J Korean Med Assoc.
2006 Dec;49(12):1154-1163. 10.5124/jkma.2006.49.12.1154.
Minimally Invasive Video-Assisted Kidney Transplantation
- Affiliations
-
- 1Department of Surgery, Chosun University College of Medicine, Korea. shdkim@chosun.ac.kr
- KMID: 2184745
- DOI: http://doi.org/10.5124/jkma.2006.49.12.1154
Abstract
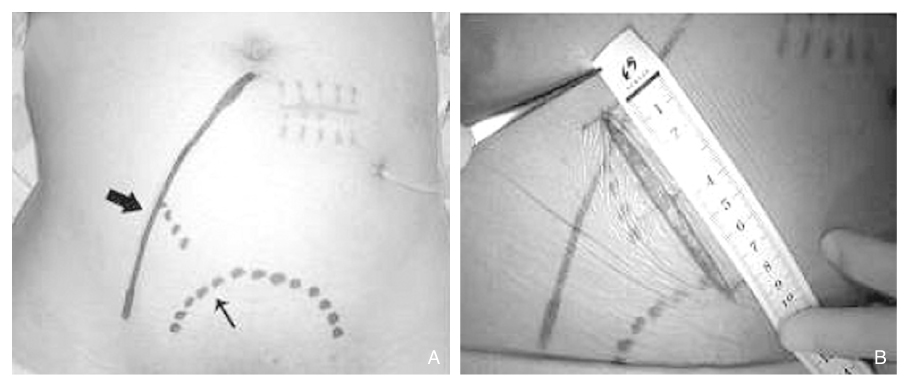
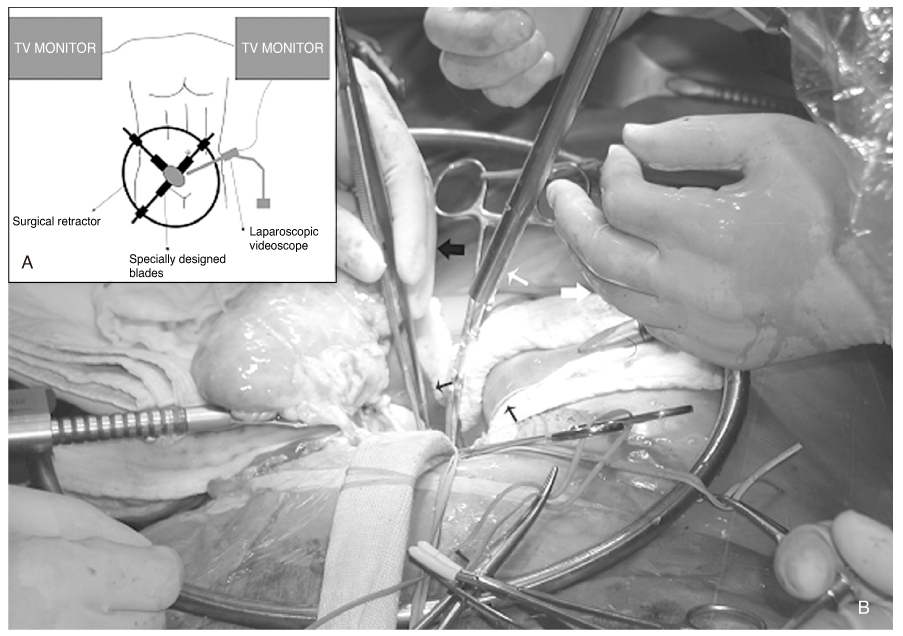
- Minimally invasive surgery (MIS) has been applied to nearly all fields of surgery due to its advantages like reduced morbidity, a better cosmetic outcome and early recovery. The recent advances in its technique have allowed us to use modified MIS technique in the field of kidney transplantation. From January 2004 to Mar 2006, minimally invasive kidney transplantation was carried out in 20 patients. Many clinical variables were compared to the conventional method. The operative procedure began with 7~8 cm skin incision. A laparoscopic balloon dissector was used to create the retroperitoneal space for the placement of the grafted kidney. Vascular anastomosis and ureteroneocystostomy were performed under direct vision and with video-assisted TV monitoring. The average length of the wound was 7.8 cm and it was placed below the belt line. The average operating time was 186 minutes. Less analgesic was given compared to conventional methods. There was one postoperative complication, a mild lymphocele. All patients showed normalized serum creatinine levels within 4 days. All grafted kidneys showed normal findings on the postoperative ultrasound and renal scans. Minimally invasive video-assisted kidney transplantation is technically feasible and may offer benefits in terms of better cosmetic outcomes, less pain and quicker recuperation than conventional kidney transplantation.
