J Breast Cancer.
2011 Mar;14(1):52-57. 10.4048/jbc.2011.14.1.52.
The Feasibility of Endoscopy-Assisted Breast Conservation Surgery for Patients with Early Breast Cancer
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. bwpark@yuhs.ac
- KMID: 2175643
- DOI: http://doi.org/10.4048/jbc.2011.14.1.52
Abstract
- PURPOSE
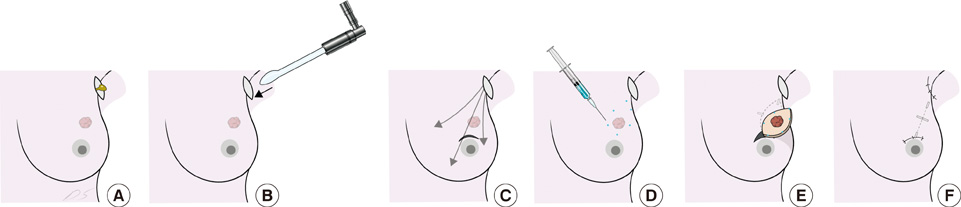
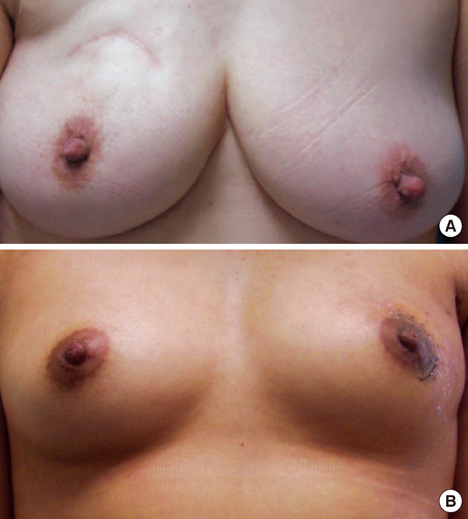
Breast conservation surgery (BCS) has become a standard treatment method for patients with early breast cancer. Endoscopy-assisted BCS (EABCS) can be performed through an inconspicuous periareolar and a small axillary incision for sentinel node biopsy, which may give better cosmetic outcomes than conventional BCS skin incisions. This study was designed to evaluate the feasibility of EABCS for patients with early breast cancer.
METHODS
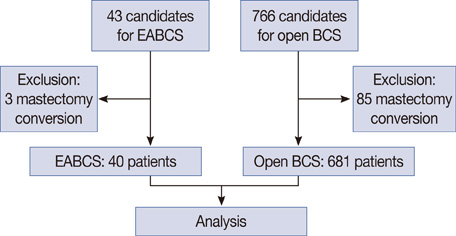
Forty-three patients were candidates for EABCS, and EABCS was performed in 40 patients with breast cancer between January 2008 and July 2010. Their clinicopathological features were retrospectively analyzed. Operative time, margin status, complications, and relapse-free survival were compared with those of patients treated by conventional BCS and who were treated at the same institute during the same period.
RESULTS
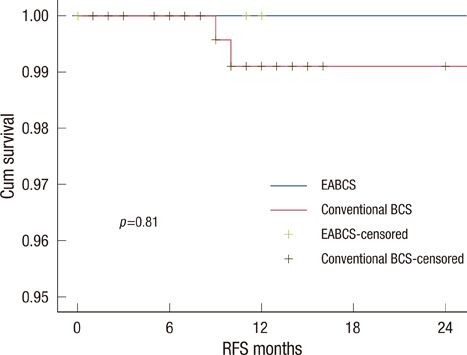
The most common lesion site of the EABCS and conventional BCS groups was the upper area of the breast. Tumor size in all patients was less than 4 cm (range, 0.4-3.7 cm), and nodal involvement was found in eight (20%) patients in the BCS group. The mean operative time was 110 minutes for the EABCS group and 107 minutes for the conventional BCS group, and those were not significantly different. No significant difference in frozen or final margin status was observed between the EABCS and conventional BCS groups. Relapse-free survival was statistically equivalent between the groups with a median follow-up of 12 months. Postoperative complications occurred in five cases in four patients with EABCS, which was not significantly different from conventional BCS.
