J Dent Rehabil Appl Sci.
2015 Sep;31(3):273-282. 10.14368/jdras.2015.31.3.273.
Prosthetic rehabilitation for a patient with CO-MI discrepancy
- Affiliations
-
- 1Department of Prosthodontics and Research Institute of Oral Science College of Dentistry, Gangneung-Wonju National University, Gangneung, Republic of Korea. doctorcj@gwnu.ac.kr
- KMID: 2180030
- DOI: http://doi.org/10.14368/jdras.2015.31.3.273
Abstract
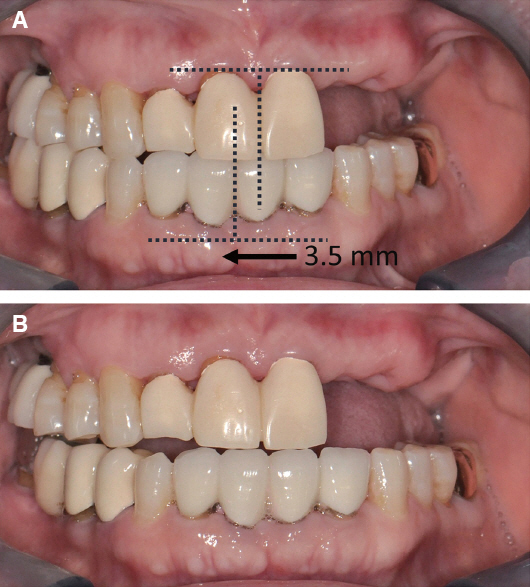
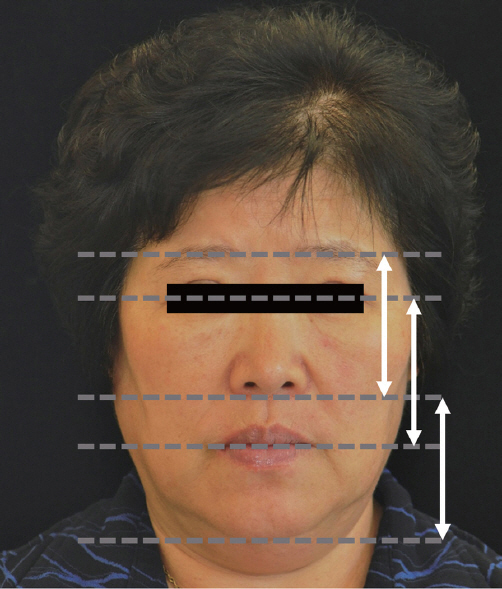
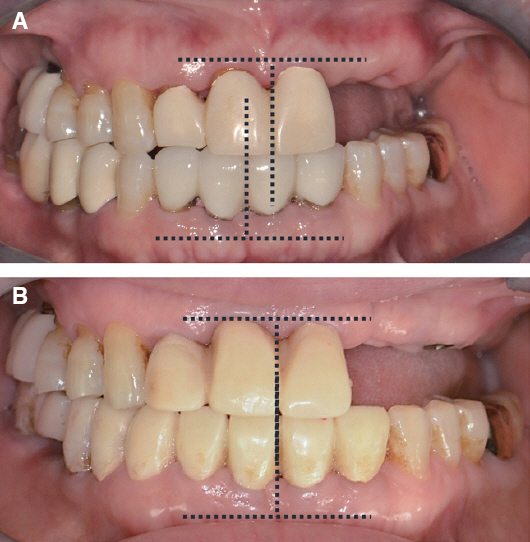
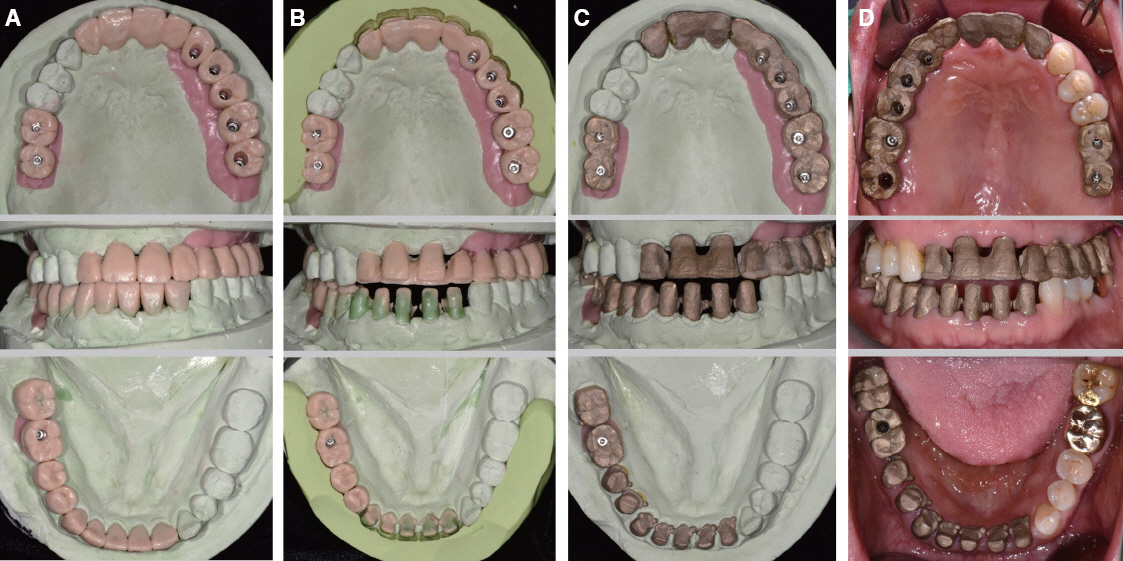
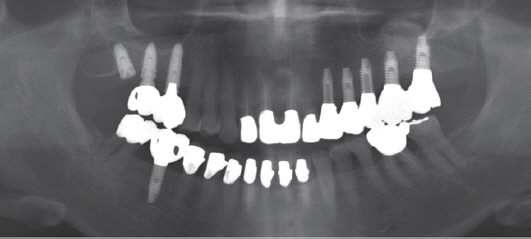
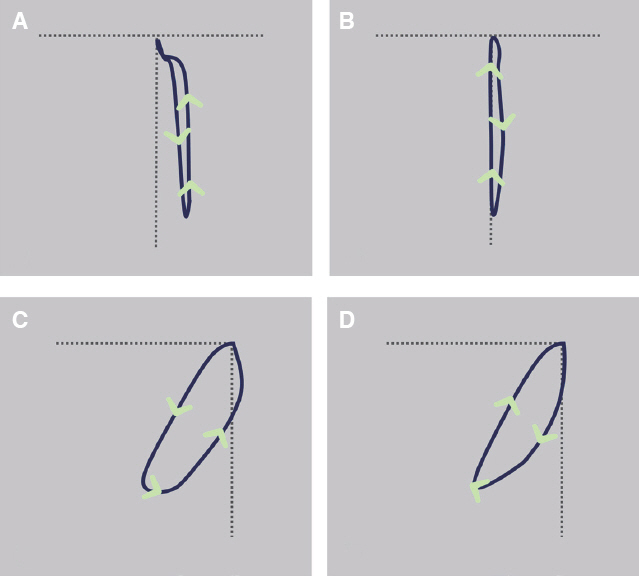
- Centric occlusion-maximum intercuspation (CO-MI) discrepancy is one of main causes of evoking premature contact and resultant mandibular shift. These non-physiological conditions can induce temporomandibular disease, periodontitis, and non-carious cervical lesion. Therefore, if CO-MI discrepancy exists in patients who need extensive prosthetic rehabilitation, it must be corrected and then physiological occlusion must be restored. This report describes the treatment procedure of removing CO-MI discrepancy and prosthetic rehabilitation in a patient with 3.5 mm discrepancy, multiple caries and periodontitis. Proper mandibular position and modified opening & closing movement were confirmed by ARCUSdigma II and transcranial radiograph.