MeSH Terms
Figure
Reference
-
1. Kojima M, Konishi F, Okada M, Nagai H. Laparoscopic colectomy versus open colectomy for colorectal carcinoma: a retrospective analysis of patients followed up for at least 4 years. Surg Today. 2004. 34:1020–1024.
Article2. Patankar SK, Larach SW, Ferrara A, Williamson PR, Gallagher JT, Narayanan S, et al. Prospective comparison of laparoscopic vs. open resections for colorectal adenocarcinoma over a ten-year period. Dis Colon Rectum. 2003. 46:601–611.
Article3. Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Ponzano C, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005. 241:232–237.
Article4. Greenstein Marc A., Harkaway Richard, Badosa Francisco, Ginsberg Phillip, Yang Shuin-Lin. Minimal incision living donor nephrectomy compared to the hand-assisted laparoscopic living donor nephrectomy. World J Urol. 2003. 20:356–359.
Article5. Kurian Marina S., Gagner Michel, Murakami Yasusuke, Andrei Valeriu, Jossart Gregg, Schwartz Myron. Hand-assisted Laparoscopic Donor Hepatectomy for Living Related Transplantation in the Porcine Model. Surg Laparosc Endosc Percutan Tech. 2002. 12:232–237.
Article6. Nanni G, Tondolo V, Citterio F, Romagnoli J, Borgetti M, Castagneto M, et al. Comparison of Oblique Versus Hockey-Stick Surgical Incision for Kidney Transplantation. Transplantation Proceedings. 2005. 37:2479–2481.
Article7. Aigner C, Jaksch P, Seebacher G, Neuhauser P, Marta G, Klepetko W, et al. Single running suture the new standard technique for bronchial anastomoses in lung transplantation. Eur J Cardiothorac Surg. 2003. 23:488–493.
Article8. Van Velthoven RF, Ahlering TE, Peltier A, Skarecky DW, Clayman RV. Technique for laparoscopic running urethrovesical anastomosis:the single knot method. Urology. 2003. 61:699–702.
Article9. Demirci D, Gulmez I, Ekmekcioglu O, Karacagil M. Retroperitoneoscopic ureterolithotomy for the treatment of ureteral calculi. Urol Int. 2004. 73:234–237.
Article10. Takada M, Ichihara T, Toyama H, Suzuki Y, Kuroda Y. Retroperitoneoscopic laparoscopic distal pancreatectomy with spleen salvage. Hepatogastroenterology. 2004. 51:925–927.11. Francis DM, Walker RG, Becker GJ, Millar RJ, Powell HR, Kincaid-Smith PS, et al. Kidney transplantation from living related donors: a 19-year experience. Med J Aust. 1993. 158:244–247.
Article12. Matas AJ, Gillingham KJ, Elick BA, Dunn DL, Gruessner RW, Najarian JS, et al. Risk factors for prolonged hospitalization after kidney transplants. Clin Transplant. 1997. 11:259–264.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Establishment of Minimally Invasive Thoracic Surgery Program
- Video-Assisted Minilaparotomy Surgery (VAMS): Challenging Cases of Nephron-Sparing Surgery in a Solitary Kidney
- Single-Incision Video-Assisted Thoracoscopic Surgery for Benign Mediastinal Diseases: Experiences in Single Institution
- A case report of Successful Laparascopic Myotomy for Achalasia
- Visualizing kidney transplant techniques: a comparative study of open and robotic surgery