J Korean Endocr Soc.
2010 Mar;25(1):61-67. 10.3803/jkes.2010.25.1.61.
A Case of Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Affiliations
-
- 1Department of Internal Medicine, Konyang University Hospital College of Medicine, Korea.
- 2Department of Pathology, Konyang University Hospital College of Medicine, Korea.
- KMID: 2177863
- DOI: http://doi.org/10.3803/jkes.2010.25.1.61
Abstract
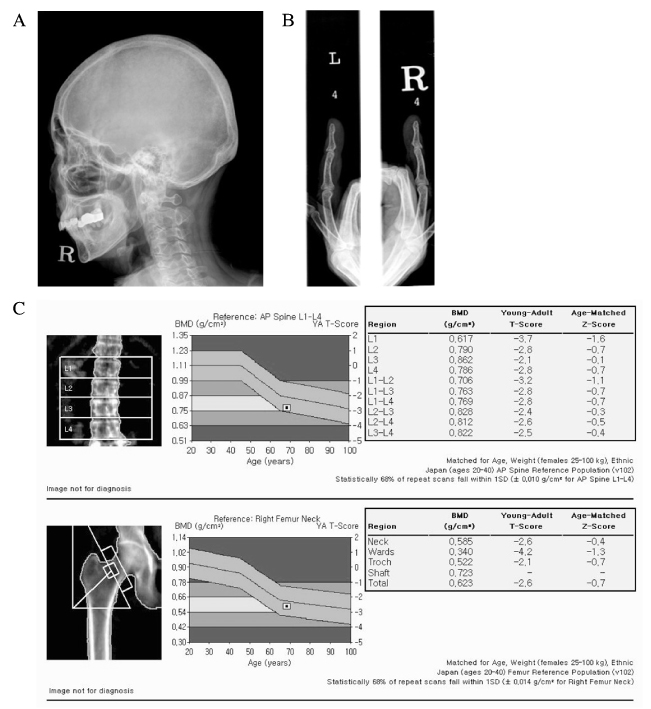
- Primary hyperparathyroidism is usually caused by a parathyroid adenoma, occasionally by primary parathyroid hyperplasia and rarely by parathyroid carcinoma. Coincidental occurrence of thyroid carcinoma in parathyroid adenoma is not uncommon, but synchronous parathyroid and thyroid carcinoma is extremely rare. Here, we describe a case of synchronous parathyroid carcinoma and papillary thyroid carcinoma.
MeSH Terms
Figure
Reference
-
1. Melton LJ 3rd. The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res. 2002. 17:N12–N17.2. Wynne AG, van Heerden J, Carney JA, Fitzpatrick LA. Parathyroid carcinoma: clinical and pathologic features in 43 patients. Medicine (Baltimore). 1992. 71:197–205.3. Shane E. Clinical review 122: Parathyroid carcinoma. J Clin Endocrinol Metab. 2001. 86:485–493.4. Howell VM, Haven CJ, Kahnoski K, Khoo SK, Petillo D, Chen J, Fleuren GJ, Robinson BG, Delbridge LW, Philips J, Nelson AE, Krause U, Hammje K, Dralle H, Hoang-Vu C, Gimm O, Marsh DJ, Morreau H, Teh BT. HRPT2 mutations are associated with malignancy in sporadic parathyroid tumours. J Med Genet. 2003. 40:657–663.5. Shattuck TM, Välimäki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C, Arnold A. Somatic and germ-line mutations of the HRPT2 gene in sporadic parathyroid carcinoma. N Engl J Med. 2003. 349:1722–1729.6. Koea JB, Shaw JH. Parathyroid cancer: biology and management. Surg Oncol. 1999. 8:155–165.7. Savli H, Sevinc A, Sari R, Ozen S, Buyukberber S, Ertas E. Occult parathyroid carcinoma in a patient with papillary thyroid carcinoma and Hashimoto's thyroiditis. J Endocrinol Invest. 2001. 24:42–44.8. Schoretsanitis G, Melissas J, Kafousi M, Karkavitsas N, Tsiftsis DD. Synchronous parathyroid and papillary thyroid carcinoma: a case report. Am J Otolaryngol. 2002. 23:382–385.9. Chang HS, Yoon JH, Chung WY, Park CS. Coexistence of parathyroid and papillary thyroid carcinoma. J Korean Surg Soc. 2004. 66:147–152.10. Burmeister LA, Sandberg M, Carty SE, Watson CG. Thyroid carcinoma found at parathyroidectomy: association with primary, secondary, and tertiary hyperparathyroidism. Cancer. 1997. 79:1611–1616.11. Leitha T, Staudenherz A. Concomitant hyperparathyroidism and nonmedullary thyroid cancer, with a review of the literature. Clin Nucl Med. 2003. 28:113–117.12. Pomares FJ, Canas R, Rodriguez JM, Hernandez AM, Parrilla P, Tebar FJ. Differences between sporadic and multiple endocrine neoplasia type 2A phaeochromocytoma. Clin Endocrinol(Oxf). 1998. 48:195–200.13. Schneider AB, Sarne DH. Long-term risks for thyroid cancer and other neoplasms after exposure to radiation. Nat Clin Pract Endocrinol Metab. 2005. 1:82–91.14. Wermers RA, Khosla S, Atkinson EJ, Achenbach SJ, Oberg AL, Grant CS, Melton LJ 3rd. Incidence of primary hyperparathyroidism in Rochester, Minnesota, 1993-2001: an update on the changing epidemiology of the disease. J Bone Miner Res. 2006. 21:171–177.15. Obara T, Fujimoto Y. Diagnosis and treatment of patients with parathyroid carcinoma: an update and review. World J Surg. 1991. 15:738–744.16. Bondeson L, Sandelin K, Grimelius L. Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol. 1993. 17:820–829.17. Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. 2007. 109:1736–1741.18. Hoelting T, Weber T, Werner J, Herfarth C. Surgical treatment of parathyroid carcinoma (Review). Oncol Rep. 2001. 8:931–934.19. Brasier AR, Nussbaum SR. Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med. 1988. 84:654–660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coexistence of Parathyroid and Papillary Thyroid Carcinoma
- Coexistence of parathyroid adenoma and papillary thyroid carcinoma
- Synchronous Parathyroid Adenoma and Papillary Thyroid Carcinoma
- Synchronous parathyroid carcinoma and papillary thyroid carcinoma in a patient with long-standing schizophrenia
- A Case of Papillary Thyroid Cancer Coexisting with Thyroid Tuberculosis