J Clin Neurol.
2013 Apr;9(2):83-90. 10.3988/jcn.2013.9.2.83.
Follow-Up of 58 Traumatic Carotid-Cavernous Fistulas after Endovascular Detachable-Balloon Embolization at a Single Center
- Affiliations
-
- 1Department of Radiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China. hbshi346@163.com
- KMID: 2179166
- DOI: http://doi.org/10.3988/jcn.2013.9.2.83
Abstract
- BACKGROUND AND PURPOSE
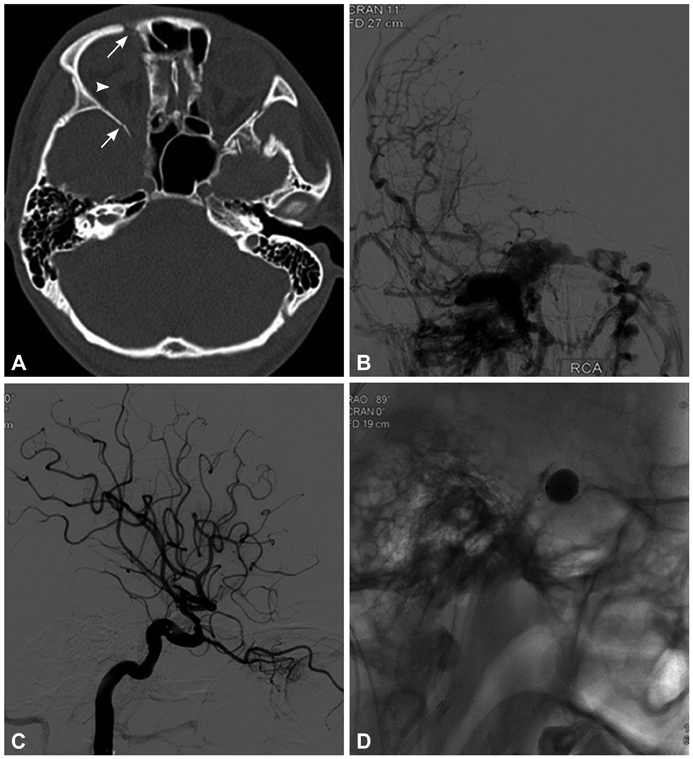
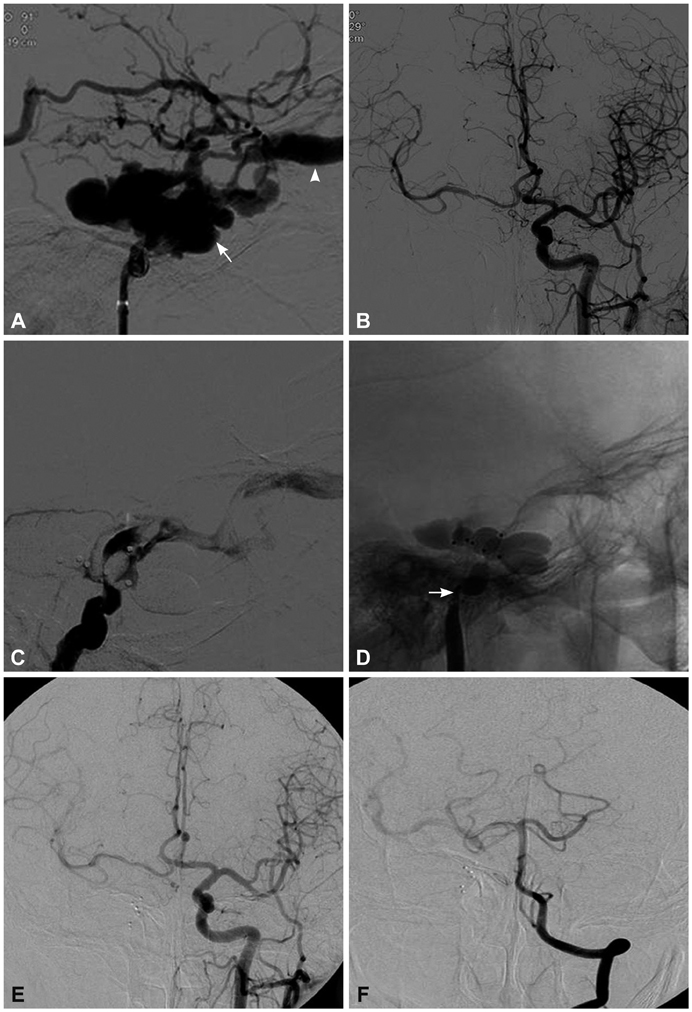
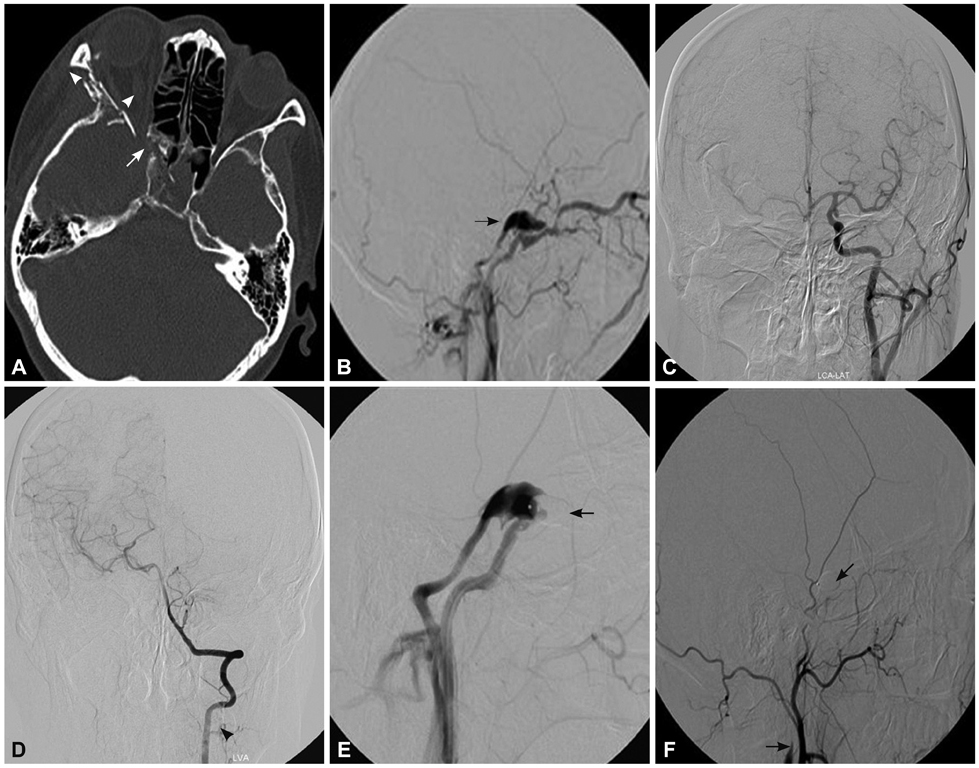
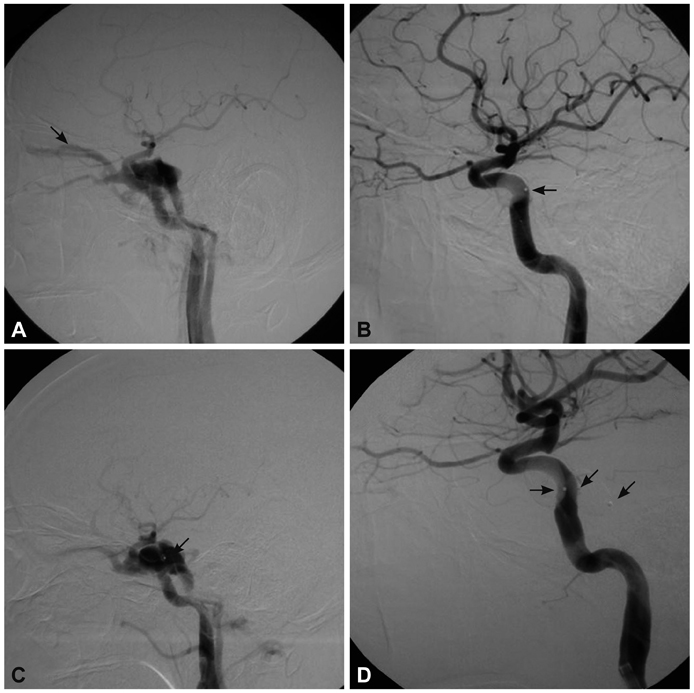
This study evaluated the clinical value of detachable-balloon embolization for traumatic carotid-cavernous fistula (TCCF), focusing on the frequency, risk factors, and retreatment of recurrence.
METHODS
Fifty-eight patients with TCCF underwent transarterial detachable-balloon embolization between October 2004 and March 2011. The clinical follow-up was performed every 3 months until up to 3 years postprocedure. Each patient was placed in either the recurrence group or the nonrecurrence group according to whether a recurrence developed after the first procedure. The relevant factors including gender, fistula location, interval between trauma and the interventional procedure, blood flow in the carotid-cavernous fistula, number of balloons, and whether the internal carotid artery (ICA) was sacrificed were evaluated.
