Ann Dermatol.
2013 May;25(2):208-212. 10.5021/ad.2013.25.2.208.
Eccrine Angiomatous Hamartoma: A Review of Ten Cases
- Affiliations
-
- 1Department of Dermatology, Ajou University School of Medicine, Suwon, Korea. maychan@ajou.ac.kr
- 2Department of Dermatology, Kyungpook National University School of Medicine, Daegu, Korea.
- 3Department of Dermatology, Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2171790
- DOI: http://doi.org/10.5021/ad.2013.25.2.208
Abstract
- BACKGROUND
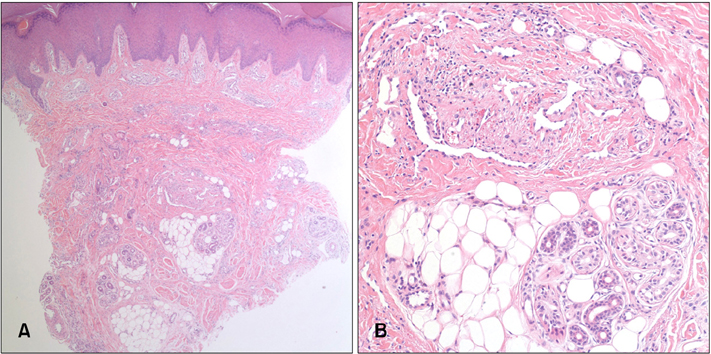
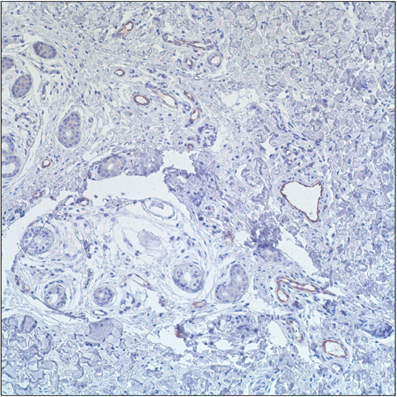
Eccrine angiomatous hamartoma (EAH) is a rare benign nodular lesion characterized by the proliferation of eccrine and vascular structures, generally capillaries, in the middle and deep dermis. It may be congenital or appear later in childhood, but rarely arises in adulthood.
OBJECTIVE
To investigate the clinicopathologic features of EAH in Korean patients.
METHODS
Ten cases of EAH diagnosed at Ajou University Hospital and Gangnam Severance Hospital in Korea from 2007 to 2010 were retrospectively reviewed.
RESULTS
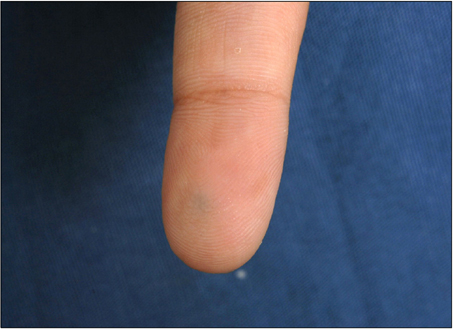
The age range of patients was between 5 and 66 years with an equal number of male and female patients. Apart from two congenital cases, the onset was late, ranging from 6 months to 65 years of age. All lesions were solitary and located on the distal extremities. Nine cases appeared as a yellow-brown nodule or plaque resembling a callus. Neither hyperhidrosis nor hypertrichosis was documented. Apart from the typical histological findings of EAH, prominent mucin deposition, fat component and nerve infiltration were observed.
CONCLUSION
This is one of the largest single case series of EAH in the literature. Clinically, resemblance to callosities and the frequent occurrence in the adulthood were the unique features in our series.
Keyword
MeSH Terms
Figure
Reference
-
1. Lotzbeck C. Ein Fall von Schweissdrusengeschwulst an der Wange. Virchows Arch Pathol Anat. 1859. 16:160.2. Challa VR, Jona J. Eccrine angiomatous hamartoma: a rare skin lesion with diverse histological features. Dermatologica. 1977. 155:206–209.
Article3. Yun JH, Kang HK, Na SY, Roh JY, Lee JR. Eccrine angiomatous hamartoma mimicking a traumatic hemorrhage. Ann Dermatol. 2011. 23:Suppl 1. S84–S87.
