J Korean Neurosurg Soc.
2013 Mar;53(3):145-149. 10.3340/jkns.2013.53.3.145.
Clinical and Radiologic Analysis of Posterior Apophyseal Ring Separation Associated with Lumbar Disc Herniation
- Affiliations
-
- 1Department of Neurosurgery, Nanoori Hospital, Seoul, Korea. medmaxx@naver.com
- KMID: 2190741
- DOI: http://doi.org/10.3340/jkns.2013.53.3.145
Abstract
OBJECTIVE
We analyzed the clinical and radiologic features of posterior apophyseal ring separation (PARS) with lumbar disc herniation and suggest the proper management options according to the PARS characteristics.
METHODS
We reviewed case series of patients with PARS who underwent surgery of lumbar disc herniation. Preoperative symptoms, neurologic status, Body Mass Index, preoperative and postoperative Visual Analogue Scale (VAS) and Korean-Oswestry Disability Index (K-ODI) scores, operation types were obtained. PARS size, locations, the degree of resection were assessed.
RESULTS
PARS was diagnosed in 109 (7.5%) patients among 1448 patients given surgical treatment for single level lumbar disc herniation. There were 55 (50.5%) small PARS and 54 (49.5%) large PARS. Among the large PARS group, 15 (27.8%) had lower endplate PARS of upper vertebra at the level of disc herniation. Thirty-nine (72.2%) were upper endplate PARS of lower vertebra. Among the group with upper endplate PARS of lower vertebra, unresected PARS was diagnosed in 12 (30.8%) cases and resected PARS was diagnosed in 27 (69.2%) cases. VAS and K-ODI scores changes were 3.6+/-2.9 and 5.4+/-6.4 in the unresected PARS group, 5.8+/-2.1 and 11.3+/-7.1 in the resected PARS group. The group with upper endplate PARS of lower vertebra showed significant difference of VAS (p=0.01) and K-ODI (p=0.013) score changes between unresected and resected PARS groups.
CONCLUSION
The large PARS of upper endplate in lower vertebra should be removed during the surgery of lumbar disc herniation. High level or bilateral side of PARS should be widely decompressed and arthrodesis procedures are necessary if there is a possibility of secondary instability.
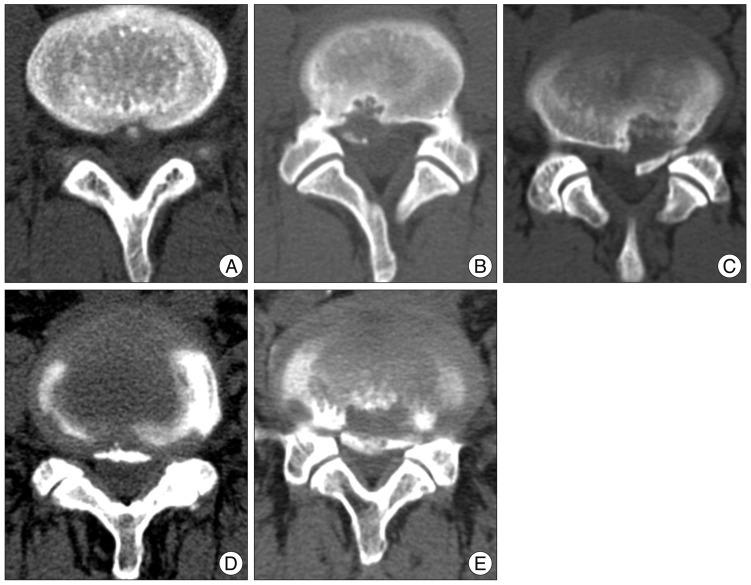
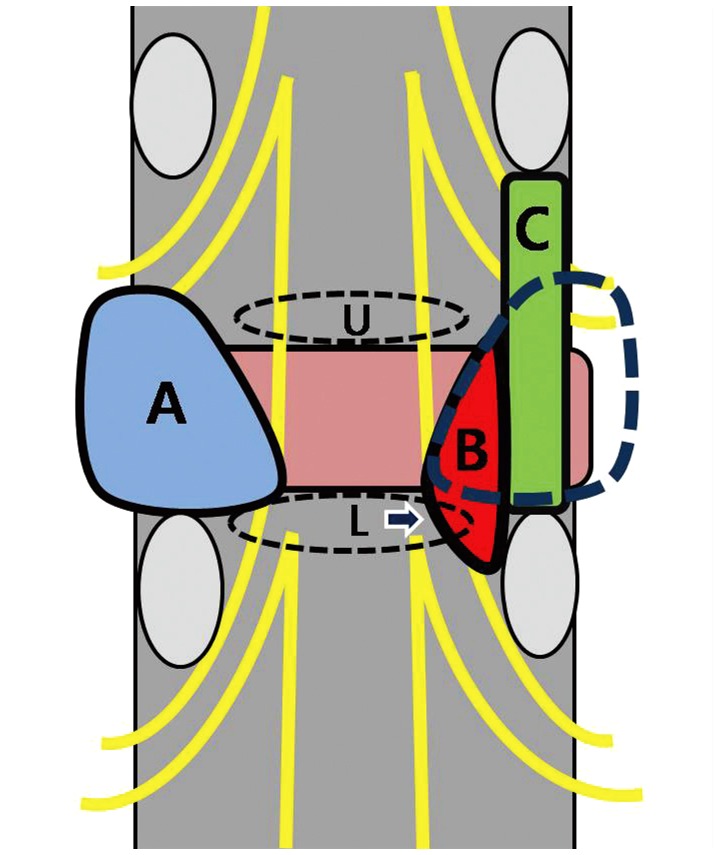
Figure
Reference
-
1. Akhaddar A, Belfquih H, Oukabli M, Boucetta M. Posterior ring apophysis separation combined with lumbar disc herniation in adults : a 10-year experience in the surgical management of 87 cases. J Neurosurg Spine. 2011; 14:475–483. PMID: 21294611.
