J Clin Neurol.
2011 Jun;7(2):77-84. 10.3988/jcn.2011.7.2.77.
Burden of Ischemic Stroke in Korea: Analysis of Disability-Adjusted Life Years Lost
- Affiliations
-
- 1Department of Neurology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. nrhks@paik.ac.kr
- 2Social and Preventive Medicine, Hallym University College of Medicine, Chuncheon, Korea.
- 3Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Biostatistics, College of Medicine, Korea University, Seoul, Korea.
- 5Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 6Department of Neurology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
- 7Department of Neurology, The Catholic University of Korea, Seoul St. Mary's Hospital, Seoul, Korea.
- 8Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- KMID: 2178970
- DOI: http://doi.org/10.3988/jcn.2011.7.2.77
Abstract
- BACKGROUND AND PURPOSE
Disability-adjusted life years (DALY), incorporating both disability and mortality, has been widely employed to measure regional and global burdens of stroke. Thus far, the DALY lost to stroke in a population has been estimated using only the crude population-level data; no previous study has incorporated refined data from stroke registries. The aim of this study was to integrate the stroke registry data and the population-level incidence data to project the nationwide DALY lost to ischemic stroke.
METHODS
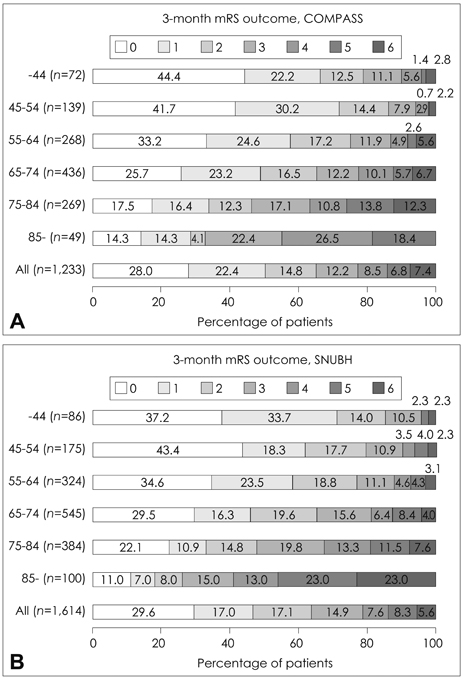
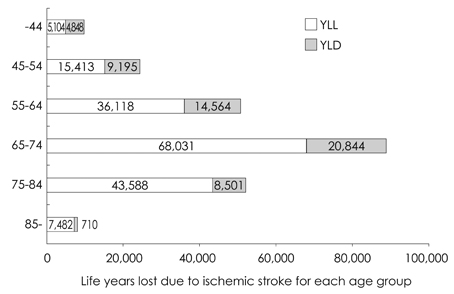
From the data of two large ischemic stroke registries, we derived an average DALY lost due to ischemic stroke for each of the following age groups: <45, 45-54, 55-64, 65-74, 75-84, and > or =85 years. The nationwide ischemic stroke incidence for each age group was extracted from a cardiovascular and cerebrovascular surveillance study that analyzed the 2004 Korean Health Insurance database.
RESULTS
The average DALY lost due to ischemic stroke for the age groups <45, 45-54, 55-64, 65-74, 75-84, and > or =85 years was 5.07, 4.63, 4.35, 3.88, 2.88, and 1.73, respectively. By multiplying the incidence and the average DALY lost, the nationwide DALY lost was determined to be 9,952 for those <45 years, 24,608 for 45-54 years, 50,682 for 55-64 years, 88,875 for 65-74 years, 52,089 for 75-84 years, and 8,192 for > or =85 years, respectively. The projected nationwide DALY lost due to 64,688 ischemic strokes in 2004 was 234,399 (121,482 for men and 113,244 for women), and the DALY lost per 100,000 person-years was 483 (500 for men and 469 for women).
CONCLUSIONS
Incidence data from a population study and DALY values derived from stroke registries can be integrated to provide a more refined projection of the nationwide burden of ischemic stroke. In Korea, more than 230,000 years of healthy life are being lost annually due to ischemic stroke, and hence prompt action is imperative.
