J Breast Cancer.
2011 Dec;14(4):253-261. 10.4048/jbc.2011.14.4.253.
Oncoplastic Surgical Techniques for Personalized Breast Conserving Surgery in Breast Cancer Patient with Small to Moderate Sized Breast
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Kyungpook National University College of Medicine, Daegu, Korea.
- 2Department of Surgery, Kyungpook National University College of Medicine, Daegu, Korea. phy123@knu.ac.kr
- KMID: 2175717
- DOI: http://doi.org/10.4048/jbc.2011.14.4.253
Abstract
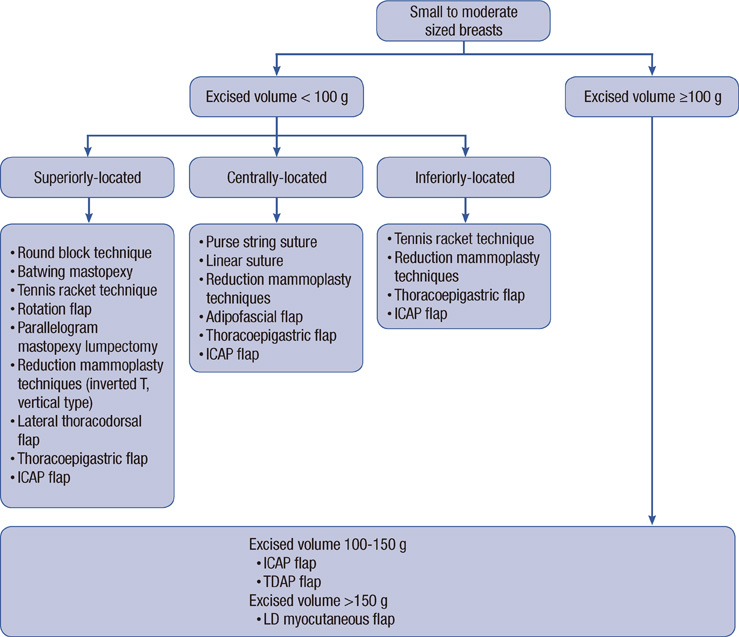
- Oncoplastic surgery has revolutionized the field of breast conserving surgery (BCS). The final aims of this technique are to obtain an adequate resection margin that will reduce the rate of local recurrence while simultaneously improving cosmetic outcomes. To obtain successful results after oncoplastic surgery, it is imperative that patients be risk-stratified based on risk factors associated with positive margins, that relevant imaging studies be reviewed, and that the confirmation of negative margins be confirmed during the initial operation. Patients who had small- to moderate-sized breasts are the most likely to be dissatisfied with the cosmetic outcome of surgery, even if the defect is small; therefore, oncoplastic surgery in this population is warranted. Reconstruction of the remaining breast tissue is divided into volume displacement and volume replacement techniques. The use of the various oncoplastic surgeries is based on tumor location and excised breast volume. If the excised volume is less than 100 g, the tumor location is used to determine which technique should be used, with the most commonly used technique being volume displacement. However, if the excised volume is greater than 100 g, the volume replacement method is generally used, and in cases where more than 150 g is excised, the latissimus dorsi myocutaneous flap may be used to obtain a pleasing cosmetic result. The local recurrence rate after oncoplastic surgery was lower than that of conventional BCS, as oncoplastic surgery reduced the rate of positive resection margins by resecting a wider section of glandular tissue. If the surgeon understands the advantages and disadvantages of oncoplastic surgery, and the multidisciplinary breast team is able to successfully collaborate, then the success rate of BCS with partial breast reconstruction can be increased while also yielding a cosmetically appealing outcome.
MeSH Terms
Figure
Cited by 2 articles
-
Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 1): Volume Displacement
Jung Dug Yang, Jeong Woo Lee, Young Kyoo Cho, Wan Wook Kim, Seung Ook Hwang, Jin Hyang Jung, Ho Yong Park
J Breast Cancer. 2012;15(1):1-6. doi: 10.4048/jbc.2012.15.1.1.Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 2): Volume Replacement
Jung Dug Yang, Jeong Woo Lee, Young Kyoo Cho, Wan Wook Kim, Seung Ook Hwang, Jin Hyang Jung, Ho Yong Park
J Breast Cancer. 2012;15(1):7-14. doi: 10.4048/jbc.2012.15.1.7.