Figure
Reference
-
References
1. The glossary of prosthodontic terms. J Prosthet Dent. 2005; 94:10–92. DOI: 10.1016/j.prosdent.2005.03.013.2. Pullinger AG, Seligman DA, Gornbein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res. 1993; 72:968–79. DOI: 10.1177/00220345930720061301. PMID: 8496480.3. Landi N, Manfredini D, Tognini F, Romagnoli M, Bosco M. Quantification of the relative risk of multiple occlusal variables for muscle disorders of the stomatognathic system. J Prosthet Dent. 2004; 92:190–5. DOI: 10.1016/j.prosdent.2004.05.013. PMID: 15295330.4. Branschofsky M, Beikler T, Schäfer R, Flemming TF, Lang H. Secondary trauma from occlusion and periodontitis. Quintessence Int. 2011; 42:515–22. PMID: 21519589.5. Harrel SK, Nunn ME. The association of occlusal contacts with the presence of increased periodontal probing depth. J Clin Periodontol. 2009; 36:1035–42. DOI: 10.1111/j.1600-051X.2009.01486.x. PMID: 19930093.6. Brandini DA, Trevisan CL, Panzarini SR, Pedrini D. Clinical evaluation of the association between noncarious cervical lesions and occlusal forces. J Prosthet Dent. 2012; 108:298–303. DOI: 10.1016/S0022-3913(12)60180-2.7. Troeltzsch M, Troeltzsch M, Cronin RJ, Brodine AH, Frankenberger R, Messlinger K. Prevalence and association of headaches, temporomandibular joint disorders, and occlusal interferences. J Prosthet Dent. 2011; 105:410–7. DOI: 10.1016/S0022-3913(11)60084-X.8. Dawson PE. Functional occlusion: from TMJ to smile design. 2007. St. Louis: CV Mosby;p. 4–9. PMID: 17906220.9. Ehrlich J, Hochman N, Yaffe A. The masticatory pattern as an adjunct for diagnosis and treatment. J Oral Rehabil. 1992; 19:393–8. DOI: 10.1111/j.1365-2842.1992.tb01581.x. PMID: 1432354.10. Yoshida E, Fueki K, Igarashi Y. Association between food mixing ability and mandibular movements during chewing of a wax cube. J Oral Rehabil. 2007; 34:791–9. DOI: 10.1111/j.1365-2842.2007.01743.x. PMID: 17919244.11. Park JM, Kim HJ, Park EJ, Kim MR, Kim SJ. Three dimensional finite element analysis of the stress distribution around the mandibular posterior implant during non-working movement according to the amount of cantilever. J Adv Prosthodont. 2014; 6:361–71. DOI: 10.4047/jap.2014.6.5.361. PMID: 25352958. PMCID: PMC4211052.12. Aglietta M, Siciliano VI, Zwahlen M, Brägger U, Pjetursson BE, Lang NP, Salvi GE. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. Clin Oral Implants Res. 2009; 20:44151. DOI: 10.1111/j.1600-0501.2009.01706.x. PMID: 19522975.13. Zurdo J, Romão C, Wennström JL. Survival and complication rates of implant-supported fixed partial dentures with cantilevers: a systematic review. Clin Oral Implants Res. 2009; 20(Suppl4):59–66. DOI: 10.1111/j.1600-0501.2009.01773.x. PMID: 19663951.14. Salama MA, Salama H, Garber DA. Guidelines for aesthetic restorative options and implant site enhancement: the utilization of orthodontic extrusion. Pract Proced Aesthet Dent. 2002; 14:125–130.15. Hellsing G. Occlusal adjustment and occlusal stability. J Prosthet Dent. 1988; 59:696–702. DOI: 10.1016/0022-3913(88)90385-X.16. Kirveskari P. Assessment of occlusal stability by measuring contact time and centric slide. J Oral Rehabil. 1999; 26:763–6. DOI: 10.1046/j.1365-2842.1999.00483.x. PMID: 10564430.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rehabilitation of a patient with non-syndromic partial oligodontia
- Rehabilitation of the Bilateral Upper Extremity Amputees
- Prosthetic ambulation in a paraplegic patient with a transfemoral amputation and radial nerve palsy
- Prosthetic Gait Training in Individuals with Pathologic Conditions and Associated Pain on the Non-Amputated Side
- Prosthetic rehabilitation for a glossectomy patient: a clinical report