Investig Magn Reson Imaging.
2015 Sep;19(3):153-161. 10.13104/imri.2015.19.3.153.
Useful MRI Features for Distinguishing Benign Peripheral Nerve Sheath Tumors and Myxoid Tumors in the Musculoskeletal System
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Gyeongi-do, Korea. netty0523@gmail.com
- 2Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Gyeongi-do, Korea.
- KMID: 2175607
- DOI: http://doi.org/10.13104/imri.2015.19.3.153
Abstract
- PURPOSE
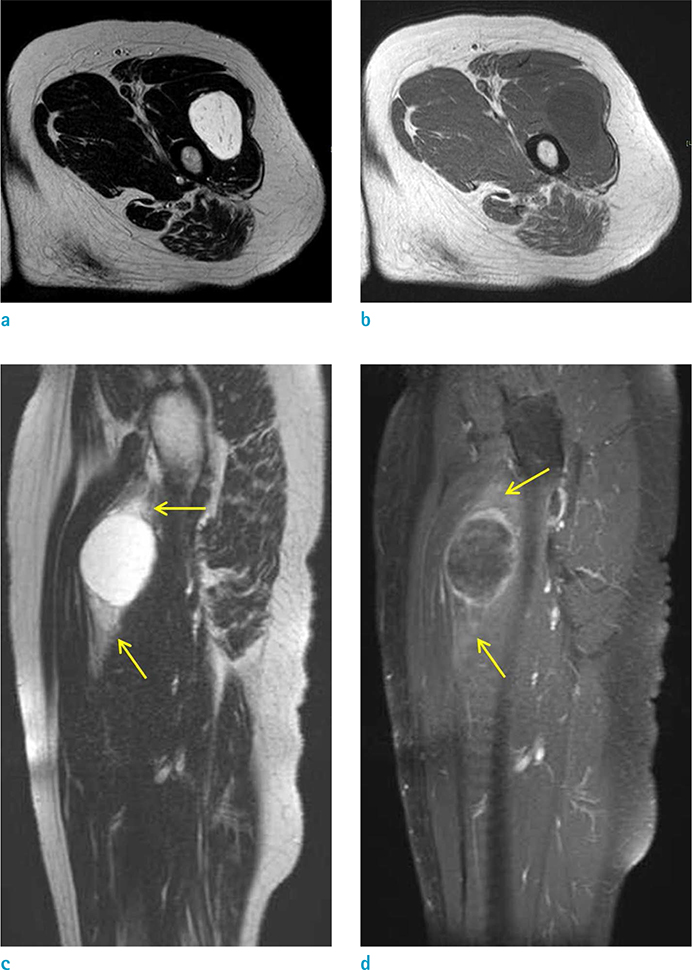
To identify the differential MRI findings between myxoid tumors and benign peripheral nerve sheath tumors (BPNSTs) in the musculoskeletal system.
MATERIALS AND METHODS
The study participants included a total of 35 consecutive patients who underwent MRI between September 2011 and December 2013. The patients were pathologically diagnosed with myxoid tumors (22 patients) or BPNSTs (13 patients). Evaluation was done by two radiologists, based on the following characteristics: size, margin, degree of signal intensity (SI) on T2-weighted images (T2WI), homogeneity of SI on T2WI, enhancement pattern, enhancement homogeneity, presence of cystic portion, internal fat component, presence of fat split sign, presence of target sign, presence of continuation with adjacent neurovascular bundle, and presence of surrounding halo.
RESULTS
Large size, high SI on T2WI, heterogeneous enhancement, and internal fat component were commonly observed in myxoid tumors, while homogenous enhancement, fat split sign, target sign were common in BPNSTs. The differences were statistically significant (P < 0.05). Other findings, such as margin, homogeneity of SI on T2WI, enhancement pattern (peripheral or solid), internal cystic portion, continuation with neurovascular bundle, and surrounding halo, did not show significant difference between myxoid tumors and BPNSTs (P > 0.05).