Article2. Asazuma T, Nobuta M, Sato M, Yamagishi M, Fujikawa K. Lumbar disc herniation associated with separation of the posterior ring apophysis: analysis of five surgical cases and review of the literature. Acta Neurochir (Wien). 2003; 145:461–466. discussion 466. PMID: 12836070.
Article3. Banerian KG, Wang AM, Samberg LC, Kerr HH, Wesolowski DP. Association of vertebral end plate fracture with pediatric lumbar intervertebral disk herniation : value of CT and MR imaging. Radiology. 1990; 177:763–765. PMID: 2243985.
Article4. Baranto A, Ekström L, Hellström M, Lundin O, Holm S, Swärd L. Fracture patterns of the adolescent porcine spine : an experimental loading study in bending-compression. Spine (Phila Pa 1976). 2005; 30:75–82. PMID: 15626985.
Article5. Bick EM, Coper JW. The ring apophysis of the human vertebra; contribution to human osteogeny. II. J Bone Joint Surg Am. 1951; 33-A:783–787. PMID: 14850517.6. Chang CH, Lee ZL, Chen WJ, Tan CF, Chen LH. Clinical significance of ring apophysis fracture in adolescent lumbar disc herniation. Spine (Phila Pa 1976). 2008; 33:1750–1754. PMID: 18628708.
Article7. Chen LH, Chang CH, Lee ZL, Niu CC, Lai PL, Tan CF, et al. Intervertebral disc herniation in adolescents. Chang Gung Med J. 2004; 27:22–28. PMID: 15074886.8. Cheon MH, Lee MK, Kim DH, Kim HH, Kim DJ. Clinical analysis of posterior lymbar apophyseal ring fractures in young adults. J Korean Neurosurg Soc. 1996; 25:1964–1969.9. Dake MD, Jacobs RP, Margolin FR. Computed tomography of posterior lumbar apophyseal ring fractures. J Comput Assist Tomogr. 1985; 9:730–732. PMID: 3160730.
Article10. Edelson JG, Nathan H. Stages in the natural history of the vertebral end-plates. Spine (Phila Pa 1976). 1988; 13:21–26. PMID: 3381133.
Article11. Epstein NE, Epstein JA. Limbus lumbar vertebral fractures in 27 adolescents and adults. Spine (Phila Pa 1976). 1991; 16:962–966. PMID: 1948383.
Article12. Epstein NE, Epstein JA, Mauri T. Treatment of fractures of the vertebral limbus and spinal stenosis in five adolescents and five adults. Neurosurgery. 1989; 24:595–604. PMID: 2710305.
Article13. Gomori JM, Floman Y, Liebergall M. CT of adult lumbar disc herniations mimicking posterior apophyseal ring fractures. Neuroradiology. 1991; 33:414–418. PMID: 1749472.
Article14. Handel SF, Twiford TW Jr, Reigel DH, Kaufman HH. Posterior lumbar apophyseal fractures. Radiology. 1979; 130:629–633. PMID: 424528.
Article15. Kaiser MC, Capesius P, Veiga-Pires JA, Sandt G. A sign of lumbar disk herniation recognizable on lateral CT generated digital radiograms. J Comput Assist Tomogr. 1984; 8:1066–1071. PMID: 6238982.
Article16. Leroux JL, Fuentes JM, Baixas P, Benezech J, Chertok P, Blotman F. Lumbar posterior marginal node (LPMN) in adults. Report of fifteen cases. Spine (Phila Pa 1976). 1992; 17:1505–1508. PMID: 1471010.17. Martínez-Lage JF, Poza M, Arcas P. Avulsed lumbar vertebral rim plate in an adolescent : trauma or malformation? Childs Nerv Syst. 1998; 14:131–134. PMID: 9579870.
Article18. Savini R, Di Silvestre M, Gargiulo G, Picci P. Posterior lumbar apophyseal fractures. Spine (Phila Pa 1976). 1991; 16:1118–1123. PMID: 1948402.
Article19. Shirado O, Yamazaki Y, Takeda N, Minami A. Lumbar disc herniation associated with separation of the ring apophysis : is removal of the detached apophyses mandatory to achieve satisfactory results? Clin Orthop Relat Res. 2005; 120–128. PMID: 15685064.20. Shiwaku K, Anuurad E, Enkhmaa B, Nogi A, Kitajima K, Shimono K, et al. Overweight Japanese with body mass indexes of 23.0-24.9 have higher risks for obesity-associated disorders : a comparison of Japanese and Mongolians. Int J Obes Relat Metab Disord. 2004; 28:152–158. PMID: 14557832.
Article21. Takata K, Inoue S, Takahashi K, Ohtsuka Y. Fracture of the posterior margin of a lumbar vertebral body. J Bone Joint Surg Am. 1988; 70:589–594. PMID: 3356726.
Article22. Tamano K, Shinohara K, Mikami H. A clinical study of displaced ring apophysis. J C-S Orthop Assoc. 1994; 6:431–433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lumbar Disc Herniation Combined with Posterior Apophyseal Ring Separation in a Young Child: A Case Report
- Posterior Apophyseal Ring Fracture in Adult Lumbar Disc Herniation: An 8-Year Experience in Minimally Invasive Surgical Management of 48 Cases
- Clinical Analysis of Recurrent Lumbar Disc Herniation
- Lumbar apophyseal ring fracture and disc herniation: CT and MRI manifestations
- Clinical Analysis of Posterior Lymbar Apophyseal Ring Fractures in Young Adults