J Korean Orthop Assoc.
2013 Dec;48(6):426-432. 10.4055/jkoa.2013.48.6.426.
Cementless Total Hip Arthroplasty Using the Conical Femoral Stem
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Chosun University, Gwangju, Korea. shalee@chosun.ac.kr
- KMID: 2185276
- DOI: http://doi.org/10.4055/jkoa.2013.48.6.426
Abstract
- PURPOSE
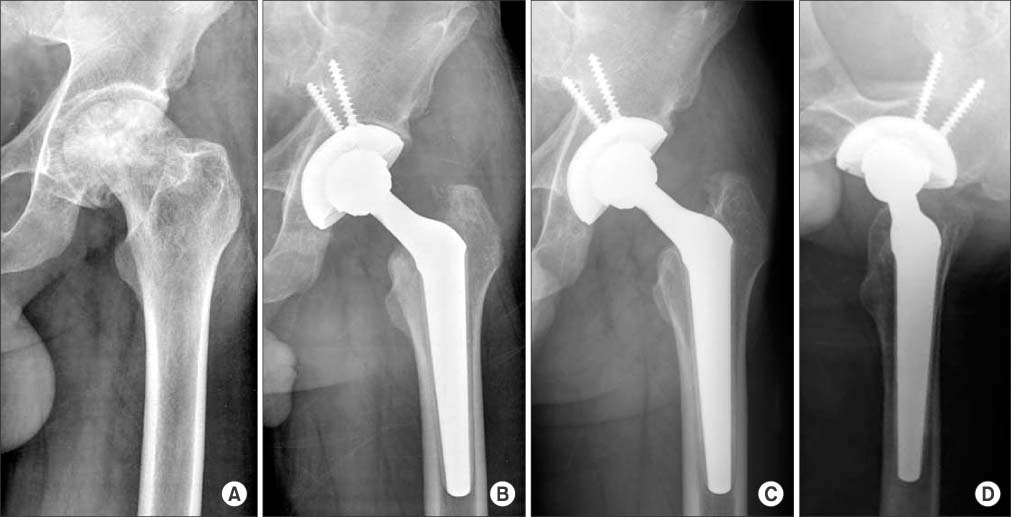
The purpose of this study is to evaluate the clinical and radiological results of cementless total hip arthroplasty using a conical stem.
MATERIALS AND METHODS
From June 2005 to December 2007, total hip arthroplasty using the conical stem was performed in 47 patients and 51 hips. The most common causes for total hip arthroplaty were osteonecrosis of the femoral head in 32 cases. The mean follow-up period was 74.3 months (range: 62-93 months) and the mean age was 51.2 years (range: 36-84 years). The clinical evaluation included the Harris hip score, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and pain on the inguinal area or thigh. Radiographic evaluation was performed for determination of the fixation status of the implant, the radiolucent line, subsidence, loosening and heterotopic ossification around the acetabular cup and the femoral stem.
RESULTS
At the most recent follow-up, the mean Harris hip score was 94.1 points and the WOMAC score was 11.3 points. Radiologically, bone ongrowth was seen in all cases without migration of acetabular cup, femoral stem, changing of the position, subsidence and loosening. Complications included two cases of posterior dislocation, one case of heterotopic ossification, and one case of deep vein thrombosis.
CONCLUSION
Cementless total hip arthroplasty using the conical femoral stem shows good clinical and radiologic results in treatment of osteonecrosis of the femoral head with normal canal flare index and femur neck fracture with stove pipe type.
MeSH Terms
Figure
Reference
-
1. Engh CA, Bobyn JD. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop Relat Res. 1988; 231:7–28.
Article2. McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented femoral component. Excellent results at ten-year follow-up. J Bone Joint Surg Br. 1997; 79:900–907.3. Noble PC, Alexander JW, Lindahl LJ, Yew DT, Granberry WM, Tullos HS. The anatomic basis of femoral component design. Clin Orthop Relat Res. 1988; 235:148–165.
Article4. Dinse GE, Lagakos SW. Nonparametric estimation of lifetime and disease onset distributions from incomplete observations. Biometrics. 1982; 38:921–932.
Article5. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988; 15:1833–1840.6. Lee S, Kim JH, Ko DO, Jeon YW, Yang SJ, Ryu CW. Ceramic on ceramic hybrid type total hip arthroplasty in patients with more than 65 years of age -minimum 5-year follow-up results. J Korean Hip Soc. 2008; 20:91–97.
Article7. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; 121:20–32.
Article8. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of ient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988; 15:1833–1840.9. Kawamura H, Dunbar MJ, Murray P, Bourne RB, Rorabeck CH. The porous coated anatomic total hip replacement. A ten to fourteen-year follow-up study of a cementless total hip arthroplasty. J Bone Joint Surg Am. 2001; 83:1333–1338.10. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; 141:17–27.11. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990; 257:107–128.
Article12. Rothman RH, Hozack WJ, Ranawat A, Moriarty L. Hydroxyapatite-coated femoral stems. A matched-pair analysis of coated and uncoated implants. J Bone Joint Surg Am. 1996; 78:319–324.
Article13. Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am. 1995; 77:432–439.
Article14. Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988; 70:337–346.
Article15. Wagner H, Wagner M. Cone prosthesis for the hip joint. Arch Orthop Trauma Surg. 2000; 120:88–95.
Article16. Linde F, Jensen J. Socket loosening in arthroplasty for congenital dislocation of the hip. Acta Orthop Scand. 1988; 59:254–257.
Article17. Lubahn JD, Evarts CM, Feltner JB. Conversion of ankylosed hips to total hip arthroplasty. Clin Orthop Relat Res. 1980; 153:146–152.
Article18. Nagano H, Inoue H, Usui M, Mitani S, Satoh T. Long-term results of Charnley low-friction arthroplasty for coxarthrosis with congenital hip dysplasia. 15 year follow-up study. Bull Hosp Jt Dis. 1997; 56:197–203.19. Dickob M, Martini T. The cementless PM hip arthroplasty. Four-to-seven-year results. J Bone Joint Surg Br. 1996; 78:195–199.20. Schenk RK, Wehrli U. Reaction of the bone to a cement-free SL femur revision prosthesis. Histologic findings in an autopsy specimen 5 1/2 months after surgery. Orthopade. 1989; 18:454–462.21. Wong M, Eulenberger J, Schenk R, Hunziker E. Effect of surface topology on the osseointegration of implant materials in trabecular bone. J Biomed Mater Res. 1995; 29:1567–1575.
Article22. Jasty M, Bragdon CR, Rubash H, Schutzer SF, Haire T, Harris W. Unrecognized femoral fractures during cementless total hip arthroplasty in the dog and their effect on bone ingrowth. J Arthroplasty. 1992; 7:501–508.
Article23. Engh CA, Bobyn JD. Principles, techniques, results, and complications with a porous-coated sintered metal system. Instr Course Lect. 1986; 35:169–183.24. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005; 87:28–36.25. Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J Bone Joint Surg Am. 2006; 88:1183–1191.26. Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005; 87:18–27.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Hip Arthroplasty with F2L Multineck Cementless Femoral Stem
- Reference Line Closer to the True Femoral Anteversion During Primary Cementless Total Hip Arthroplasty
- Short-term Results after Cementless Total Hip Arthroplasty Using a Fully Hydroxyapatite-coated Femoral Stem
- Short Term Results of Cementless Total Hip Arthroplasty With a Tapered Femoral Component
- Usefulness of a Modular Hip System for Combined Anteversion in Cementless Total Hip Arthroplasty