J Clin Neurol.
2015 Oct;11(4):349-357. 10.3988/jcn.2015.11.4.349.
Dysphagia May Be an Independent Marker of Poor Outcome in Acute Lateral Medullary Infarction
- Affiliations
-
- 1Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea. mkhan@snu.ac.kr
- 2Department of Neurology, Seoul Metropolitan Boramae Hospital, Seoul, Korea.
- 3Department of Neurology, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 4Department of Neurology, Chungbuk National University, Chungju, Korea.
- 5Department of Neurology, Seoul Medical Center, Seoul, Korea.
- 6Department of Neurology, Asan Medical Center, Seoul, Korea.
- KMID: 2179754
- DOI: http://doi.org/10.3988/jcn.2015.11.4.349
Abstract
- BACKGROUND AND PURPOSE
The functional recovery after the lateral medullary infarction (LMI) is usually good. Little is known about the prognostic factors associated with poor outcome following acute LMI. The aim of this study was to identify the factors associated with poor long-term outcome after acute LMI, based on experiences at a single center over 11 years.
METHODS
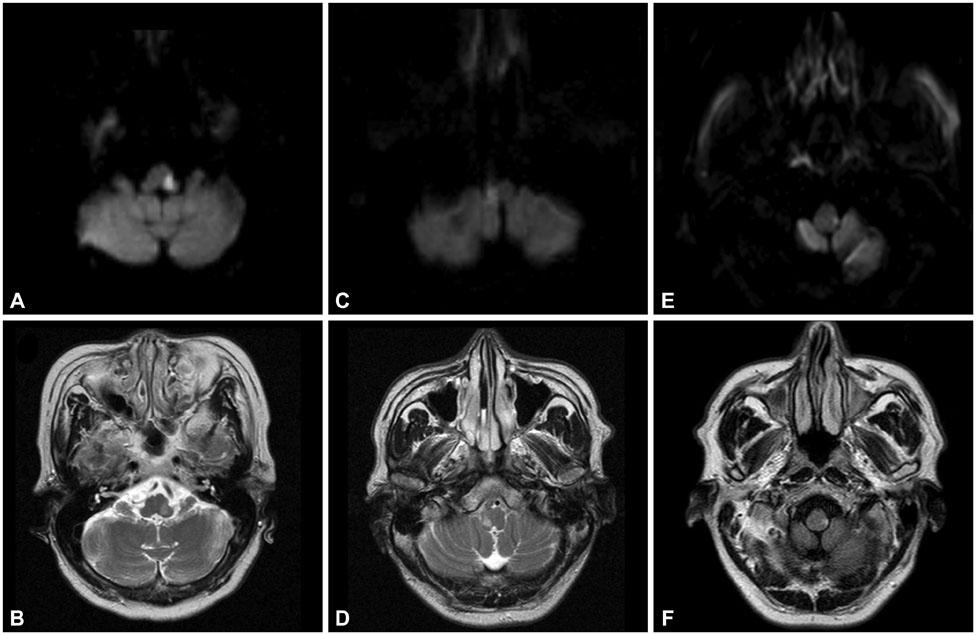
A consecutive series of 157 patients with acute LMI who were admitted within 7 days after symptom onset was evaluated retrospectively. Clinical symptoms were assessed within 1 day after admission, and outcomes were evaluated over a 1-year period after the initial event. The lesions were classified into three vertical types (rostral, middle, and caudal), and the patients were divided into two groups according to the outcome at 1 year: favorable [modified Rankin Scale (mRS) score < or =1] and unfavorable (mRS score > or =2).
RESULTS
Of the 157 patients, 93 (59.2%) had a favorable outcome. Older age, hypertension, dysphagia, requirement for intensive care, and pneumonia were significantly more prevalent in the unfavorable outcome group. The frequencies of intensive care (13%) and mortality (16.7%) were significantly higher in the rostral lesion (p=0.002 and p=0.002). Conditional logistic regression analysis revealed that older age and initial dysphagia were independently related to an unfavorable outcome at 1 year [odds ratio (OR)=1.04, 95% confidence interval (95% CI)=1.001-1.087, p=0.049; OR=2.46, 95% CI=1.04-5.84, p=0.041].
CONCLUSIONS
These results suggest that older age and initial dysphagia in the acute phase are independent risk factors for poor long-term prognosis after acute LMI.
Keyword
MeSH Terms
Figure
Reference
-
1. Hankey GJ, Spiesser J, Hakimi Z, Bego G, Carita P, Gabriel S. Rate, degree, and predictors of recovery from disability following ischemic stroke. Neurology. 2007; 68:1583–1587.
Article2. König IR, Ziegler A, Bluhmki E, Hacke W, Bath PM, Sacco RL, et al. Predicting long-term outcome after acute ischemic stroke: a simple index works in patients from controlled clinical trials. Stroke. 2008; 39:1821–1826.3. Sumer MM, Ozdemir I, Tascilar N. Predictors of outcome after acute ischemic stroke. Acta Neurol Scand. 2003; 107:276–280.
