Ann Surg Treat Res.
2015 May;88(5):269-275. 10.4174/astr.2015.88.5.269.
Learning curves for single incision and conventional laparoscopic right hemicolectomy: a multidimensional analysis
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. Seonghyeon.Yun@gmail.com
- 2Department of Surgery, Columbia Hospital, Kuala Lumpur, Malaysia, Korea.
- 3Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2166995
- DOI: http://doi.org/10.4174/astr.2015.88.5.269
Abstract
- PURPOSE
This study aimed to compare the learning curves and early postoperative outcomes for conventional laparoscopic (CL) and single incision laparoscopic (SIL) right hemicolectomy (RHC).
METHODS
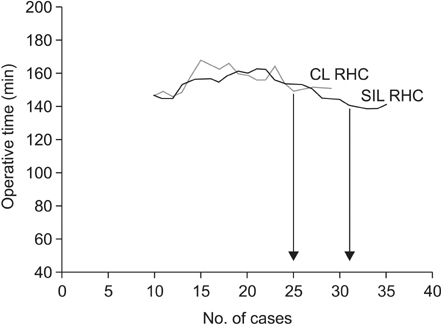
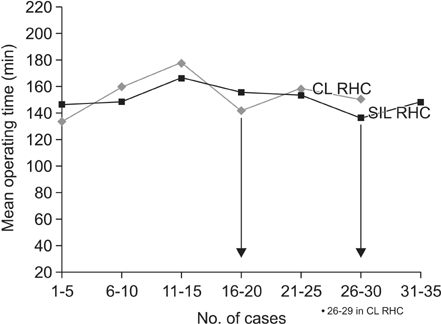
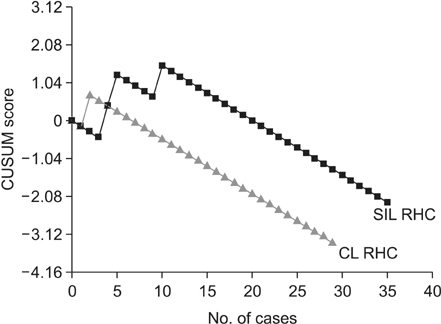
This retrospective study included the initial 35 cases in each group. Learning curves were evaluated by the moving average of operative time, mean operative time of every five consecutive cases, and cumulative sum (CUSUM) analysis. The learning phase was considered overcome when the moving average of operative times reached a plateau, and when the mean operative time of every five consecutive cases reached a low point and subsequently did not vary by more than 30 minutes.
RESULTS
Six patients with missing data in the CL RHC group were excluded from the analyses. According to the mean operative time of every five consecutive cases, learning phase of SIL and CL RHC was completed between 26 and 30 cases, and 16 and 20 cases, respectively. Moving average analysis revealed that approximately 31 (SIL) and 25 (CL) cases were needed to complete the learning phase, respectively. CUSUM analysis demonstrated that 10 (SIL) and two (CL) cases were required to reach a steady state of complication-free performance, respectively. Postoperative complications rate was higher in SIL than in CL group, but the difference was not statistically significant (17.1% vs. 3.4%).
CONCLUSION
The learning phase of SIL RHC is longer than that of CL RHC. Early oncological outcomes of both techniques were comparable. However, SIL RHC had a statistically insignificant higher complication rate than CL RHC during the learning phase.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Colonoscopy learning curves for colorectal surgery fellow trainees: experiences with the 15-year colonoscopy training program
Jung Ryul Oh, Kyung Su Han, Chang Won Hong, Byung Chang Kim, Bun Kim, Sung Chan Park, Min Jung Kim, Sang Jae Lee, Jae Hwan Oh, Changha Shin, Dae Kyung Sohn
Ann Surg Treat Res. 2018;95(4):169-174. doi: 10.4174/astr.2018.95.4.169.Learning curve for single-port robot-assisted rectal cancer surgery
Moon Suk Choi, Seong Hyeon Yun, Chang Kyu Oh, Jung Kyong Shin, Yoon Ah Park, Jung Wook Huh, Yong Beom Cho, Hee Cheol Kim, Woo Yong Lee
Ann Surg Treat Res. 2022;102(3):159-166. doi: 10.4174/astr.2022.102.3.159.