Article4. Pelle MT, Pride HB, Tyler WB. Eccrine angiomatous hamartoma. J Am Acad Dermatol. 2002. 47:429–435.
Article5. Nakatsui TC, Schloss E, Krol A, Lin AN. Eccrine angiomatous hamartoma: report of a case and literature review. J Am Acad Dermatol. 1999. 41:109–111.
Article6. Lever WF, Elder DE. Lever's histopathology of the skin. 2009. 10th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.7. Galan A, McNiff JM. Eccrine angiomatous hamartoma with features resembling verrucous hemangioma. J Cutan Pathol. 2007. 34:Suppl 1. 68–70.
Article8. Smith C, Montesinos E, Revert A, Ramon D, Molina I, Jorda E. Eccrine angiomatous hamartoma: report of three patients. Pediatr Dermatol. 1996. 13:139–142.
Article9. Torres JE, Martín RF, Sánchez JL. Eccrine angiomatous hamartoma. P R Health Sci J. 1994. 13:159–160.10. Sulica RL, Kao GF, Sulica VI, Penneys NS. Eccrine angiomatous hamartoma (nevus): immunohistochemical findings and review of the literature. J Cutan Pathol. 1994. 21:71–75.
Article11. Aloi F, Tomasini C, Pippione M. Eccrine angiomatous hamartoma: a multiple variant. Dermatology. 1992. 184:219–222.
Article12. Diaz-Landaeta L, Kerdel FA. Hyperhidrotic, painful lesion. Eccrine angiomatous hamartoma. Arch Dermatol. 1993. 129:107. 110.
Article13. Kikuchi I, Kuroki Y, Inoue S. Painful eccrine angiomatous nevus on the sole. J Dermatol. 1982. 9:329–332.
Article14. Srinivas CR, Rao PL. Sudoriparous angioma--regression following intravascular aethoxysclerol, a sclerosing agent. Br J Dermatol. 1988. 119:111–113.
Article15. Tharakaram S, Kumar TV, Yesudian P. Sudoriparous angioma. Int J Dermatol. 1983. 22:432–433.
Article16. Wolf R, Krakowski A, Dorfman B, Baratz M. Eccrine angiomatous hamartoma. A painful step. Arch Dermatol. 1989. 125:1489–1490.
Article17. Donati P, Amantea A, Balus L. Eccrine angiomatous hamartoma: a lipomatous variant. J Cutan Pathol. 1989. 16:227–229.
Article18. Gabrielsen TO, Elgjo K, Sommerschild H. Eccrine angiomatous hamartoma of the finger leading to amputation. Clin Exp Dermatol. 1991. 16:44–45.
Article19. Seraly MP, Magee K, Abell E, Bridenstine J, Jegasothy BV. Eccrine-angiomatous nevus, a new variant. J Am Acad Dermatol. 1993. 29:274–275.
Article20. Nakayama H, Mihara M, Hattori K, Mishima E, Shimao S. Eccrine angiomatous hamartoma of the sacral region. Acta Derm Venereol. 1994. 74:477.21. Cebreiro C, Sánchez-Aguilar D, Gómez Centeno P, Fernández-Redondo V, Toribio J. Eccrine angiomatous hamartoma: report of seven cases. Clin Exp Dermatol. 1998. 23:267–270.
Article22. Tsuji T, Sawada H. Eccrine angiomatous hamartoma with verrucous features. Br J Dermatol. 1999. 141:167–169.
Article23. Laeng RH, Heilbrunner J, Itin PH. Late-onset eccrine angiomatous hamartoma: clinical, histological and imaging findings. Dermatology. 2001. 203:70–74.
Article24. Jeong E, Park HJ, Oh ST, Lee JY, Cho BK. Late-onset eccrine angiomatous hamartoma on the forehead. Int J Dermatol. 2006. 45:598–599.
Article25. Lee Y, Jung YJ, Lee WS. Late-onset eccrine angiomatous hamartoma associated with a ganglion cyst on the sole of the foot. Ann Dermatol. 2011. 23:S218–S221.
Article