomes, reconstructive microsurgeons now play major role in various reconstructive fields.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Soft Tissue Reconstruction for Open Tibia Fractures
Young-Woo Kim, Ho-Youn Park, Yoo-Joon Sur
Arch Hand Microsurg. 2020;25(3):207-218. doi: 10.12790/ahm.20.0037.History and Recent Advances in Microsurgery
Hyokyung Yoo, Byung Jun Kim
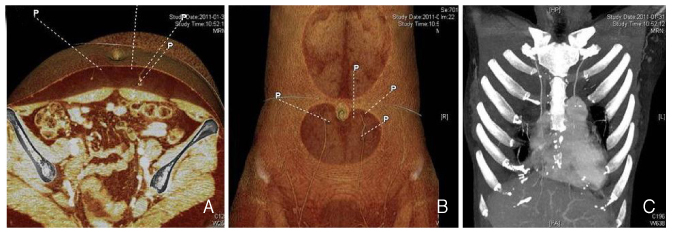
Arch Hand Microsurg. 2021;26(3):174-183. doi: 10.12790/ahm.21.0097.
Reference
-
1. Chung CN. Clinical observation on skin graft and flap. J Korean Soc Plast Reconstr Surg. 1974. 1:23–39.2. Lim P, Cho MJ, Cho HS, Hur E, Lee JW, Ham KS. An axillary scar contracture corrected by microvascular free groin flap transfer. J Korean Soc Plast Reconstr Surg. 1978. 5:189–194.3. Park CG, Lee HW, Kim CH. Microvascular free flaps for the reconstruction of head and neck. J Korean Soc Plast Reconstr Surg. 1985. 12:187–198.4. Choi SH, Hong SH, Na SK, Park CS. Clinical experiences of dorsalis pedis free flap transfer. J Korean Soc Plast Reconstr Surg. 1981. 8:189–198.5. Lee DJ, Hur E, Cho MJ, Lim P. Clinical experiences of free flap transfer. J Korean Soc Plast Reconstr Surg. 1980. 7:313–320.6. Franklin JD, Withers EH, Madden JJ Jr, Lynch JB. Use of the free dorsalis pedis flap in head and neck repairs. Plast Reconstr Surg. 1979. 63:195–204.
Article7. Leeb DC, Ben-Hur N, Mazzarella L. Reconstruction of the floor of the mouth with a free Dorsalis pedis flap. Plast Reconstr Surg. 1977. 59:379–381.
Article8. Ahn HC, Yang EZ, Kim CY, Lee JH. Various applications of deep inferior epigastric artery perforator free flap. J Korean Soc Plast Reconstr Surg. 2009. 36:707–713.9. Choi BK, Kim YS, Lee WJ, Lew DH, Tark KC. The Safety of microsurgical head and neck reconstruction in the elderly patients. J Korean Soc Plast Reconstr Surg. 2006. 33:289–293.10. Jeon BJ, Lim SY, Hyon WS, Bang SI, Oh KS, Mun GH. Anterolateral thigh flap: our experiences in head and neck reconstruction. J Korean Soc Plast Reconstr Surg. 2006. 33:276–282.11. Tark KC, Yoon JS, Shin KS. Analysis of 83 consecutive free flaps. J Korean Soc Plast Reconstr Surg. 1993. 20:155–166.12. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989. 42:645–648.
Article13. Kroll SS, Rosenfield L. Perforator-based flaps for low posterior midline defects. Plast Reconstr Surg. 1988. 81:561–566.
Article14. Lee KS, Chang JS, Park JW. Functioning gracilis musculocutaneous free flap transplantation for the reconstruction of injured upper extremity. J Korean Orthop Assoc. 1992. 27:1868–1876.
Article15. Jung KM, Hong IP, Kim JH. Reconstruction of extensive lower extermity soft tissue defect using free latissimus dorsi muscle flap with STSG. J Korean Soc Plast Reconstr Surg. 1999. 26:927–932.16. Cho KS, Kim DY, Lee SY, Cho BH. Reconstruction of the tissue defects of extremities with anterolateral thigh free flap. J Korean Soc Plast Reconstr Surg. 1999. 26:281–286.17. Kim HS, Kim KC, Kim SE. Soft tissue reconstruction of children's extremity with perforator free flap. J Korean Soc Microsurg. 2007. 16:14–22.18. Oh CH, Shim JS, Park DH. Lower extremity reconstruction by perforator based flap. J Korean Soc Plast Reconstr Surg. 2009. 36:720–726.19. Whitaker IS, Smit JM, Rozen W, Dimopoulou A, Acosta R. Pre operative computed tomographic angiography (CTA): a valuable lesson in planning DIEP flaps. J Plast Reconstr Aesthet Surg. 2009. 62:551.