Reference
-
1. Li JC, Hon SS, Ng SS, Lee JF, Yiu RY, Leung KL. The learning curve for laparoscopic colectomy: experience of a surgical fellow in an university colorectal unit. Surg Endosc. 2009; 23:1603–1608.2. Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC. Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum. 2001; 44:217–222.3. Dinçler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P. Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum. 2003; 46:1371–1378.4. Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005; 242:83–91.5. Choi DH, Jeong WK, Lim SW, Chung TS, Park JI, Lim SB, et al. Learning curves for laparoscopic sigmoidectomy used to manage curable sigmoid colon cancer: single-institute, three-surgeon experience. Surg Endosc. 2009; 23:622–628.6. Simons AJ, Anthone GJ, Ortega AE, Franklin M, Fleshman J, Geis WP, et al. Laparoscopic-assisted colectomy learning curve. Dis Colon Rectum. 1995; 38:600–603.7. Bolsin S, Colson M. The use of the Cusum technique in the assessment of trainee competence in new procedures. Int J Qual Health Care. 2000; 12:433–438.8. Curet MJ, Putrakul K, Pitcher DE, Josloff RK, Zucker KA. Laparoscopically assisted colon resection for colon carcinoma: perioperative results and long-term outcome. Surg Endosc. 2000; 14:1062–1066.9. Tjandra JJ, Chan MK. Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis. 2006; 8:375–388.10. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005; 365:1718–1726.11. Salowi MA, Choong YF, Goh PP, Ismail M, Lim TO. CUSUM: a dynamic tool for monitoring competency in cataract surgery performance. Br J Ophthalmol. 2010; 94:445–449.12. Rajput A, Romanus D, Weiser MR, ter Veer A, Niland J, Wilson J, et al. Meeting the 12 lymph node (LN) benchmark in colon cancer. J Surg Oncol. 2010; 102:3–9.13. Ng SS, Lee JF, Yiu RY, Li JC, Leung WW, Leung KL. Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg. 2008; 32:454–458.14. Tan WS, Chew MH, Ooi BS, Ng KH, Lim JF, Ho KS, et al. Laparoscopic versus open right hemicolectomy: a comparison of short-term outcomes. Int J Colorectal Dis. 2009; 24:1333–1339.15. Leblanc F, Champagne BJ, Augestad KM, Stein SL, Marderstein E, Reynolds HL, et al. Single incision laparoscopic colectomy: technical aspects, feasibility, and expected benefits. Diagn Ther Endosc. 2010; 2010:913216.16. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484.17. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059.18. Yang C, Wexner SD, Safar B, Jobanputra S, Jin H, Li VK, et al. Conversion in laparoscopic surgery: does intraoperative complication influence outcome. Surg Endosc. 2009; 23:2454–2458.19. Boni L, Dionigi G, Cassinotti E, Di Giuseppe M, Diurni M, Rausei S, et al. Single incision laparoscopic right colectomy. Surg Endosc. 2010; 24:3233–3236.20. Hayashi M, Asakuma M, Komeda K, Miyamoto Y, Hirokawa F, Tanigawa N. Effectiveness of a surgical glove port for single port surgery. World J Surg. 2010; 34:2487–2489.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic single-incision right hemicolectomy with extended lymphadenectomy using the da Vinci SP Surgical Platform
- Initial Clinical Experience of Pure Single-Incision Robotic Right Hemicolectomy with da Vinci SP Platform
- Solo Single-Incision Laparoscopic Appendectomy versus Conventional Single-Incision Laparoscopic Appendectomy
- Laparoscopic extended right hemicolectomy with superiorto-inferior dissection: a mentee’s initial experience
- Single incision laparoscopic colectomy for colorectal cancer: comparison with conventional laparoscopic colectomy