Infect Chemother.
2015 Dec;47(4):261-267. 10.3947/ic.2015.47.4.261.
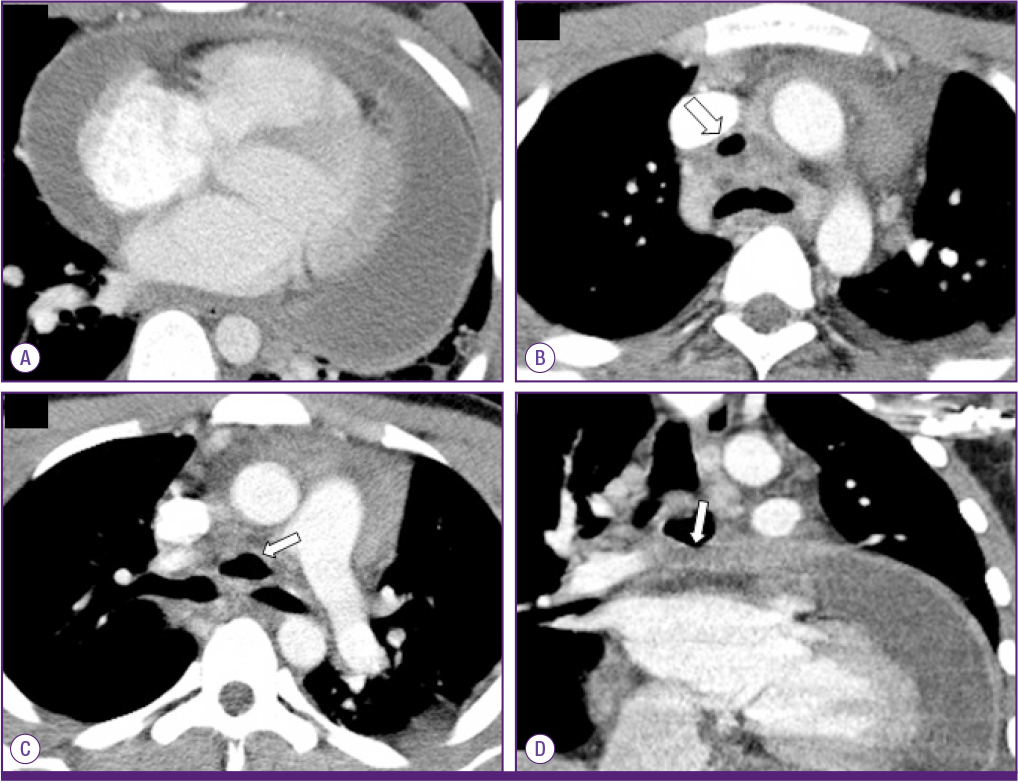
Polymicrobial Purulent Pericarditis Probably caused by a Broncho-Lymph Node-Pericardial Fistula in a Patient with Tuberculous Lymphadenitis
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. paihj@hanyang.ac.kr
- 2Department of Thoracic and Cardiovascular Surgery, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 2170505
- DOI: http://doi.org/10.3947/ic.2015.47.4.261
Abstract
- Purulent pericarditis is a rare condition with a high mortality rate. We report a case of purulent pericarditis subsequently caused by Candida parapsilosis, Peptostreptococcus asaccharolyticus, Streptococcus anginosus, Staphylococcus aureus, Prevotella oralis, and Mycobacterium tuberculosis in a previously healthy 17-year-old boy with mediastinal tuberculous lymphadenitis. The probable route of infection was a bronchomediastinal lymph node-pericardial fistula. The patient improved with antibiotic, antifungal, and antituberculous medication in addition to pericardiectomy.
Keyword
MeSH Terms
Figure
Reference
-
1. Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH. Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004; 25:587–610.2. Shiber JR. Purulent pericarditis: Acute infections and chronic complications. Hosp Physician. 2008; 44:9–18.3. Ferreira dos Santos L, Moreira D, Ribeiro P, Rodrigues B, Correia E, Nunes L, Sequeira M, Albuquerque A, Barros I, Saraiva JP, Santos O. Purulent pericarditis: a rare diagnosis. Rev Port Cardiol. 2013; 32:721–727.