Keyword
Figure
Cited by 3 articles
-
Job Stress-attributable Burden of Disease in Korea
Kyungjoon Lee, Inah Kim
J Korean Med Sci. 2018;33(25):. doi: 10.3346/jkms.2018.33.e187.Disability-Adjusted Life Years Analysis: Implications for Stroke Research
Keun-Sik Hong
J Clin Neurol. 2011;7(3):109-114. doi: 10.3988/jcn.2011.7.3.109.Medial Temporal Atrophy and Memory Dysfunction in Poststroke Cognitive Impairment-No Dementia
Beom Joon Kim, Mi-Young Oh, Myung Suk Jang, Moon-Ku Han, Jisung Lee, Juneyoung Lee, Yeonwook Kang, Kyung-Ho Yu, Byung-Chul Lee, Sangyun Kim, Byung-Woo Yoon, Hee-Joon Bae
J Clin Neurol. 2012;8(1):43-50. doi: 10.3988/jcn.2012.8.1.43.
Reference
-
1. Murray CJ. Murray CJL, Lopez AD, editors. Rethinking DALYs. The Global Burden of Disease and Injury Series. 1996. Vol 1. Cambridge, MA: Harvard University Press;1–98.2. Estimate of DALYs by sex, cause, and WHO region. WHO. Accessed 10/26/2010. (http://www.who.int/healthinfo/statistics/gbdwhoregiondaly2002.xls).3. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009. 8:345–354.
Article4. O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010. 376:112–123.5. Truelsen T, Begg S, Mathers C. The global burden of cerebrovascular disease. Accessed Oct/25/2010. (http://www.who.int/healthinfo/statistics/bod_cerebrovasculardiseasestroke.pdf).6. Global Burden of Disease 2004 Update: Disability Weights for diseases and conditions. WHO. Accessed Apr/2/2009. (www.who.int/healthinfo/global_burden_disease/GBD2004_DisabilityWeights.pdf).7. Hong KS, Saver JL. Quantifying the value of stroke disability outcomes: WHO global burden of disease project disability weights for each level of the modified Rankin Scale. Stroke. 2009. 40:3828–3833.
Article8. Hong KS, Saver JL. Years of disability-adjusted life gained as a result of thrombolytic therapy for acute ischemic stroke. Stroke. 2010. 41:471–477.
Article9. Hong KS, Saver JL, Kang DW, Bae HJ, Yu KH, Koo J, et al. Years of optimum health lost due to complications after acute ischemic stroke: disability-adjusted life-years analysis. Stroke. 2010. 41:1758–1765.
Article10. Construction of National Surveillance System for Cardiovascular & Cerebrovascular Diseases. Korean Center for Disease Control. 2006.11. Hong KS, Kang DW, Koo JS, Yu KH, Han MK, Cho YJ, et al. Impact of neurological and medical complications on 3-month outcomes in acute ischaemic stroke. Eur J Neurol. 2008. 15:1324–1331.
Article12. Life Tables for Korea, 2005. KOSIS. Accessed Oct/11/2009. (http://www.kosis.kr/OLAP/Analysis/stat_OLAP.jsp?tbl_id=DT_1B42&org_id=101&vwcd=MT_ZTITLE&path=).13. Eriksson M, Norrving B, Terént A, Stegmayr B. Functional outcome 3 months after stroke predicts long-term survival. Cerebrovasc Dis. 2008. 25:423–429.
Article14. Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P. Oxfordshire Community Stroke Project, the International Stroke Trial (UK). Lothian Stroke Register. Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ. 2008. 336:376–379.
Article15. Fox-Rushby JA, Hanson K. Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis. Health Policy Plan. 2001. 16:326–331.
Article16. Lee H, Yoon SJ, Ahn HS, Moon OR. Estimation of potential health gains from reducing multiple risk factors of stroke in Korea. Public Health. 2007. 121:774–780.
Article17. Lee BC, Roh JK. Korean Stroke Registry. International experience in stroke registries: Korean Stroke Registry. Am J Prev Med. 2006. 31:S243–S245.18. Yu KH, Bae HJ, Kwon SU, Kang DW, Hong KS, Lee YS, et al. Analysis of 10,811 cases with acute ischemic stroke from Korean stroke registry: Hospital-based multicenter prospective registration study. J Korean Neurol Assoc. 2006. 24:535–543.19. Duncan PW, Goldstein LB, Matchar D, Divine GW, Feussner J. Measurement of motor recovery after stroke. Outcome assessment and sample size requirements. Stroke. 1992. 23:1084–1089.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disability-Adjusted Life Years Analysis: Implications for Stroke Research
- Years of Life Lost due to Premature Death in People with Disabilities in Korea: the Korean National Burden of Disease Study Framework
- Measuring the Burden of Disease in Korea Using Disability-Adjusted Life Years (2008–2020)
- The Burden of Stroke in Kurdistan Province, Iran From 2011 to 2017
- Trend of Disease Burden of North Korean Defectors in South Korea Using Disability-adjusted Life Years from 2010 to 2018