Ann Surg Treat Res.
2015 May;88(5):289-293. 10.4174/astr.2015.88.5.289.
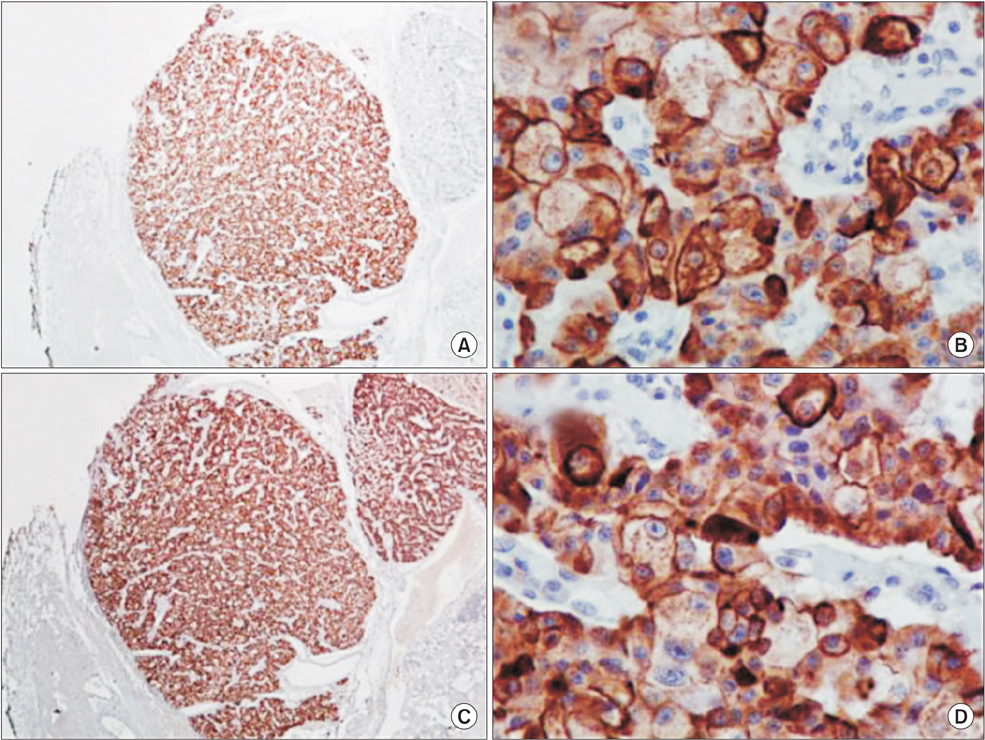
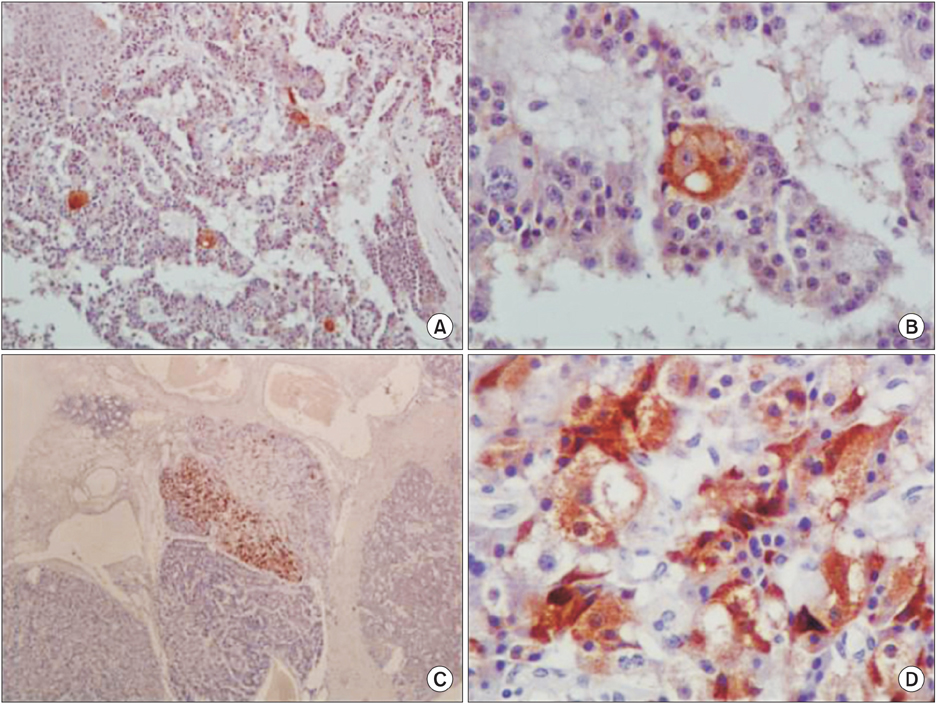
Giant malignant insulinoma
- Affiliations
-
- 1Department of Surgery, University Hospital of Patras, Rion, Greece. dimitriskaravias@gmail.com
- 2Division of Endocrinology and Diabetes, Department of Internal Medicine, University Hospital of Patras, Rion, Greece.
