Cancer Res Treat.
2014 Jan;46(1):74-80.
High-Dose-Rate Brachytherapy for the Treatment of Vaginal Intraepithelial Neoplasia
- Affiliations
-
- 1Department of Radiation Oncology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- 3Department of Obstetrics and Gynecology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 4Department of Medical Oncology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 5Department of Radiation Oncology, Bucheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Bucheon, Korea. scyoon@catholic.ac.kr
Abstract
- PURPOSE
Vaginal intraepithelial neoplasia (VAIN), a rare premalignant condition, is difficult to eradicate. We assess the effectiveness of high-dose rate intracavitary brachytherapy (HDR-ICR) in patients with VAIN or carcinoma in situ (CIS) of the vagina after hysterectomy.
MATERIALS AND METHODS
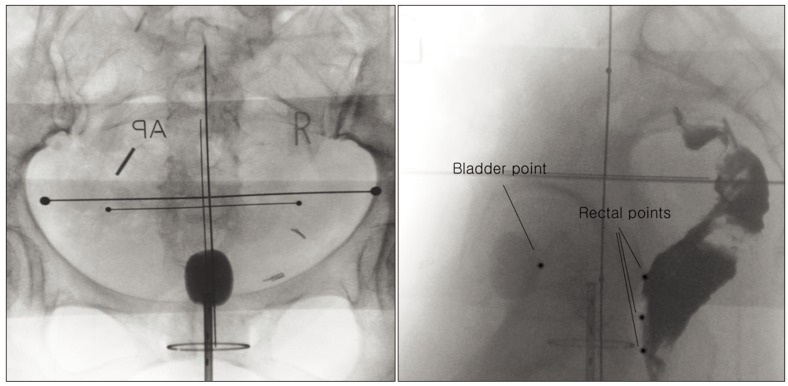
We reviewed 34 patients treated for posthysterectomy VAIN or CIS of the vagina by brachytherapy as the sole treatment. All patients underwent a coloposcopic-directed punch biopsy or had abnormal cytology, at least 3 consecutive times. All patients were treated with a vaginal cylinder applicator. The total radiation dose was mainly 40 Gy in 8 fractions during the periods of 4 weeks at a prescription point of the median 0.2 cm (range, 0 to 0.5 cm) depth from the surface of the vaginal mucosa.
RESULTS
Acute toxicity was minimal. Seven patients had grade 1/2 acute urinary and rectal complications. There were 15 cases of late toxicity, predominantly vaginal mucosal reaction in 12 patients. Of these patients, two patients suffered from grade 3 vaginal stricture and dyspareunia continuously. After a median follow-up time of 48 months (range, 4 to 122 months), there were 2 recurrences and 2 persistent diseases, in which a second-line therapy was needed. The success rate was 88.2%. The average prescription point in failure patients was 1.1 mm from the surface of the vagina compared to an average of 2.6 mm in non-recurrent patients (p=0.097).
CONCLUSION
HDR-ICR is an effective treatment method in VAIN patients. In spite of high cure rates, we should consider issues regarding vaginal toxicity and radiation techniques to reduce the occurrence of failure and toxicity.
MeSH Terms
Figure
Reference
-
1. Dodge JA, Eltabbakh GH, Mount SL, Walker RP, Morgan A. Clinical features and risk of recurrence among patients with vaginal intraepithelial neoplasia. Gynecol Oncol. 2001; 83:363–369. PMID: 11606098.
Article2. Audet-Lapointe P, Body G, Vauclair R, Drouin P, Ayoub J. Vaginal intraepithelial neoplasia. Gynecol Oncol. 1990; 36:232–239. PMID: 2404839.
Article3. Gurumurthy M, Cruickshank ME. Management of vaginal intraepithelial neoplasia. J Low Genit Tract Dis. 2012; 16:306–312. PMID: 22460272.
Article4. Wee WW, Chia YN, Yam PK. Diagnosis and treatment of vaginal intraepithelial neoplasia. Int J Gynaecol Obstet. 2012; 117:15–17. PMID: 22239755.
Article5. Gemmell J, Holmes DM, Duncan ID. How frequently need vaginal smears be taken after hysterectomy for cervical intraepithelial neoplasia? Br J Obstet Gynaecol. 1990; 97:58–61. PMID: 2306428.
Article6. Woodman CB, Mould JJ, Jordan JA. Radiotherapy in the management of vaginal intraepithelial neoplasia after hysterectomy. Br J Obstet Gynaecol. 1988; 95:976–979. PMID: 3191051.
Article7. Teruya Y, Sakumoto K, Moromizato H, Toita T, Ogawa K, Murayama S, et al. High dose-rate intracavitary brachytherapy for carcinoma in situ of the vagina occurring after hysterectomy: a rational prescription of radiation dose. Am J Obstet Gynecol. 2002; 187:360–364. PMID: 12193925.
Article8. Ogino I, Kitamura T, Okajima H, Matsubara S. High-dose-rate intracavitary brachytherapy in the management of cervical and vaginal intraepithelial neoplasia. Int J Radiat Oncol Biol Phys. 1998; 40:881–887. PMID: 9531374.9. MacLeod C, Fowler A, Dalrymple C, Atkinson K, Elliott P, Carter J. High-dose-rate brachytherapy in the management of high-grade intraepithelial neoplasia of the vagina. Gynecol Oncol. 1997; 65:74–77. PMID: 9103394.
Article10. Graham K, Wright K, Cadwallader B, Reed NS, Symonds RP. 20-year retrospective review of medium dose rate intracavitary brachytherapy in VAIN3. Gynecol Oncol. 2007; 106:105–111. PMID: 17481703.
Article11. Blanchard P, Monnier L, Dumas I, Morice P, Pautier P, Duvillard P, et al. Low-dose-rate definitive brachytherapy for high-grade vaginal intraepithelial neoplasia. Oncologist. 2011; 16:182–188. PMID: 21262875.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Design of a New Applicator for High-Dose Rate Vaginal Brachytherapy
- Total vaginectomy for refractory vaginal intraepithelial neoplasia III of the vaginal vault
- Effectiveness of 5-FU Cream in the Management of Vaginal Intraepithelial Neoplasia
- Dosimetric analysis of intracavitary brachytherapy applicators: a practical study
- Role of CO2 laser Vaporization in the Management of Vaginal Intraepithelial Neoplasia