Article4. Nedeltchev K, der Maur TA, Georgiadis D, Arnold M, Caso V, Mattle HP, et al. Ischaemic stroke in young adults: predictors of outcome and recurrence. J Neurol Neurosurg Psychiatry. 2005; 76:191–195.
Article5. Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003; 126(Pt 8):1864–1872.
Article6. Kim JS, Choi-Kwon S. Sensory sequelae of medullary infarction: differences between lateral and medial medullary syndrome. Stroke. 1999; 30:2697–2703.7. Norrving B, Cronqvist S. Lateral medullary infarction: prognosis in an unselected series. Neurology. 1991; 41(2(Pt 1)):244–248.8. Caplan LR. Bilateral distal vertebral artery occlusion. Neurology. 1983; 33:552–558.
Article9. Nelles G, Contois KA, Valente SL, Higgins JL, Jacobs DH, Kaplan JD, et al. Recovery following lateral medullary infarction. Neurology. 1998; 50:1418–1422.
Article10. Aydogdu I, Ertekin C, Tarlaci S, Turman B, Kiylioglu N, Secil Y. Dysphagia in lateral medullary infarction (Wallenberg's syndrome): an acute disconnection syndrome in premotor neurons related to swallowing activity? Stroke. 2001; 32:2081–2087.
Article11. Caplan LR, Pessin MS, Scott RM, Yarnell P. Poor outcome after lateral medullary infarcts. Neurology. 1986; 36:1510–1513.
Article12. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42:1206–1252.
Article13. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001; 285:2486–2497.14. Vijan S. Type 2 diabetes. Ann Intern Med. 2010; 152:ITC31–ITC15. quiz ITC316
Article15. Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000; 15:19–30.
Article16. Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia. 2001; 16:7–18.
Article17. Sulter G, Steen C, De Keyser J. Use of the Barthel index and modified Rankin scale in acute stroke trials. Stroke. 1999; 30:1538–1541.
Article18. Hoare Z, Lim WS. Pneumonia: update on diagnosis and management. BMJ. 2006; 332:1077–1079.
Article19. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article20. Hosoya T, Nagahata M, Yamaguchi K. Prevalence of vertebral artery dissection in Wallenberg syndrome: neuroradiological analysis of 93 patients in the Tohoku District, Japan. Radiat Med. 1996; 14:241–246.21. Hosoya T, Watanabe N, Yamaguchi K, Kubota H, Onodera Y. Intracranial vertebral artery dissection in Wallenberg syndrome. AJNR Am J Neuroradiol. 1994; 15:1161–1165.22. Shin JH, Suh DC, Choi CG, Leei HK. Vertebral artery dissection: spectrum of imaging findings with emphasis on angiography and correlation with clinical presentation. Radiographics. 2000; 20:1687–1696.
Article23. Kim JS, Lee JH, Suh DC, Lee MC. Spectrum of lateral medullary syndrome. Correlation between clinical findings and magnetic resonance imaging in 33 subjects. Stroke. 1994; 25:1405–1410.
Article24. Leno C, Berciano J, Combarros O, Polo JM, Pascual J, Quintana F, et al. A prospective study of stroke in young adults in Cantabria, Spain. Stroke. 1993; 24:792–795.
Article25. Leys D, Bandu L, Hénon H, Lucas C, Mounier-Vehier F, Rondepierre P, et al. Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology. 2002; 59:26–33.
Article26. Dash D, Bhashin A, Pandit AK, Tripathi M, Bhatia R, Prasad K, et al. Risk factors and etiologies of ischemic strokes in young patients: a tertiary hospital study in north India. J Stroke. 2014; 16:173–177.
Article27. Kim H, Chung CS, Lee KH, Robbins J. Aspiration subsequent to a pure medullary infarction: lesion sites, clinical variables, and outcome. Arch Neurol. 2000; 57:478–483.
Article28. Kwon M, Lee JH, Kim JS. Dysphagia in unilateral medullary infarction: lateral vs medial lesions. Neurology. 2005; 65:714–718.
Article29. Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989; 52:236–241.
Article30. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204.31. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763.32. Bours GJ, Speyer R, Lemmens J, Limburg M, de Wit R. Bedside screening tests vs. videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs. 2009; 65:477–493.
Article33. Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996; 27:1028–1032.
Article34. Badan I, Buchhold B, Hamm A, Gratz M, Walker LC, Platt D, et al. Accelerated glial reactivity to stroke in aged rats correlates with reduced functional recovery. J Cereb Blood Flow Metab. 2003; 23:845–854.
Article35. Petcu EB, Sfredel V, Platt D, Herndon JG, Kessler C, Popa-Wagner A. Cellular and molecular events underlying the dysregulated response of the aged brain to stroke: a mini-review. Gerontology. 2008; 54:6–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolated Axial Lateropulsion in Lateral Medullary Infarction
- Pure Limb Ataxia as Isolated Manifestation in Lateral Medullary Infarction
- Lateral Medullary Infarction with Ipsilesional Gaze-Evoked and Head-Shaking Nystagmus
- A Case Of Lateral Medullary Infarction Presenting as Isolated Dysphagia with Unilateral Vocal Fold Paralysis
- Sudden Unexpected Death after Lateral Medullary Infarction