Article4. Rubin RH, Moellering RC Jr. Clinical, microbiologic and therapeutic aspects of purulent pericarditis. Am J Med. 1975; 59:68–78.
Article5. Parsons R, Argoud G, Palmer DL. Mixed bacterial infection of the pericardium. South Med J. 1983; 76:1046–1048.
Article6. Epstein SK, Winslow CJ, Brecher SM, Faling LJ. Polymicrobial bacterial pericarditis after transbronchial needle aspiration. Case report with an investigation on the risk of bacterial contamination during fiberoptic bronchoscopy. Am Rev Respir Dis. 1992; 146:523–525.
Article7. Lu DC, Chang SC, Chen HC. Polymicrobial bacterial pericarditis with mediastinitis after endotracheal intubation. Diagn Microbiol Infect Dis. 1995; 23:115–118.
Article8. Sawaya FJ, Sawaya JI, Gharzuddine W, Eid EV, Kanj SS. Cardiac tamponade caused by polymicrobial gram-negative organisms. Int J Infect Dis. 2009; 13:e483–e484.
Article9. Louw A, Tikly M. Purulent pericarditis due to co-infection with Streptococcus pneumoniae and Mycobacterium tuberculosis in a patient with features of advanced HIV infection. BMC Infect Dis. 2007; 7:12.10. World Health Organization (WHO). Global tuberculosis report 2013. Accessed 17 May 2014. Available at: http://reliefweb.int/sites/reliefweb.int/files/resources/9789241564656_eng.pdf.11. Trauter BW, Darouiche RO. Tuberculous pericarditis: optimal diagnosis and management. Clin Infect Dis. 2001; 33:954–961.
Article12. Stirling P, Faroug R, Amanat S, Ahmed A, Armstrong M, Sharma P, Qamruddin A. False-negative rate of Gram-stain microscopy for diagnosis of septic arthritis: suggestions for improvement. Int J Microbiol. 2014; 2014:830857.
Article13. Marchiori E, Francisco FA, Zanetti G, Hochhegger B. Lymphobronchial fistula: another complication associated with lymphobronchial tuberculosis in children. Pediatr Radiol. 2013; 43:252–253.
Article14. Yoon JH, Jung JY, Min JW, Park SY, Jeon YD, Hong HC, Bang JH, Joh JS. Lymphobronchial fistula of tuberculous lymphadenitis in acquired immunodeficiency syndrome. Infect Chemother. 2012; 44:35–39.
Article15. Bennett JA, Haramati LB. CT of bronchopericardial fistula: an unusual complication of multi drug-resistant tuberculosis in HIV infection. AJR Am J Roentgenol. 2000; 175:819–820.16. Owens CM, Hamon MD, Graham TR, Wood AJ, Newland AC. Bronchopericardial fistula and pneumopericardium complicating invasive pulmonary aspergillosis. Clin Lab Haematol. 1990; 12:351–354.
Article17. Dabar G, Daher M, Harmouche C. Bronchopericardial fistula treatment by a metallic stent. Rev Mal Respir. 2013; 30:429–432.18. Wattez H, Bellier J, Akkad R, Porte H. Bronchopericardial fistula after a pulmonary resection. Ann Thorac Surg. 2013; 95:1099.
Article19. Ali I, Beg MH. Traumatic bronchopericardial fistula presenting as cardiac tamponade. J Thorac Cardiovasc Surg. 1988; 95:740.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Purulent pericarditis: subdiaphragmatic suppurative focus
- Esophago-Mediastinal Fistula Due to Tuberculous Mediastinal Lymphadenitis
- Primary Purulent Pericarditis with Cardiac Tamponade due to Oropharyngeal Polymicrobial Infection: A Case Report and Literature Review
- Nodo-Colonic Fistula Caused by Intra-Abdominal Tuberculous Lymphadenitis during Treatment with Anti-Tuberculous Medication: A Case Report
- The role of CT in the diagnosis of constrictive pericarditis