Article20. Lim SY, Pyon JK, Mun GH, Bang SI, Oh KS. Surgical treatment of angiosarcoma of the scalp with superficial parotidectomy. Ann Plast Surg. 2010. 64:180–182.
Article21. Kim YH, Kim JT. Perforator flaps in head and neck reconstruction. Hanyang Med Rev. 2009. 29:265–273.
Article22. Thorwarth M, Eulzer C, Bader R, Wolf C, Schmidt M, Schultze-Mosgau S. Free flap transfer in cranio-maxillofacial surgery: a review of the current data. Oral Maxillofac Surg. 2008. 12:113–124.
Article23. Lipa JE, Butler CE. Enhancing the outcome of free latissimus dorsi muscle flap reconstruction of scalp defects. Head Neck. 2004. 26:46–53.
Article24. Lee SH, Mun GH. Transverse thoracodorsal artery perforator flaps: experience with 31 free flaps. J Plast Reconstr Aesthet Surg. 2008. 61:372–379.
Article25. Amin A, Rifaat M, Civantos F, Weed D, Abu-Sedira M, Bassiouny M. Free anterolateral thigh flap for reconstruction of major craniofacial defects. J Reconstr Microsurg. 2006. 22:97–104.
Article26. Koshima I, Inagawa K, Urushibara K, Moriguchi T. Paraumbilical perforator flap without deep inferior epigastric vessels. Plast Reconstr Surg. 1998. 102:1052–1057.
Article27. Mun GH, Lim SY, Hyon WS, Bang SI, Oh KS. A novel reconstruction of 2 distinct defects: concomitant use of a thoracodorsal artery perforator flap and its corresponding muscle flap. Ann Plast Surg. 2005. 55:676–678.28. Choi HC, Han SH, Koh KS, Yoon KC, Chung BS. Free muscle flap reconstruction following resection of the skull base tumour. J Korean Soc Plast Reconstr Surg. 1993. 20:1257–1265.29. Hanasono MM, Sacks JM, Goel N, Ayad M, Skoracki RJ. The anterolateral thigh free flap for skull base reconstruction. Otolaryngol Head Neck Surg. 2009. 140:855–860.
Article30. Zhang B, Li DZ, Xu ZG, Tang PZ. Deep inferior epigastric artery perforator free flaps in head and neck reconstruction. Oral Oncol. 2009. 45:116–120.
Article31. Kim KH, Chung CH, Chang YJ, Rho YS. Reconstruction of midfacial defects with free flaps after maxillectomy. J Korean Soc Plast Reconstr Surg. 2010. 37:607–612.32. Santamaria E, Granados M, Barrera-Franco JL. Radial forearm free tissue transfer for head and neck reconstruction: versatility and reliability of a single donor site. Microsurgery. 2000. 20:195–201.
Article33. Browne JD, Burke AJ. Benefits of routine maxillectomy and orbital reconstruction with the rectus abdominis free flap. Otolaryngol Head Neck Surg. 1999. 121:203–209.
Article34. Uglesic V, Virag M, Varga S, Knezevic P, Milenovic A. Reconstruction following radical maxillectomy with flaps supplied by the subscapular artery. J Craniomaxillofac Surg. 2000. 28:153–160.
Article35. Suga H, Asato H, Okazaki M, Okochi M, Narushima M. Combination of costal cartilage graft and rib-latissimus dorsi flap: a new strategy for secondary reconstruction of the maxilla. J Craniofac Surg. 2007. 18:639–642.36. Andrades P, Rosenthal EL, Carroll WR, Baranano CF, Peters GE. Zygomatic-maxillary buttress reconstruction of midface defects with the osteocutaneous radial forearm free flap. Head Neck. 2008. 30:1295–1302.
Article37. Chang DW, Langstein HN. Use of the free fibula flap for restoration of orbital support and midfacial projection following maxillectomy. J Reconstr Microsurg. 2003. 19:147–152.
Article38. Maranzano M, Atzei A. The versatility of vascularized iliac crest with internal oblique muscle flap for composite upper maxillary reconstruction. Microsurgery. 2007. 27:37–42.
