J Korean Foot Ankle Soc.
2014 Dec;18(4):202-207. 10.14193/jkfas.2014.18.4.202.
Tibiotalocalcaneal Arthrodesis Using Retrograde Compressive Intramedullary Nail
- Affiliations
-
- 1Department of Orthopaedic Surgery, Daedong Hospital, Busan, Korea. 70sh-yoo@hanmail.net
- KMID: 2181642
- DOI: http://doi.org/10.14193/jkfas.2014.18.4.202
Abstract
- PURPOSE
The purpose of this study was to evaluate the radiological and clinical outcomes of tibiotalocalcaneal arthrodesis using retrograde compressive intramedullary nail for patients with complex hindfoot problems, including Charcot arthropathy, osteonecrosis of talus, combined arthritis of the ankle and subtalar joint, failure of previous ankle arthrodesis, and failed total ankle arthroplasty.
MATERIALS AND METHODS
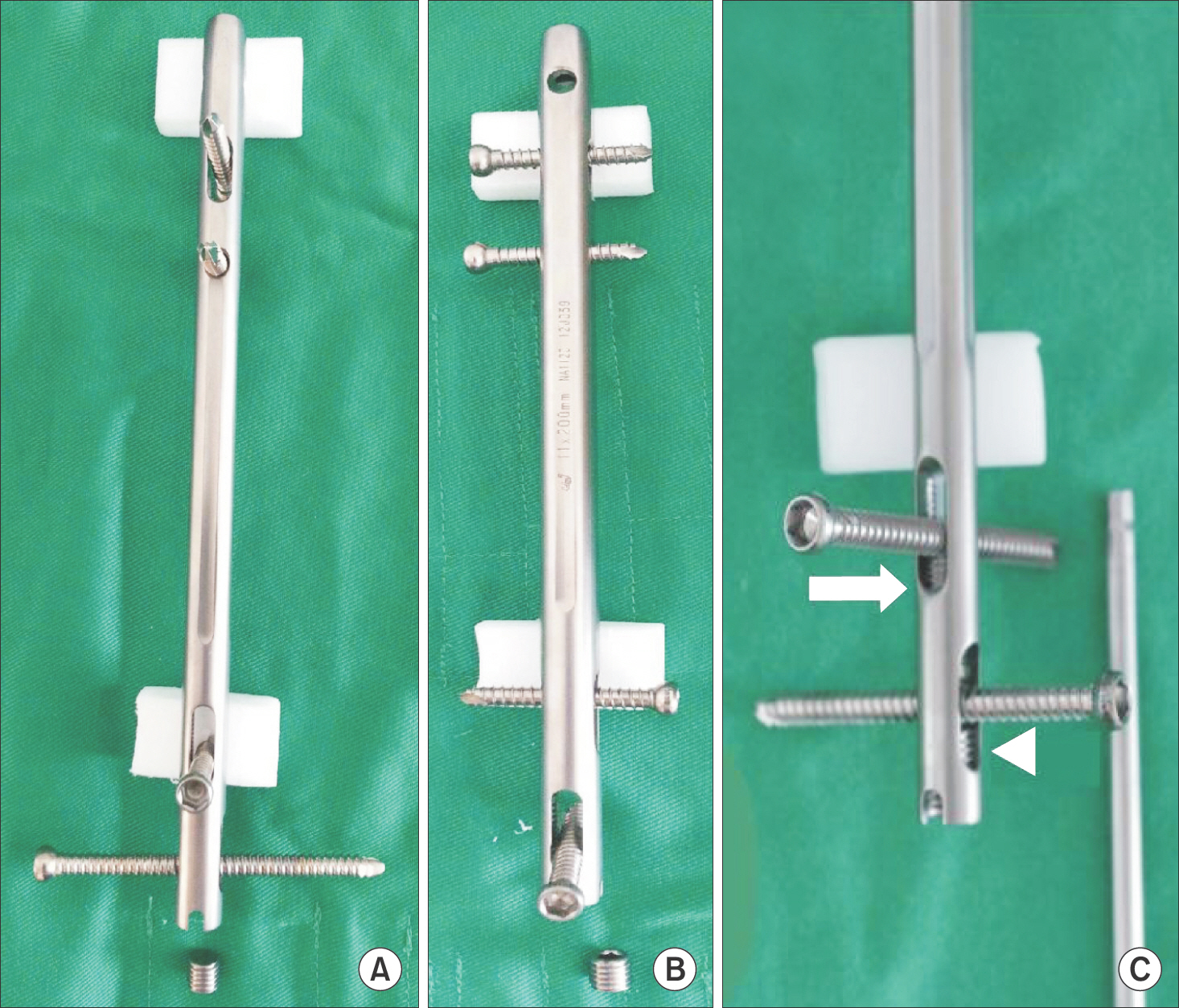
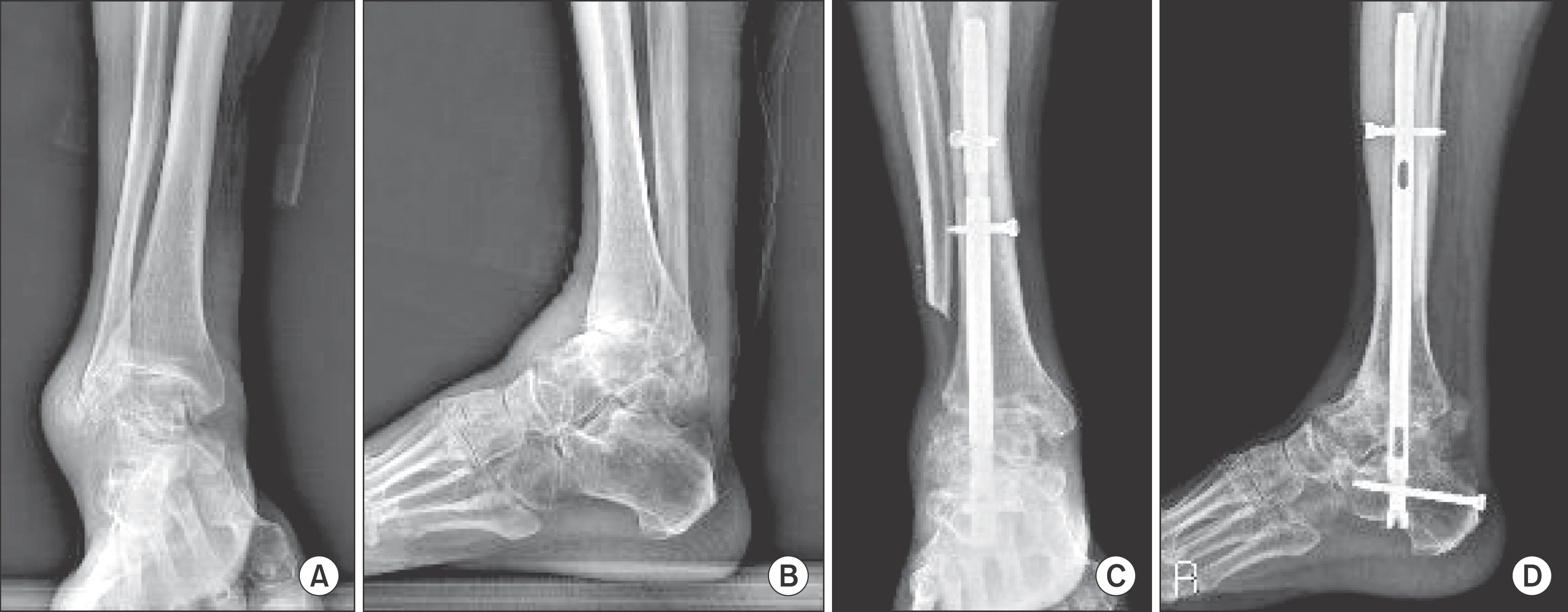
Eighteen consecutive patients (10 men and 8 women) with an average age of 54 years (range, 42~72 years) underwent tibiotalocalcaneal arthrodesis using retrograde compressive intramedullary nail fixation. The mean duration of follow-up was 16 months (range, 12~23 months). Radiological evaluation included assessment of the union status of ankle and subtalar joints. Clinical evaluations included visual analogue scale (VAS) for pain and patient satisfaction, and postoperative complications were analyzed.
