J Korean Fract Soc.
2008 Apr;21(2):135-139. 10.12671/jkfs.2008.21.2.135.
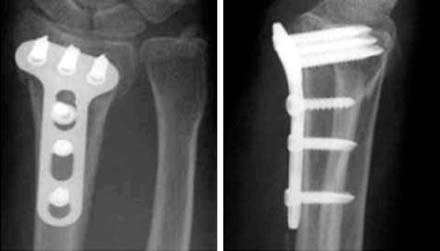
A Comparison of LCPlate versus Conventional T-plate Fixation about the Reduction Loss in the Treatment of Distal Radial Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. ostone01@ilsanpaik.ac.kr
- KMID: 2183909
- DOI: http://doi.org/10.12671/jkfs.2008.21.2.135
Abstract
-
PURPOSE: The purpose of this study was to evaluate and compare the clinical & radiological outcome between LCP and conventional T-plate fixation in the treatment of distal radial fracture.
MATERIALS AND METHODS
From January 2000 to October 2006, 26 patients were treated by LCP fixation and 20 patients were treated by conventional T-plate fixation for distal radial fracture. We used the X-ray to calculate the radial inclination, radial length and volar tilting, then compared the loss of correction after the operation between both groups. We also evaluated the clinical functional outcome by Mayo wrist score.
RESULTS
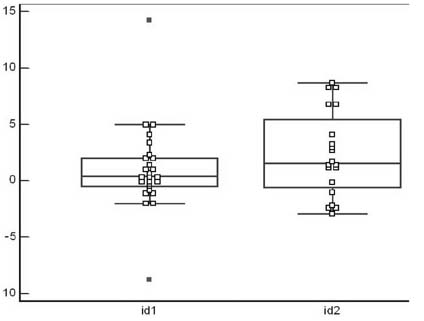
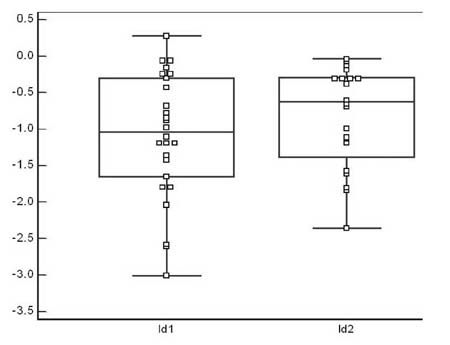
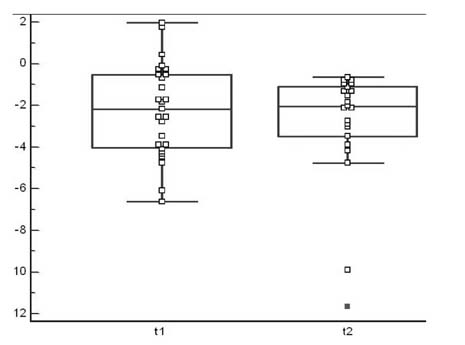
The average follow-up since operation was ten months in both LCP and conventional T-plate fixation group. According to Frykmann classification, there were 1 case of type 1 (4%), 2 of type 2 (8%), 5 of type 3 (19%), 14 of type 4 (54%), 1 of type 5 (4%), 2 of type 7 (8%), 1 of type 8 (4%), and to AO classification, 4 of type A (15%), 22 of type C (85%) in LCP group. In conventional T-plate group, according to Frykmann classification, there were 12 cases of type 3 (60%), 4 of type 4 (20%), 3 of type 7 (15%), 1 of type 8 (5%), and to AO classification, 6 of type B (30%), 14 of type C (70%). In LCP group, the loss of correction between immediate post-operation and last follow-up was about 1.03 degrees in radial inclination, -1.09 mm in radial length, -2.08 degrees in volar tilting at each, and in conventional T-plate group, 2.4 degrees in radial inclination, -0.82 mm in radial length, -2.11 degrees in volar tilting at each. There was no statistical significance (p>0.05) in two groups. In the clinical functional outcome (according to Mayo wrist score), 92% of patient showed above good result in LCP group and 85% of patient showed above good result in conventional T-plate group. There was no infection, delayed union.
CONCLUSION
Treatment by Interposition of fragments and shortening in the intractable nonunion of humerus with a bony defect can achieve not only good functional result, shortened bone union time and improved in shoulder and elbow motion.
Figure
Reference
-
1. Arora R, Lutz M, Fritz D, Zimmermann R, Oberladstätter J, Gabl M. Palmar locking plate for treatment of unstable dorsal dislocated distal radius fractures. Arch Orthop Trauma Surg. 2005; 125:399–404.
Article2. Axelrod TS, McMurtry RY. Open reduction and internal fixation of comminuted, intraarticular fractures of the distal radius. J Hand Surg Am. 1990; 15:1–11.
Article3. Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006; 88:2687–2694.
Article4. Cooney WP 3rd, Dobyns JH, Linscheid RL. Complications of Colles' fractures. J Bone Joint Surg Am. 1980; 62:613–619.
Article5. De Plama AF. Comminuted fractures of the distal end of the radius treated by ulnar pinning. J Bone Joint Surg Am. 1952; 24:651–662.6. Hove LM, Helland P, Mølster AO. Dynamic traction for unstable fractures of the distal radius. J Hand Surg Br. 1990; 24:210–214.
Article7. Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function. A prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000; 82:340–344.8. Kamano M, Honda Y, Kazuki K, Yasuda M. Palmar plating for dorsally displaced fractures of the distal radius. Clin Orthop Relat Res. 2002; 397:403–408.
Article9. Leung F, Zhu L, Ho H, Lu WW, Chow SP. Palmar plate fixation of AO Type C2 fracture of distal radius using a locking compression plate-a biomechanical study in a cadaveric model. J Hand Surg Br. 2003; 28:263–266.
Article10. Liebovic SJ, Geissler WB. Treatment of complex intra-articular distal radius fractures. Orthop Clin North Am. 1994; 25:685–706.
Article11. McAuliffe JA. Combined internal and external fixation of distal radius fractures. Hand Clin. 2005; 21:395–406.
Article12. Ring D, Prommersberger K, Jupiter JB. Combined dorsal and volar plate fixation of complex fractures of the distal part of the radius. J Bone Joint Surg Am. 2004; 86:1646–1652.
Article13. Rogachefsky RA, Lipson SR, Applegate B, Ouellette EA, Savenor AM, McAuliffe JA. Treatment of severely comminuted intra-articular fracture of the distal end of the radius by open reduction and combined interanal and external fixation. J Bone Joint Surg Am. 2001; 83:509–519.
Article14. Willis AA, Kutsumi K, Zobitz ME, Cooney WP 3rd. Internal fixation of dorsally displaced fractures of the distal part of the radius. A biomechanical analysis of volar plate fracture stability. J Bone Joint Surg Am. 2006; 88:2411–2417.
Article15. Yoo MJ, Park JY, Park HG, Chung KT. Treatment of fracture of distal radius-comparison of closed reduction and cast versus percutaneous pinning versus percutaneous pinning with external fixation. J Korean Soc Surg Hand. 2002; 7:15–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiologic Reduction Loss after Surgical Treatment of Distal Radius Fracture
- Usefulness of Reduction and Internal Fixation Using a 2.4 mm Hand Plating System in Type AO 33-A3 Distal Femur Fracture - Technical Note -
- External fixation of distal radius fracture
- Type III Monteggia Equivalent Fracture with Ipsilateral Distal Radial Epiphyseal and Ulnar Metaphyseal Fracture in a Child: Case Report
- Plate Fixation of AO Type C3 Fractures of the Distal Radius