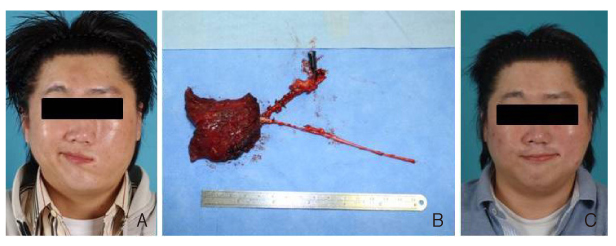
Article39. Pomahac B, Lengele B, Ridgway EB, Matros E, Andrews BT, Cooper JS, Kutz R, Pribaz JJ. Vascular considerations in composite midfacial allotransplantation. Plast Reconstr Surg. 2010. 125:517–522.
Article40. Blocker TG Jr, Stout RA. Mandibular reconstruction, World War II. Plast Reconstr Surg (1946). 1949. 4:153–156.
Article41. Shenaq SM, Klebuc MJ. The iliac crest microsurgical free flap in mandibular reconstruction. Clin Plast Surg. 1994. 21:37–44.
Article42. Wei FC, Jain V, Celik N, Chen HC, Chuang DC, Lin CH. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002. 109:2219–2226.
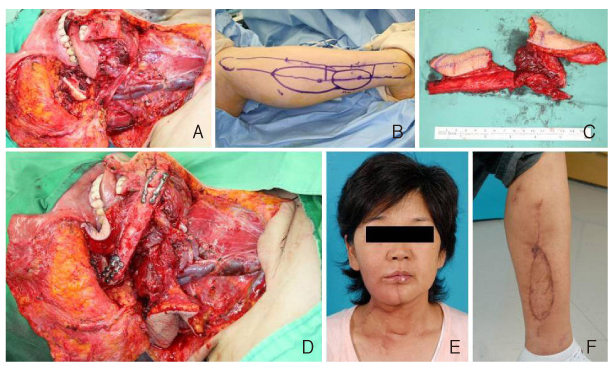
Article43. Harii K, Ohmori K, Torii S. Free gracilis muscle transplantation, with microneurovascular anastomoses for the treatment of facial paralysis. A preliminary report. Plast Reconstr Surg. 1976. 57:133–143.
Article44. Terzis JK. Pectoralis minor: a unique muscle for correction of facial palsy. Plast Reconstr Surg. 1989. 83:767–776.45. Harii K, Asato H, Yoshimura K, Sugawara Y, Nakatsuka T, Ueda K. One-stage transfer of the latissimus dorsi muscle for reanimation of a paralyzed face: a new alternative. Plast Reconstr Surg. 1998. 102:941–951.
Article46. Choi JH, Minn KW. Chest wall reconstruction with muscle flap. J Korean Soc Plast Reconstr Surg. 2003. 30:413–419.47. Sullivan SR, Truxillo TM, Mann GN, Isik FF. Utility of the free deep inferior epigastric perforator flap in chest wall reconstruction. Breast J. 2007. 13:50–54.
Article48. Ahn S. Breast reconstruction using implants. J Korean Med Assoc. 2011. 54:51–60.
Article49. Cho YK, Yang JD, Kim GR, Chung HY, Cho BC, Park HY. Immediate implant reconstruction using silicone prosthesis in breast cancer patients after skin sparing mastectomy. J Korean Soc Plast Reconstr Surg. 2010. 37:749–757.50. Lee HK, Kim YJ, Lee SJ. The latissimus dorsi flap with an implant: the most useful & proper breast reconstruction method for the young mastectomy patient. J Korean Soc Aesthetic Plast Surg. 2000. 6:83–90.51. Park JH, Bang SI, Kim SH, Im SY, Mun GH, Hyon WS, Oh KS. Breast reconstruction with the extended latissimus dorsi musculocutancous flap. J Korean Soc Plast Reconstr Surg. 2005. 32:408–415.52. Eom JS. Breast reconstruction using pedicled transverse rectus abdominis musculocutaneous (TRAM) flap. J Korean Med Assoc. 2011. 54:12–21.
Article53. Kim EK, Eom JS, Ahn SH, Son BH, Lee TJ. Evolution of the pedicled TRAM flap: a prospective study of 500 consecutive cases by a single surgeon in Asian patients. Ann Plast Surg. 2009. 63:378–382.54. Nahabedian MY, Momen B, Galdino G, Manson PN. Breast reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg. 2002. 110:466–475.
Article55. Jin US, Minn KW. Breast reconstruction using the transverse rectus abdominis musculocutaneous (TRAM) free flap. J Korean Med Assoc. 2011. 54:22–34.