RESULTS
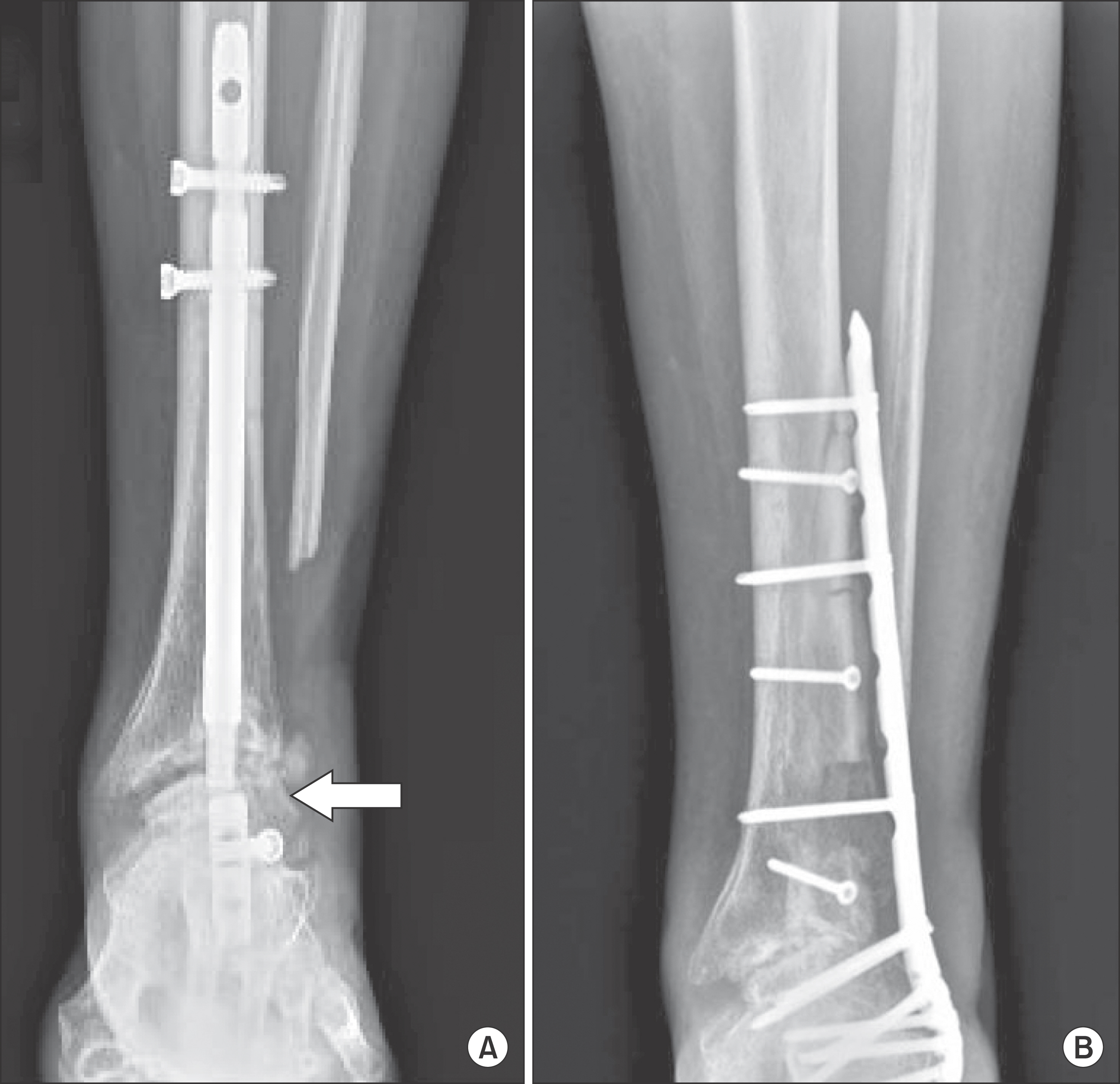
Radiological union was achieved in 14 ankle joints (77%) and 16 subtalar joints (88%) at an average of 16 weeks (range, 14~40 weeks) and 14 weeks (range, 12~24 weeks), respectively. The preoperative VAS were 4.6 (range, 4~8) at rest and 8.2 (range, 7~10) during walking, and the postoperative VAS were 2.2 (range, 0~3) and 4.6 (range, 4~6), respectively (p<0.05). There were 6 nonunions (4 ankle joints and 2 subtalar joints), 3 tibia fractures, 2 delayed union of ankle joints, and 2 breakage of the implant.
