Ewha Med J.
2014 Dec;37(Suppl):S37-S40. 10.12771/emj.2014.37.S.S37.
Amphetamine-Like Weight Reduction Drug Induced Acute Cardiomyopathy with Left Ventricular Thrombosis
- Affiliations
-
- 1Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea. ysk1140@eulji.ac.kr
- 2Yonsei Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2171310
- DOI: http://doi.org/10.12771/emj.2014.37.S.S37
Abstract
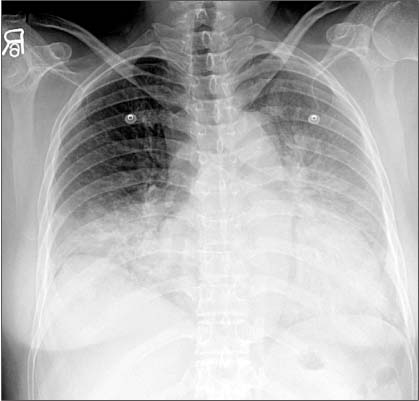
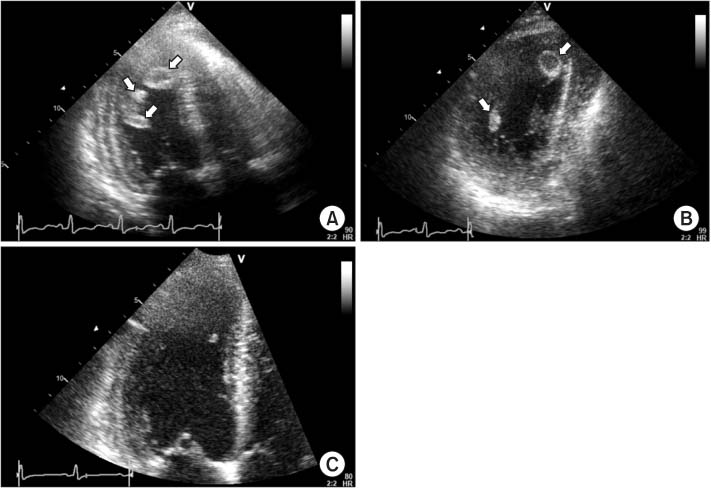
- A 37-year-old female patient admitted due to dyspnea on exertion and peripheral edema. For one and a half years, the patient had been taking various drugs and supplements to reduce weight, including amphetamine-like drugs. The patient had no major cardiovascular risk factors except three pack-years of smoking. A chest computed tomography showed a 1.7 cm diameter, capsulated space-occupying lesion in the left ventricle (LV) and 2-dimensional echocardiography showed LV systolic dysfunction (Left ventricular ejection fraction [LVEF], 30%) with a mobile cystic mass (1.1x1.8 cm) that was attached to the LV apex, which was increased in size and number the next day, even with low dose low-molecular-weight heparin. With an increased dose of anticoagulation medication and heart failure management with diuretics and angiotensin receptor II blocker, LV dysfunction was recovered and the LV thrombus disappeared.
Keyword
MeSH Terms
Figure
Reference
-
1. Mariotti KC, Rossato LG, Froehlich PE, Limberger RP. Amphetamine-type medicines: a review of pharmacokinetics, pharmacodynamics, and toxicological aspects. Curr Clin Pharmacol. 2013; 8:350–357.2. Bashour TT. Acute myocardial infarction resulting from amphetamine abuse: a spasm-thrombus interplay? Am Heart J. 1994; 128:1237–1239.3. Carson P, Oldroyd K, Phadke K. Myocardial infarction due to amphetamine. Br Med J. 1987; 294:1525–1526.4. De Silva DA, Wong MC, Lee MP, Chen CL, Chang HM. Amphetamine-associated ischemic stroke: clinical presentation and proposed pathogenesis. J Stroke Cerebrovasc Dis. 2007; 16:185–186.5. Huang CN, Wu DJ, Chen KS. Acute myocardial infarction caused by transnasal inhalation of amphetamine. Jpn Heart J. 1993; 34:815–818.6. Hung MJ, Kuo LT, Cherng WJ. Amphetamine-related acute myocardial infarction due to coronary artery spasm. Int J Clin Pract. 2003; 57:62–64.7. Orzel JA. Acute myocardial infarction complicated by chronic amphetamine use. Arch Intern Med. 1982; 142:644.8. Packe GE, Garton MJ, Jennings K. Acute myocardial infarction caused by intravenous amphetamine abuse. Br Heart J. 1990; 64:23–24.9. Ragland AS, Ismail Y, Arsura EL. Myocardial infarction after amphetamine use. Am Heart J. 1993; 125:247–249.10. Waksman J, Taylor RN Jr, Bodor GS, Daly FF, Jolliff HA, Dart RC. Acute myocardial infarction associated with amphetamine use. Mayo Clin Proc. 2001; 76:323–326.11. Call TD, Hartneck J, Dickinson WA, Hartman CW, Bartel AG. Acute cardiomyopathy secondary to intravenous amphetamine abuse. Ann Intern Med. 1982; 97:559–560.12. Croft CH, Firth BG, Hillis LD. Propylhexedrine-induced left ventricular dysfunction. Ann Intern Med. 1982; 97:560–561.13. Waller BF, Rohr TM, McLaughlin T, Grider L, Taliercio CP, Fetters J. Intracardiac thrombi: frequency, location, etiology, and complications: a morphologic review: part II. Clin Cardiol. 1995; 18:530–534.14. Haft JI, Kranz PD, Albert FJ, Fani K. Intravascular platelet aggregation in the heart induced by norepinephrine. Microscopic studies. Circulation. 1972; 46:698–708.15. Pepi M, Evangelista A, Nihoyannopoulos P, Flachskampf FA, Athanassopoulos G, Colonna P, et al. Recommendations for echocardiography use in the diagnosis and management of cardiac sources of embolism: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr. 2010; 11:461–476.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Ventricular Thrombus Associated with Takotsubo Cardiomyopathy: A Cardioembolic Cause of Cerebral Infarction
- A Case of Pheochromocytoma Presenting as Stress-Induced Cardiomyopathy with Large Left Ventricular Thrombus
- Stress-induced cardiomyopathy during ophthalmologic surgery: A case report
- A Case of Apical Hypertrophic Cardiomyopathy Combined Acute Myocardial Infarction with Multiple Coronary Thrombosis
- A Case of Anorexia Nervosa Complicated With Strongly Suspected Stress-Induced Cardiomyopathy and Mural Thrombus