CONCLUSION
In the differential diagnosis of myxoid tumors and BPNSTs involving the musculoskeletal system, several MRI findings such as degree of SI on T2WI, enhancement homogeneity, internal fat component, fat split sign, and target sign, may be helpful in establishing the diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999; 19:1253–1280.2. Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995; 164:395–402.3. Kransdorf MJ. Malignant soft-tissue tumors in a large referral population: distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995; 164:129–134.4. Muler JH, Paulino AF, Roulston D, Baker LH. Myxoid malignant fibrous histiocytoma with multiple primary sites. Sarcoma. 2002; 6:51–55.5. Gustafson P. Soft tissue sarcoma. Epidemiology and prognosis in 508 patients. Acta Orthop Scand Suppl. 1994; 259:1–31.6. Willems SM, Wiweger M, van Roggen JF, Hogendoorn PC. Running GAGs: myxoid matrix in tumor pathology revisited: what's in it for the pathologist? Virchows Arch. 2010; 456:181–192.7. Graadt van Roggen JF, Hogendoorn PC, Fletcher CD. Myxoid tumours of soft tissue. Histopathology. 1999; 35:291–312.8. Bermejo A, De Bustamante TD, Martinez A, Carrera R, Zabia E, Manjon P. MR imaging in the evaluation of cystic-appearing soft-tissue masses of the extremities. Radiographics. 2013; 33:833–855.9. Sung MS, Kang HS, Suh JS, et al. Myxoid liposarcoma: appearance at MR imaging with histologic correlation. Radiographics. 2000; 20:1007–1019.10. Waters B, Panicek DM, Lefkowitz RA, et al. Low-grade myxofibrosarcoma: CT and MRI patterns in recurrent disease. AJR Am J Roentgenol. 2007; 188:W193–W198.11. Banks KP. The target sign: extremity. Radiology. 2005; 234:899–900.12. Kaya M, Wada T, Nagoya S, et al. MRI and histological evaluation of the infiltrative growth pattern of myxofibrosarcoma. Skeletal Radiol. 2008; 37:1085–1090.13. Laffan EE, Ngan BY, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: part 2. Tumors of fibroblastic/myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin. Radiographics. 2009; 29:e36.14. Lowenthal D, Zeile M, Niederhagen M, et al. Differentiation of myxoid liposarcoma by magnetic resonance imaging: a histopathologic correlation. Acta Radiol. 2014; 55:952–960.15. Suh JS, Abenoza P, Galloway HR, Everson LI, Griffiths HJ. Peripheral (extracranial) nerve tumors: correlation of MR imaging and histologic findings. Radiology. 1992; 183:341–346.16. Tateishi U, Hasegawa T, Beppu Y, Kawai A, Satake M, Moriyama N. Prognostic significance of MRI findings in patients with myxoid-round cell liposarcoma. AJR Am J Roentgenol. 2004; 182:725–731.17. van Vliet M, Kliffen M, Krestin GP, van Dijke CF. Soft tissue sarcomas at a glance: clinical, histological, and MR imaging features of malignant extremity soft tissue tumors. Eur Radiol. 2009; 19:1499–1511.18. Varma DG, Moulopoulos A, Sara AS, et al. MR imaging of extracranial nerve sheath tumors. J Comput Assist Tomogr. 1992; 16:448–453.19. Koga H, Matsumoto S, Manabe J, Tanizawa T, Kawaguchi N. Definition of the target sign and its use for the diagnosis of schwannomas. Clin Orthop Relat Res. 2007; 464:224–229.20. Chee DW, Peh WC, Shek TW. Pictorial essay: imaging of peripheral nerve sheath tumours. Can Assoc Radiol J. 2011; 62:176–182.21. Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM. Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics. 2003; 23:29–43.22. Zulfiqar MI, Sheikh UN, Montgomery EA. Myxoid neoplasms. Surg Pathol Clin. 2011; 4:843–864.23. Murphey MD, McRae GA, Fanburg-Smith JC, Temple HT, Levine AM, Aboulafia AJ. Imaging of soft-tissue myxoma with emphasis on CT and MR and comparison of radiologic and pathologic findings. Radiology. 2002; 225:215–224.24. Lal H, Neyaz Z, Kapoor VK, Pottakkat B, Gupta P. Local recurrence and multi-organ metastasis of primary retroperitoneal leiomyosarcoma in unusual locations after surgical resection. J Radiol Case Rep. 2011; 5:1–8.25. Levy AD, Remotti HE, Thompson WM, Sobin LH, Miettinen M. Gastrointestinal stromal tumors: radiologic features with pathologic correlation. Radiographics. 2003; 23:283–304. 456quiz 532
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Peripheral Nerve Sheath Tumor of the Larynx
- Sequestered Disc Mimicking Benign Neurogenic Tumor: Report of 2 Cases
- Multiple Primary Cardiac Malignant Peripheral Nerve Sheath Tumors in the Left Atrium: Case Report
- Malignant Peripheral Nerve Sheath Tumor of the Breast in a Patient without Neurofibromatosis: A Case Report
- Two Cases of Retroperitioneal Schwannoma