Ewha Med J.
2014 Mar;37(1):36-40. 10.12771/emj.2014.37.1.36.
Retrospective Analysis of Anesthesia for Cesarean Section of the Patients with Hypertensive Disorders in Pregnancy for 15 Years
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Gangnam CHA Hospital, CHA University, Seoul, Korea. ecbang63@hanmail.net
- KMID: 2171272
- DOI: http://doi.org/10.12771/emj.2014.37.1.36
Abstract
OBJECTIVES
To compare the clnical data of general and regional anesthesia for cesarean section in patients with systemic hypertension.
METHODS
We conducted a retrospective survey with the medical records of the patients with hypertensive disorders in pregnancy, who under went cesarean section from January 1998 to December 2012. We collected data including patients' demographics, anesthesia and maternal and neonatal outcome. According to anesthetic method, the subjects were divided into general anesthesia and regional anesthesia group and the clinical outcome were compared. We reclassified the patients according to the use of magnesium sul fate (MgSO4) and compared the clinical outcomes.
RESULTS
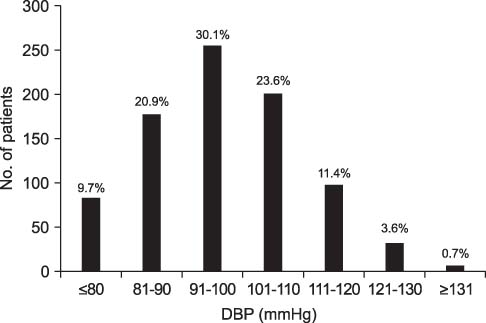
Of the 1,050 hypertensive parturients, 848 (80.8%) patients went through cesarean section. Three hundred and sixty three patients (42.8%) underwent epidural anesthesia, general and spinal anesthesia were used in 268 (31.6%), and 217 (25.6%) patients, respectively. There was no significant difference in maternal and neonatal outcome according to anesthetic method. In the patients administered MgSO4, 1 minute Apgar score was lower and maternal gestational age and birth weight were less than the patients not receiving MgSO4.
CONCLUSION
Anesthetic methods did not have effect on outcome of cesarean section of the patients with hypertensive disorder of pregnancy.
Keyword
MeSH Terms
Figure
Reference
-
1. Sibai BM. Hypertension. In : Gabbe SG, editor. Obstetrics: normal and problem pregnancies. 6th ed. Philadelphia, PA: Elsevier Mosby;2012. p. 779–820.2. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000; 183:S1–S22.3. Wali A, Suresh MS. Maternal morbidity, mortality, and risk assessment. Anesthesiol Clin. 2008; 26:197–230.4. Savaj S, Vaziri N. An overview of recent advances in pathogenesis and diagnosis of preeclampsia. Iran J Kidney Dis. 2012; 6:334–338.5. Gofton EN, Capewell V, Natale R, Gratton RJ. Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension. Am J Obstet Gynecol. 2001; 185:798–803.6. Zuspan FP. New concepts in the understanding of hypertensive diseases during pregnancy: an overview. Clin Perinatol. 1991; 18:653–659.7. Lo JO, Mission JF, Caughey AB. Hypertensive disease of pregnancy and maternal mortality. Curr Opin Obstet Gynecol. 2013; 25:124–132.8. Byun JS, Jung J, Kim SM, Kim YH, Song TB. A clinical study of pregnancy-induced hypertensionPIH in Korea in the last 7 years (1992-1998). Korean J Obstet Gynecol. 2000; 43:2283–2292.9. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap L III, Wenstrom KD. Hypertensive disorder in pregnancy. In : Cunningham FG, Leveno KJ, Gilstrap LC, editors. Williams obstetrics. 22th ed. New York: McGraw-Hill Co.;2005. p. 737–754.10. Terrone DA, Isler CM, May WL, Magann EF, Norman PF, Martin JN Jr. Cardiopulmonary morbidity as a complication of severe preeclampsia HELLP syndrome. J Perinatol. 2000; 20:78–81.11. Dyer RA, Piercy JL, Reed AR. The role of the anaesthetist in the management of the pre-eclamptic patient. Curr Opin Anaesthesiol. 2007; 20:168–174.12. Dennis AT. Management of pre-eclampsia: issues for anaesthetists. Anaesthesia. 2012; 67:1009–1020.13. Wallace DH, Giesecke AH. Spinal anesthesia in severe preeclampsia: a historical analysis of reappraisal. Int Cong Ser. 2002; 1242:177–183.14. Huang CJ, Fan YC, Tsai PS. Differential impacts of modes of anaesthesia on the risk of stroke among preeclamptic women who undergo Caesarean delivery: a population-based study. Br J Anaesth. 2010; 105:818–826.15. Chaudhary S, Salhotra R. Subarachnoid block for caesarean section in severe preeclampsia. J Anaesthesiol Clin Pharmacol. 2011; 27:169–173.16. Ajuzieogu OV, Ezike HA, Amucheazi AO, Enwereji J. A retrospective study of the outcome of cesarean section for women with severe pre-eclampsia in a third world setting. Saudi J Anaesth. 2011; 5:15–18.17. Aya AG, Mangin R, Vialles N, Ferrer JM, Robert C, Ripart J, et al. Patients with severe preeclampsia experience less hypotension during spinal anesthesia for elective cesarean delivery than healthy parturients: a prospective cohort comparison. Anesth Analg. 2003; 97:867–872.18. Clark VA, Sharwood-Smith GH, Stewart AV. Ephedrine requirements are reduced during spinal anaesthesia for caesarean section in preeclampsia. Int J Obstet Anesth. 2005; 14:9–13.19. Sharwood-Smith G, Clark V, Watson E. Regional anaesthesia for caesarean section in severe preeclampsia: spinal anaesthesia is the preferred choice. Int J Obstet Anesth. 1999; 8:85–89.20. Alexander JM, McIntire DD, Leveno KJ, Cunningham FG. Selective magnesium sulfate prophylaxis for the prevention of eclampsia in women with gestational hypertension. Obstet Gynecol. 2006; 108:826–832.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical evaluation of anesthesia for cesarean section of the patients with hypertensive disorders in pregnancy: retrospective study for 10 years
- Clinical evaluation of anesthesia for cesarean section of the patients with hypertensive disorders in pregnancy
- Anesthetic Management of a Patient with Pheochromocytoma in Pregnancy: A case report
- Clinical Evaluation of Anesthesia for Cesarean Section of Toxemia
- A Case of an Anesthesia for an Emergency Cesarean Section in a Patient with an Aortic Dissection