CONCLUSION
Tibiotalocalcaneal arthrodesis using retrograde compressive intramedullary nail may be considered as a viable option in patients with complex hindfoot problems.
Keyword
MeSH Terms
Figure
Reference
-
1.Treppo S., Koepp H., Quan EC., Cole AA., Kuettner KE., Grodzin-sky AJ. Comparison of biomechanical and biochemical properties of cartilage from human knee and ankle pairs. J Orthop Res. 2000. 18:739–48.
Article2.Cole AA., Margulis A., Kuettner KE. Distinguishing ankle and knee articular cartilage. Foot Ankle Clin. 2003. 8:305–16.
Article3.Acosta R., Ushiba J., Cracchiolo A 3rd. The results of a primary and staged pantalar arthrodesis and tibiotalocalcaneal arthrodesis in adult patients. Foot Ankle Int. 2000. 21:182–94.
Article4.Cooper PS. Complications of ankle and tibiotalocalcaneal arthrodesis. Clin Orthop Relat Res. 2001. 391:33–44.
Article5.Hanson TW., Cracchiolo A 3rd. The use of a 95 degree blade plate and a posterior approach to achieve tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2002. 23:704–10.6.Millett PJ., O’Malley MJ., Tolo ET., Gallina J., Fealy S., Helfet DL. Tibiotalocalcaneal fusion with a retrograde intramedullary nail: clinical and functional outcomes. Am J Orthop (Belle Mead NJ). 2002. 31:531–6.7.Mueckley TM., Eichorn S., von Oldenburg G., Speitling A., DiCicco JD 3rd., Hofmann GO, et al. Biomechanical evaluation of primary stiffness of tibiotalar arthrodesis with an intramedullary compression nail and four other fixation devices. Foot Ankle Int. 2006. 27:814–20.
Article8.Holt ES., Hansen ST., Mayo KA., Sangeorzan BJ. Ankle arthrodesis using internal screw fixation. Clin Orthop Relat Res. 1991. 268:21–8.9.Morgan CD., Henke JA., Bailey RW., Kaufer H. Long-term results of tibiotalar arthrodesis. J Bone Joint Surg Am. 1985. 67:546–50.
Article10.Papa J., Myerson M., Girard P. Salvage, with arthrodesis, in intractable diabetic neuropathic arthropathy of the foot and ankle. J Bone Joint Surg Am. 1993. 75:1056–66.
Article11.Papa JA., Myerson MS. Pantalar and tibiotalocalcaneal arthrodesis for post-traumatic osteoarthrosis of the ankle and hindfoot. J Bone Joint Surg Am. 1992. 74:1042–9.
Article12.Quill GE. The use of a second-generation intramedullary nail in the fixation of difficult ankle and hind foot arthrodesis. Am J Orthop. 1999. 1:23–31.13.Mückley T., Klos K., Drechsel T., Beimel C., Gras F., Hofmann GO. Short-term outcome of retrograde tibiotalocalcaneal arthrodesis with a curved intramedullary nail. Foot Ankle Int. 2011. 32:47–56.
Article14.Noonan T., Pinzur M., Paxinos O., Havey R., Patwardhin A. Tibio-talocalcaneal arthrodesis with a retrograde intramedullary nail: a biomechanical analysis of the effect of nail length. Foot Ankle Int. 2005. 26:304–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Surgical Outcome of Tibiotalocalcaneal Arthrodesis Using a Retrograde Intramedullary Nail
- Interlocking Intramedullary Nail Fixation for Tibiotalocalcaneal Fusion(2 cases)
- Arthrodesis of the Knee Using a Retrograde Femoral Intramedullary Nail: Technical Report
- Value of Tibiotalocalcaneal Arthrodesis Using Retrograde Intramedullary Nailing in Severe Hindfoot Deformity and Arthritis
- Foot and Ankle Motion after Tibiotalocalcaneal Arthrodesis: Comparison with Tibiotalar Arthrodesis Using a Multi-Segment Foot Model