Ann Surg Treat Res.
2014 Jun;86(6):331-333. 10.4174/astr.2014.86.6.331.
Use of right lobe graft with type IV portal vein accompanied by type IV biliary tree in living donor liver transplantation: report of a case
- Affiliations
-
- 1Department of General Surgery, Assiut University Hospital, Assiut, Egypt.
- 2Department of HBP Surgery and Liver Transplantation, Korea University College of Medicine, Seoul, Korea. kimds1@korea.ac.kr
- KMID: 2167112
- DOI: http://doi.org/10.4174/astr.2014.86.6.331
Abstract
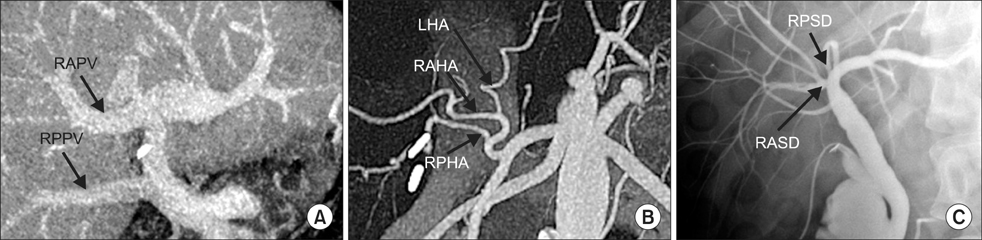
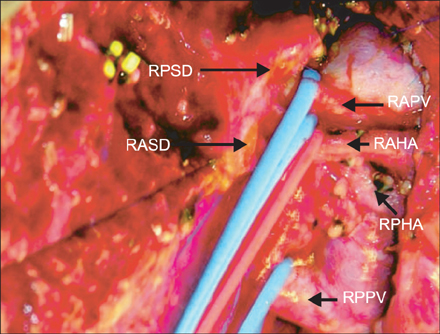
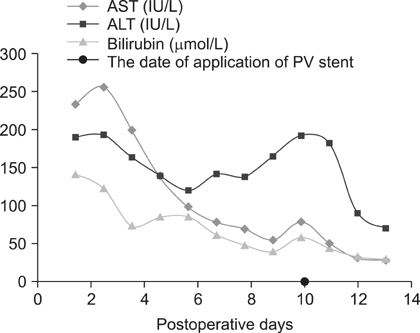
- Anatomic variations of the portal vein (PV) and bile duct (BD) are more common on the right lobe as compared with left lobe grafts in living donor liver transplantation (LDLT). We recently experienced a case of LDLT for hepatocellular carcinoma combined with liver cirrhosis secondary to hepatitis B virus and hepatitis C virus infection. The only available donor had right lobe graft with type IV PV associated with type IV BD. The patient underwent relaparotomy for PV stenting due to PV stenosis. Percutaneous transhepatic biliary drainage was done for a stricture at the site of biliary reconstruction. Thereafter, the patient was discharged in good health. Our experience suggests that, the use of right lobe graft with type IV PV accompanied by type IV BD should be the last choice for LDLT, because of its technical difficulty and risks of associated complications.
MeSH Terms
Figure
Reference
-
1. Marcos A, Ham JM, Fisher RA, Olzinski AT, Posner MP. Surgical management of anatomical variations of the right lobe in living donor liver transplantation. Ann Surg. 2000; 231:824–831.2. Gadzijev EM. Surgical anatomy of hepatoduodenal ligament and hepatic hilus. J Hepatobiliary Pancreat Surg. 2002; 9:531–533.3. Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, et al. Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg. 2004; 239:82–86.4. Lee KK, Lee SK, Moon IS, Kim DG, Lee MD. Surgical techniques according to anatomic variations in living donor liver transplantation using the right lobe. Transplant Proc. 2008; 40:2517–2520.5. Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation. 2003; 75:3 Suppl. S28–S32.6. Varotti G, Gondolesi GE, Goldman J, Wayne M, Florman SS, Schwartz ME, et al. Anatomic variations in right liver living donors. J Am Coll Surg. 2004; 198:577–582.7. Nakamura T, Tanaka K, Kiuchi T, Kasahara M, Oike F, Ueda M, et al. Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation. 2002; 73:1896–1903.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Portal flow augmentation using meso-reno-portal anastomosis during liver transplantation with severe portal vein thrombosis
- Portal bifurcation reconstruction using own hepatic vein grafts due to portal vein anomaly of the living donor for the patient with portal vein thrombosis
- Renoportal Anastomosis in Living Donor Liver Transplantation; An Effective Technique for Patient with Diffuse Portal Vein Thrombosis and Large Splenorenal Shunts
- Living-donor liver transplantation for Abernethy malformation - case report and review of literature