CONCLUSION
Performing EABCS in patients with early breast cancer seems to be feasible and safe. Further study with a longer-term follow-up may be needed to confirm the clinical value of EABCS.
MeSH Terms
Figure
Reference
-
1. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002. 347:1233–1241.
Article2. Ingram D. Is it time for breast cancer surgeons to embrace endoscopic-assisted mastectomy? ANZ J Surg. 2008. 78:837–838.
Article3. Fukuma E. Endoscopic breast surgery for breast cancer. Nippon Geka Gakkai Zasshi. 2006. 107:64–68.4. Tamaki Y, Miyoshi Y, Noguchi S. Application of endoscopic surgery for breast cancer treatment. Nippon Geka Gakkai Zasshi. 2002. 103:835–838.5. Lee EK, Kook SH, Park YL, Bae WG. Endoscopy-assisted breast-conserving surgery for early breast cancer. World J Surg. 2006. 30:957–964.
Article6. Hong YI, Shin H. Endoscopy-assisted breast conserving surgery for breast cancer: a preliminary clinical experience. J Breast Cancer. 2010. 13:138–146.
Article7. Giordano PA, Rouif M, Laurent B, Mateu J. Endoscopic transaxillary breast augmentation: clinical evaluation of a series of 306 patients over a 9-year period. Aesthet Surg J. 2007. 27:47–54.
Article8. Eaves FF 3rd, Bostwick J 3rd, Nahai F, Murray DR, Styblo TM, Carlson GW. Endoscopic techniques in aesthetic breast surgery. Augmentation, mastectomy, biopsy, capsulotomy, capsulorrhaphy, reduction, mastopexy, and reconstructive techniques. Clin Plast Surg. 1995. 22:683–695.9. Troilius C. Endoscopic transaxillary breast augmentation. Aesthet Surg J. 2004. 24:67–73.
Article10. Yamashita K, Shimizu K. Endoscopic video-assisted breast surgery: procedures and short-term results. J Nippon Med Sch. 2006. 73:193–202.
Article11. Keshtgar MR, Fukuma E. Endoscopic mastectomy: what does the future hold? Womens Health (Lond Engl). 2009. 5:107–109.
Article12. Kitamura K, Ishida M, Inoue H, Kinoshita J, Hashizume M, Sugimachi K. Early results of an endoscope-assisted subcutaneous mastectomy and reconstruction for breast cancer. Surgery. 2002. 131:1 Suppl. S324–S329.
Article13. Owaki T, Yoshinaka H, Ehi K, Kijima Y, Uenosono Y, Shirao K, et al. Endoscopic quadrantectomy for breast cancer with sentinel lymph node navigation via a small axillary incision. Breast. 2005. 14:57–60.
Article14. Nishimura R, Akizuki M, Tashima R, Ootao R. Investigation of factors related to periods to ipsilateral breast tumor recurrence after breast-conserving surgery and measures for preventing recurrence in early breast cancer. Breast Cancer. 2006. 13:152–158.
Article15. Dunne C, Burke JP, Morrow M, Kell MR. Effect of margin status on local recurrence after breast conservation and radiation therapy for ductal carcinoma in situ. J Clin Oncol. 2009. 27:1615–1620.
Article16. Freedman G, Fowble B, Hanlon A, Nicolaou N, Fein D, Hoffman J, et al. Patients with early stage invasive cancer with close or positive margins treated with conservative surgery and radiation have an increased risk of breast recurrence that is delayed by adjuvant systemic therapy. Int J Radiat Oncol Biol Phys. 1999. 44:1005–1015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgery of Breast Cancer during the Last 5 Years: More Sophisticated and Specialized?
- The Highligts of 28th Annual Meeting of San Antonio Breast Cancer Symposium
- Volume Replacement with Polyglactin 910 Mesh for Breast Reconstruction after Endoscopy-Assisted Breast Conserving Surgery for Treating Early Breast Cancer: the Early Results
- Early Screening of Breast Cancer in Korea
- Changes in the Clinical Features of and the Treatment for Breast Cancer