- 3Department of Radiology, University Hospital of Patras, Rion, Greece.
- 4Department of Pathology, University Hospital of Patras, Rion, Greece.
- KMID: 2166998
- DOI: http://doi.org/10.4174/astr.2015.88.5.289
Abstract
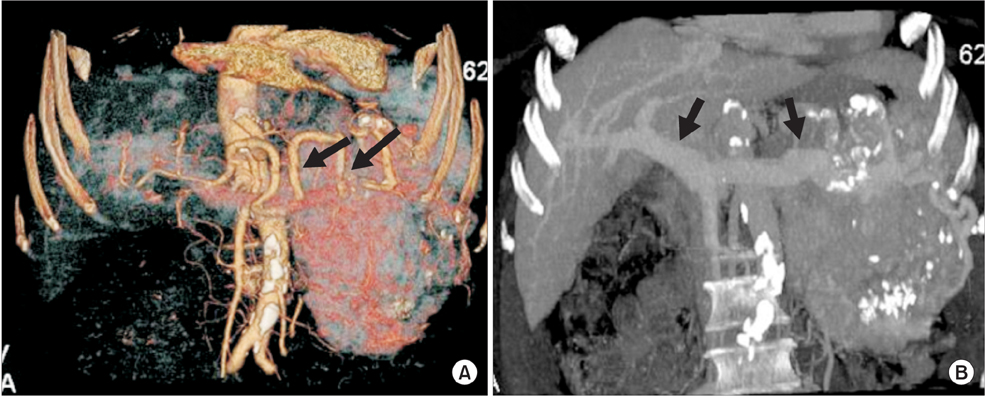
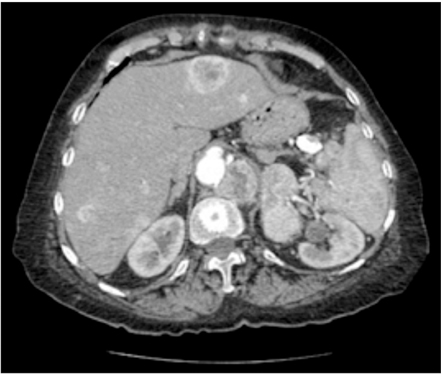
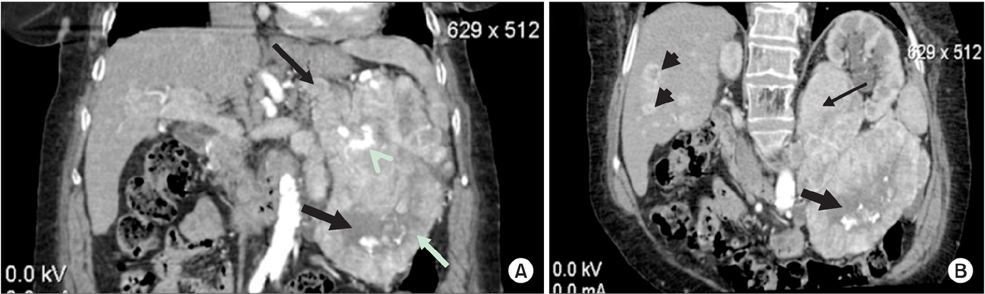
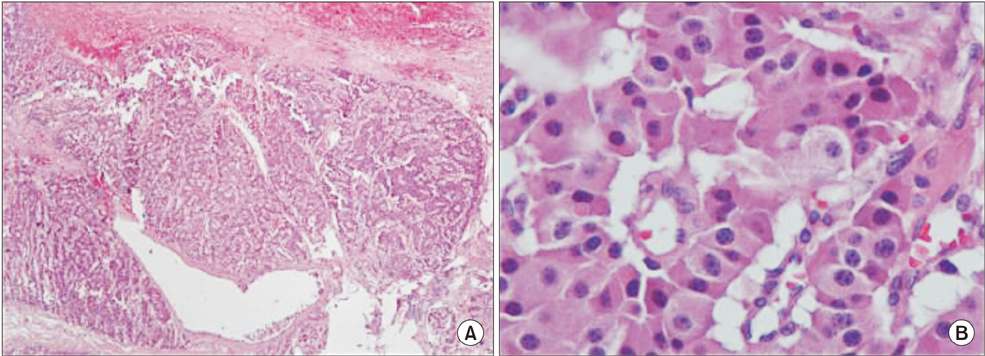
- Insulinomas are the most common pancreatic neuroendocrine tumors. Most insulinomas are benign, small, intrapancreatic solid tumors and only large tumors have a tendency for malignancy. Most patients present with symptoms of hypoglycemia that are relieved with the administration of glucose. We herein present the case of a 75-year-old woman who presented with an acute hypoglycemic episode. Subsequent laboratory and radiological studies established the diagnosis of a 17-cm malignant insulinoma, with local invasion to the left kidney, lymph node metastasis, and hepatic metastases. Patient symptoms, diagnostic and imaging work-up and surgical management of both the primary and the metastatic disease are reviewed.
Keyword
MeSH Terms
Figure
Reference
-
1. Service FJ, McMahon MM, O'Brien PC, Ballard DJ. Functioning insulinoma--incidence, recurrence, and long-term survival of patients: a 60-year study. Mayo Clin Proc. 1991; 66:711–719.2. Kulke MH, Anthony LB, Bushnell DL, de Herder WW, Goldsmith