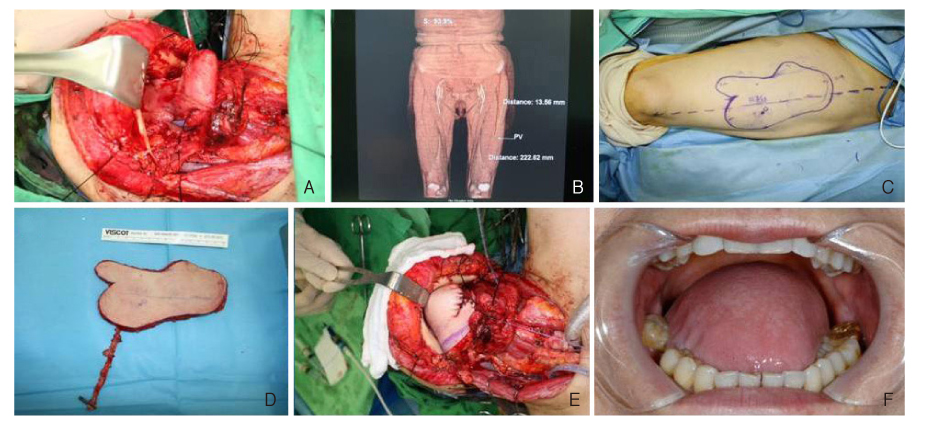
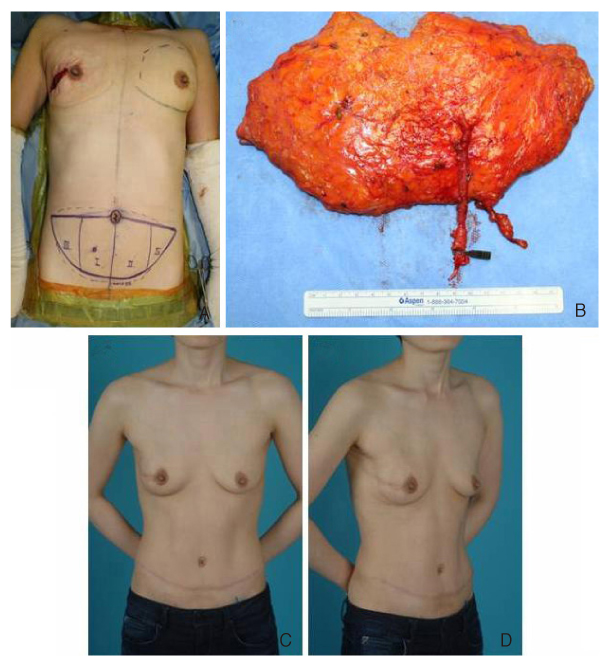
Article56. Kim JH, Park JU, Cho SH, Eo SR. Immediate breast reconstruction with DIEP free flap. J Korean Soc Microsurg. 2008. 17:94–100.57. Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivan SK, Boraski J, Metzinger SE, Dupin CL, Allen RJ. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004. 113:1153–1160.
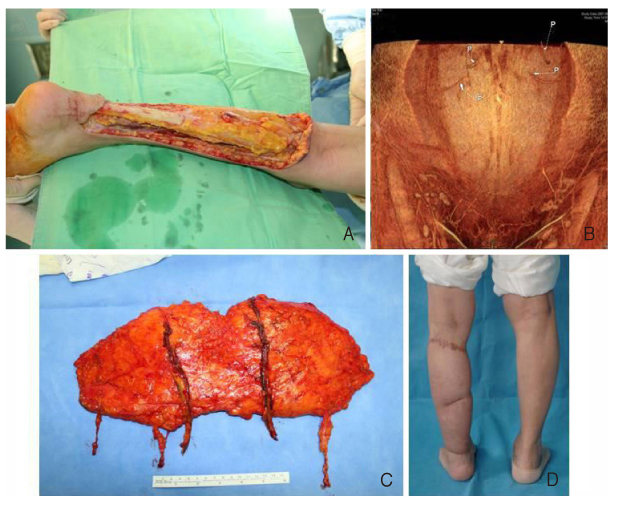
Article58. Tajsic N, Winkel R, Hoffmann R, Husum H. Sural perforator flap for reconstructive surgery in the lower leg and the foot: a clinical study of 86 patients with post-traumatic osteomyelitis. J Plast Reconstr Aesthet Surg. 2009. 62:1701–1708.