RESULTS
All 58 TCCFs were successfully treated with transarterial balloon embolization, including 7 patients with ICA sacrifice. Recurrent fistulas occurred in seven patients during the follow-up period. Univariate analysis indicated that the interval between trauma and the interventional procedure (p=0.006) might be the main factor related to the recurrence of TCCF. The second treatments involved ICA sacrifice in two patients, fistula embolization with balloons in four patients, and placement of a covered stent in one patient.
CONCLUSIONS
Detachable balloons can still serve as the first-line treatment for TCCFs and recurrent TCCFs despite having a nonnegligible recurrence rate. Shortening the interval between trauma and the interventional procedure may reduce the risk of recurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Barnwell SL, O'Neill OR. Endovascular therapy of carotid cavernous fistulas. Neurosurg Clin N Am. 1994. 5:485–495.
Article2. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985. 62:248–256.
Article3. Serbinenko FA. Balloon catheterization and occlusion of major cerebral vessels. J Neurosurg. 1974. 41:125–145.
Article4. Lewis AI, Tomsick TA, Tew JM Jr. Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons. Neurosurgery. 1995. 36:239–245.5. Luo CB, Teng MM, Chang FC, Chang CY. Transarterial balloon-assisted n-butyl-2-cyanoacrylate embolization of direct carotid cavernous fistulas. AJNR Am J Neuroradiol. 2006. 27:1535–1540.6. Yoshida K, Melake M, Oishi H, Yamamoto M, Arai H. Transvenous embolization of dural carotid cavernous fistulas: a series of 44 consecutive patients. AJNR Am J Neuroradiol. 2010. 31:651–655.
Article7. Archondakis E, Pero G, Valvassori L, Boccardi E, Scialfa G. Angiographic follow-up of traumatic carotid cavernous fistulas treated with endovascular stent graft placement. AJNR Am J Neuroradiol. 2007. 28:342–347.8. Wang C, Xie X, You C, Zhang C, Cheng M, He M, et al. Placement of covered stents for the treatment of direct carotid cavernous fistulas. AJNR Am J Neuroradiol. 2009. 30:1342–1346.
Article9. Lasjaunias P, Santoyo-Vazquez A. Segmental agenesis of the internal carotid artery: angiographic aspects with embryological discussion. Anat Clin. 1984. 6:133–141.
Article10. van Rooij WJ, Sluzewski M, Beute GN. Ruptured cavernous sinus aneurysms causing carotid cavernous fistula: incidence, clinical presentation, treatment, and outcome. AJNR Am J Neuroradiol. 2006. 27:185–189.11. Wang W, Li YD, Li MH, Tan HQ, Gu BX, Wang J, et al. Endovascular treatment of post-traumatic direct carotid-cavernous fistulas: A single-center experience. J Clin Neurosci. 2011. 18:24–28.
Article12. Gemmete JJ, Chaudhary N, Pandey A, Ansari S. Treatment of carotid cavernous fistulas. Curr Treat Options Neurol. 2010. 12:43–53.
Article13. Luo CB, Teng MM, Yen DH, Chang FC, Lirng JF, Chang CY. Endovascular embolization of recurrent traumatic carotid-cavernous fistulas managed previously with detachable balloons. J Trauma. 2004. 56:1214–1220.
Article14. Bavinzski G, Killer M, Gruber A, Richling B. Treatment of post-traumatic carotico-cavernous fistulae using electrolytically detachable coils: technical aspects and preliminary experience. Neuroradiology. 1997. 39:81–85.
Article15. Luo CB, Teng MM, Chang FC, Chang CY. Traumatic indirect carotid cavernous fistulas: angioarchitectures and results of transarterial embolization by liquid adhesives in 11 patients. Surg Neurol. 2009. 71:216–222.
Article16. Li MH, Li YD, Tan HQ, Luo QY, Cheng YS. Treatment of distal internal carotid artery aneurysm with the willis covered stent: a prospective pilot study. Radiology. 2009. 253:470–477.
Article17. Li J, Lan ZG, Xie XD, You C, He M. Traumatic carotid-cavernous fistulas treated with covered stents: experience of 12 cases. World Neurosurg. 2010. 73:514–519.
Article18. Hoit DA, Schirmer CM, Malek AM. Stent graft treatment of cerebrovascular wall defects: intermediate-term clinical and angiographic results. Neurosurgery. 2008. 62:ONS380–ONS388.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central Retinal Vein Occlusion During Embolization for Carotid Cavernous Sinus Fistula
- Endovascular Graft-Stent Placement for Treatment of Traumatic Carotid Cavernous Fistulas
- Treatment of Traumatic Carotid-Cavernous Fistulas using Debrun's Detachable Balloons
- GDC(Guglielmi Detachable Coil) Embolization Used in Carotid-Cavernous Fistula Incompletely Occluded by Detachable Balloon
- Transarterial Guglielmi Detachable Coils Embolization with Stenting for the Treatment of a Traumatic Carotid Cavernous Fistula: Case Report