SJ, Klimstra DS, et al. Tumor Society (NANETS). NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010; 39:735–752.3. Mansour JC, Chen H. Pancreatic endocrine tumors. J Surg Res. 2004; 120:139–161.4. Whipple AO, Frantz VK. Adenoma of islet cells with hyperinsulinism: a review. Ann Surg. 1935; 101:1299–1335.5. Vinik AI, Woltering EA, Warner RR, Caplin M, O'Dorisio TM, Wiseman GA, et al. NANETS consensus guidelines for the diagnosis of neuroendocrine tumor. Pancreas. 2010; 39:713–734.6. Alexakis N, Neoptolemos JP. Pancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol. 2008; 22:183–205.7. Balon HR, Goldsmith SJ, Siegel BA, Silberstein EB, Krenning EP, Lang O, et al. Procedure guideline for somatostatin receptor scintigraphy with (111)In-pentetreotide. J Nucl Med. 2001; 42:1134–1138.8. Tucker ON, Crotty PL, Conlon KC. The management of insulinoma. Br J Surg. 2006; 93:264–275.9. Oberg K. Pancreatic endocrine tumors. Semin Oncol. 2010; 37:594–618.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Malignant Insulinoma Resistant to Octreotide and Combination Chemotherapy
- Successful Endoscopic Ultrasound-Guided Alcohol Ablation of Sporadic Insulinoma Using Three-Dimensional Targeting (with Video)
- Clinical Significance of Hyperinsulinsism - Diagnosis of Insulinoma
- A Case of Insulinoma without Peripheral Hyperinsulinemia
- Malignant Giant Cell Tumor of the Skull