Article59. Wong CH, Tan BK. Perforator-sparing transposition flaps for lower limb defects: anatomic study and clinical application. Ann Plast Surg. 2007. 58:614–621.60. Momeni A, Krischak S, Bannasch H. The thoracodorsal artery perforator flap with a vascularized scapular segment for reconstruction of a composite lower extremity defect. Microsurgery. 2006. 26:515–518.
Article61. Yang D, Yang JF, Morris SF, Tang M, Nie C. Medial plantar artery perforator flap for soft-tissue reconstruction of the heel. Ann Plast Surg. 2011. 02. 04. [Epub].
Article62. Unglaub F, Wolf MB, Dragu A, Forst J, Horch RE, Kneser U. Reconstruction of a child's forefoot defect using a distally based pedicled medial plantar flap. Arch Orthop Trauma Surg. 2010. 130:155–158.
Article63. Caleffi E, Bocchi A, Montacchini G, Papadia F. Reconstruction of the heel by a medial plantar flap. Ital J Orthop Traumatol. 1989. 15:191–196.64. Botte MJ, Gellman H. Reconstruction of a traumatic hallux amputation using a plantar V-Y advancement flap. Clin Orthop Relat Res. 1987. (220):211–216.
Article65. Tamura A, Takeuchi Y, Yamakage A. Reconstruction of plantar heel defects with free gracilis musculocutaneous flap. J Foot Ankle Surg. 1994. 33:274–277.66. Dubrow TJ, Lesavoy MA. Acne of the heel: acne vulgaris complicating a free vascularized latissimus dorsi musculocutaneous flap. Ann Plast Surg. 1989. 23:349–351.
Article67. Ikuta Y, Murakami T, Yoshioka K, Tsuge K. Reconstruction of the heel pad by flexor digitorum brevis musculocutaneous flap transfer. Plast Reconstr Surg. 1984. 74:86–96.
Article68. Bostwick J 3rd. Reconstruction of the heel pad by muscle transposition and split skin graft. Surg Gynecol Obstet. 1976. 143:973–974.
Article69. Jeong JH. Reconstruction of large heel defects using gracilis muscle free flaps. Yeungnam Univ J Med. 1997. 14:227–236.
Article70. Hong JP. Reconstruction of the diabetic foot using the anterolateral thigh perforator flap. Plast Reconstr Surg. 2006. 117:1599–1608.
Article71. Nagase T, Gonda K, Inoue K, Higashino T, Fukuda N, Gorai K, Mihara M, Nakanishi M, Koshima I. Treatment of lymphedema with lymphaticovenular anastomoses. Int J Clin Oncol. 2005. 10:304–310.
Article72. Dubernard JM, Owen E, Herzberg G, Martin X, Guigal V, Dawahra M, Pasticier G, Mongin-Long D, Kopp C, Ostapetz A, Lanzetta M, Kapila H, Hakim N. The first transplantation of a hand in humans: early results. Chirurgie. 1999. 124:358–365.73. Devauchelle B, Badet L, Lengelé B, Morelon E, Testelin S, Michallet M, D'Hauthuille C, Dubernard JM. First human face allograft: early report. Lancet. 2006. 368:203–209.
Article74. Dubernard JM, Lengele B, Morelon E, Testelin S, Badet L, Moure C, Beziat JL, Dakpe S, Kanitakis J, D'Hauthuille C, El Jaafari A, Petruzzo P, Lefrancois N, Taha F, Sirigu A, Di Marco G, Carmi E, Bachmann D, Cremades S, Giraux P, Burloux G, Hequet O, Parquet N, Frances C, Michallet M, Martin X, Devauchelle B. Outcomes 18 months after the firs4t human partial face transplantation. N Engl J Med. 2007. 357:2451–2460.
Article75. Soni CV, Barker JH, Pushpakumar SB, Furr LA, Cunningham M, Banis JC Jr, Frank J. Psychosocial considerations in facial transplantation. Burns. 2010. 36:959–964.
Article76. Siemionow M, Agaoglu G, Unal S. A cadaver study in preparation for facial allograft transplantation in humans: part II. Mock facial transplantation. Plast Reconstr Surg. 2006. 117:876–885.
Article77. Siemionow MZ, Gordon CR. Institutional review board-based recommendations for medical institutions pursuing protocol approval for facial transplantation. Plast Reconstr Surg. 2010. 126:1232–1239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stepwise Training for Reconstructive Microsurgery: The Journey to Becoming a Confident Microsurgeon in Singapore
- The Optimal Color of Background Sheets for Microsurgery
- History and Recent Advances in Microsurgery
- Digital Artery Perforator Flaps
- A Mountain Head Lamp Applied for Loupes-assisted Microsurgery