Ann Dermatol.
2009 Feb;21(1):75-77. 10.5021/ad.2009.21.1.75.
A Case of Vitiligo after Kawasaki's Disease
- Affiliations
-
- 1Department of Dermatology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea. dermy@kd.ac.kr
- 2Department of Pediatric Cardiology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- 3Department of Pathology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- KMID: 2172073
- DOI: http://doi.org/10.5021/ad.2009.21.1.75
Abstract
- Vitiligo is a common skin disease, but its pathogenesis has not been fully determined, though an autoimmune etiology is considered likely. Kawasaki disease (KD) is an acute multisystem vasculitis of childhood associated with coronary arteriopathy, and is diagnosed based on clinical criteria. Furthermore, vitiligo has been associated with several other diseases, but no report has been issued about the relationship between vitiligo and Kawasaki's disease. The author's report the case of an 8-year-old male child that presented with depigmented lesions, which developed from the desquamative skin lesions of Kawasaki's disease.
Keyword
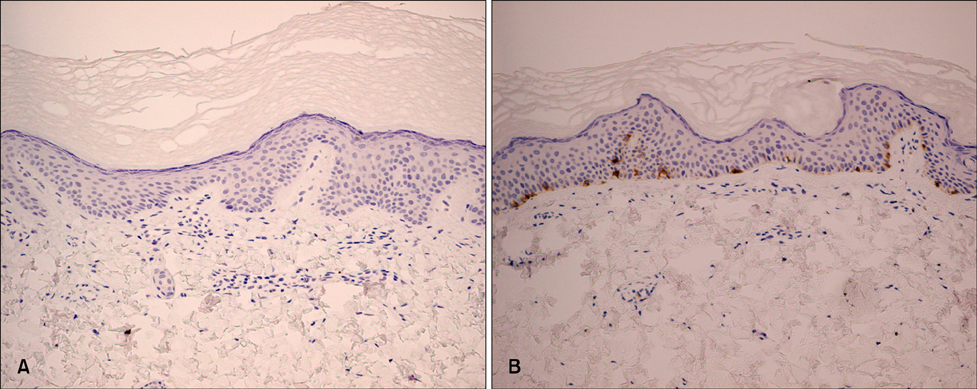
Figure
Reference
-
1. Kovacs SO. Vitiligo. J Am Acad Dermatol. 1998. 38:647–666.
Article2. Kemp EH, Gavalas NG, Gawkrodger DJ, Weetman AP. Autoantibody responses to melanocytes in the depigmenting skin disease vitiligo. Autoimmun Rev. 2007. 6:138–142.
Article3. Passeron T, Ortonne JP. Physiopathology and genetics of vitiligo. J Autoimmun. 2005. 25:Suppl. 63–68.
Article4. Ongenae K, Van Geel N, Naeyaert JM. Evidence for an autoimmune pathogenesis of vitiligo. Pigment Cell Res. 2003. 16:90–100.
Article5. Harning R, Cui J, Bystryn JC. Relation between the incidence and level of pigment cell antibodies and disease activity in vitiligo. J Invest Dermatol. 1991. 97:1078–1080.
Article6. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004. 114:1708–1733.
Article7. Zvulunov A, Greenberg D, Cagnano E, Einhorn M. Development of psoriatic lesions during acute and convalescent phases of Kawasaki disease. J Paediatr Child Health. 2003. 39:229–231.
Article8. Schwartz RA, Janniger CK. Vitiligo. Cutis. 1997. 60:239–244.9. Kemp EH, Waterman EA, Weetman AP. Autoimmune aspects of vitiligo. Autoimmunity. 2001. 34:65–77.
Article10. Kim DS. Kawasaki disease. Yonsei Med J. 2006. 47:759–772.
Article11. Frieden IJ, Resnick SD. Kawasaki disease. Pediatr Clin North Am. 1991. 38:881–882.12. Mizuno Y, Suga Y, Muramatsu S, Hasegawa T, Ogawa H. Psoriasiform and palmoplanter pustular lesions induced after Kawasaki disease. Int J Dermatol. 2006. 45:1080–1082.
Article