Reference
-
1. Arriagada R, Lê MG, Guinebretiore JM, Dunant A, Rochard F, Tursz T. Late local recurrences in a randomised trial comparing conservative treatment with total mastectomy in early breast cancer patients. Ann Oncol. 2003. 14:1617–1622.
Article2. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002. 347:1233–1241.
Article3. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002. 347:1227–1232.
Article4. Al-Ghazal SK, Blamey RW. Cosmetic assessment of breast-conserving surgery for primary breast cancer. Breast. 1999. 8:162–168.
Article5. Clough KB, Cuminet J, Fitoussi A, Nos C, Mosseri V. Cosmetic sequelae after conservative treatment for breast cancer: classification and results of surgical correction. Ann Plast Surg. 1998. 41:471–481.
Article6. Pleijhuis RG, Graafland M, de Vries J, Bart J, de Jong JS, van Dam GM. Obtaining adequate surgical margins in breast-conserving therapy for patients with early-stage breast cancer: current modalities and future directions. Ann Surg Oncol. 2009. 16:2717–2730.
Article7. Cho KR, Seo BK, Kim CH, Whang KW, Kim YH, Kim BH, et al. Noncalcified ductal carcinoma in situ: ultrasound and mammographic findings correlated with histological findings. Yonsei Med J. 2008. 49:103–110.
Article8. Ikeda DM, Andersson I. Ductal carcinoma in situ: atypical mammographic appearances. Radiology. 1989. 172:661–666.
Article9. Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2008. 17:748–757.
Article10. Kaplan SS. Clinical utility of bilateral whole-breast US in the evaluation of women with dense breast tissue. Radiology. 2001. 221:641–649.
Article11. Kolb TM, Lichy J, Newhouse JH. Occult cancer in women with dense breasts: detection with screening US--diagnostic yield and tumor characteristics. Radiology. 1998. 207:191–199.
Article12. Morris EA, Liberman L, Dershaw DD, Kaplan JB, LaTrenta LR, Abramson AF, et al. Preoperative MR imaging-guided needle localization of breast lesions. AJR Am J Roentgenol. 2002. 178:1211–1220.
Article13. Hata T, Takahashi H, Watanabe K, Takahashi M, Taguchi K, Itoh T, et al. Magnetic resonance imaging for preoperative evaluation of breast cancer: a comparative study with mammography and ultrasonography. J Am Coll Surg. 2004. 198:190–197.
Article14. Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RM, Dixon JM, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008. 26:3248–3258.
Article15. Lim HI, Choi JH, Yang JH, Han BK, Lee JE, Lee SK, et al. Does pre-operative breast magnetic resonance imaging in addition to mammography and breast ultrasonography change the operative management of breast carcinoma? Breast Cancer Res Treat. 2010. 119:163–167.
Article16. Avril N, Rosé CA, Schelling M, Dose J, Kuhn W, Bense S, et al. Breast imaging with positron emission tomography and fluorine-18 fluorodeoxyglucose: use and limitations. J Clin Oncol. 2000. 18:3495–3502.
Article17. Walter C, Scheidhauer K, Scharl A, Goering UJ, Theissen P, Kugel H, et al. Clinical and diagnostic value of preoperative MR mammography and FDG-PET in suspicious breast lesions. Eur Radiol. 2003. 13:1651–1656.
Article18. MacDonald S, Taghian AG. Prognostic factors for local control after breast conservation: does margin status still matter? J Clin Oncol. 2009. 27:4929–4930.
Article19. Bulstrode NW, Shrotria S. Prediction of cosmetic outcome following conservative breast surgery using breast volume measurements. Breast. 2001. 10:124–126.
Article20. Bae SG, Yang JD, Lee SY, Chung KH, Chung HY, Cho BC, et al. Oncoplastic techniques for treatment of inferiorly located breast cancer. J Korean Soc Plast Reconstr Surg. 2008. 35:680–686.21. Cendán JC, Coco D, Copeland EM 3rd. Accuracy of intraoperative frozen-section analysis of breast cancer lumpectomy-bed margins. J Am Coll Surg. 2005. 201:194–198.
Article22. Olson TP, Harter J, Muñoz A, Mahvi DM, Breslin T. Frozen section analysis for intraoperative margin assessment during breast-conserving surgery results in low rates of re-excision and local recurrence. Ann Surg Oncol. 2007. 14:2953–2960.
Article23. Haid A, Knauer M, Dunzinger S, Jasarevic Z, Köberle-Wührer R, Schuster A, et al. Intra-operative sonography: a valuable aid during breast-conserving surgery for occult breast cancer. Ann Surg Oncol. 2007. 14:3090–3101.
Article24. Yang JD, Bae SG, Chung HY, Cho BC, Park HY, Jung JH. The usefulness of oncoplastic volume displacement techniques in the superiorly located breast cancers for Korean patients with small to moderate-sized breasts. Ann Plast Surg. 2011. 67:474–480.
Article25. Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol. 2005. 6:145–157.
Article26. Losken A, Hamdi M. Partial breast reconstruction: current perspectives. Plast Reconstr Surg. 2009. 124:722–736.
Article27. Almasad JK, Salah B. Breast reconstruction by local flaps after conserving surgery for breast cancer: an added asset to oncoplastic techniques. Breast J. 2008. 14:340–344.
Article28. Petit JY, De Lorenzi F, Rietjens M, Intra M, Martella S, Garusi C, et al. Technical tricks to improve the cosmetic results of breast-conserving treatment. Breast. 2007. 16:13–16.
Article29. Veronesi U, Volterrani F, Luini A, Saccozzi R, Del Vecchio M, Zucali R, et al. Quadrantectomy versus lumpectomy for small size breast cancer. Eur J Cancer. 1990. 26:671–673.
Article30. Rigotti G, Marchi A, Galiè M, Baroni G, Benati D, Krampera M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg. 2007. 119:1409–1422.
Article31. Losken A, Mackay GJ, Bostwick J 3rd. Nipple reconstruction using the C-V flap technique: a long-term evaluation. Plast Reconstr Surg. 2001. 108:361–369.
Article32. Dolmans GH, van de Kar AL, van Rappard JH, Hoogbergen MM. Nipple reconstruction: the "Hammond" flap. Plast Reconstr Surg. 2008. 121:353–354.
Article33. Kronowitz SJ, Kuerer HM, Buchholz TA, Valero V, Hunt KK. A management algorithm and practical oncoplastic surgical techniques for repairing partial mastectomy defects. Plast Reconstr Surg. 2008. 122:1631–1647.
Article34. Losken A, Styblo TM, Carlson GW, Jones GE, Amerson BJ. Management algorithm and outcome evaluation of partial mastectomy defects treated using reduction or mastopexy techniques. Ann Plast Surg. 2007. 59:235–242.
Article35. Munhoz AM, Aldrighi CM, Montag E, Arruda E, Brasil JA, Filassi JR, et al. Outcome analysis of immediate and delayed conservative breast surgery reconstruction with mastopexy and reduction mammaplasty techniques. Ann Plast Surg. 2011. 67:220–225.
Article36. Rietjens M, Urban CA, Rey PC, Mazzarol G, Maisonneuve P, Garusi C, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007. 16:387–395.
Article37. Urban C, Lima R, Schunemann E, Spautz C, Rabinovich I, Anselmi K. Oncoplastic principles in breast conserving surgery. Breast. 2011. 20:Suppl 3. S92–S95.
Article38. Rainsbury RM. Surgery insight: oncoplastic breast-conserving reconstruction--indications, benefits, choices and outcomes. Nat Clin Pract Oncol. 2007. 4:657–664.
Article39. Hassa A, Curtis MS, Colakoglu S, Tobias AM, Lee BT. Early results using ultrasound-assisted liposuction as a treatment for fat necrosis in breast reconstruction. Plast Reconstr Surg. 2010. 126:762–768.
Article40. Trombetta M, Valakh V, Julian TB, Werts ED, Parda D. Mammary fat necrosis following radiotherapy in the conservative management of localized breast cancer: does it matter? Radiother Oncol. 2010. 97:92–94.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 1): Volume Displacement
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 2): Volume Replacement
- Oncoplastic Breast Surgery
- Usefulness of Oncoplastic Volume Replacement Techniques after Breast Conserving Surgery in Small to Moderate-sized Breasts
- Oncoplastic Technique Combining an Adipofascial Flap with an Extended Glandular Flap for the Breast-Conserving Reconstruction of Small Dense Breasts