Cancer Res Treat.
2004 Aug;36(4):222-227.
Radical Radiotherapy for Locally Advanced Cancer of Uterine Cervix
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. happylark@hanmir.com
- 2Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Obstetrics and Gynecology, Samsung Cheil Hospital and Women's Healthcare Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
- PURPOSE
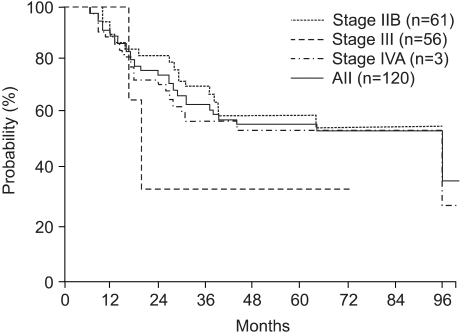
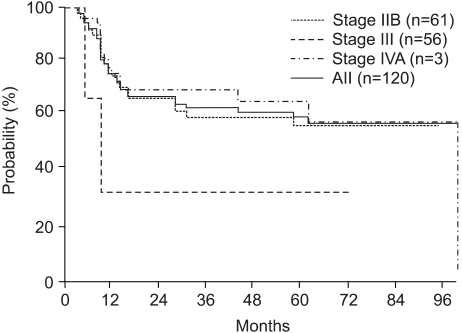
This study was performed to evaluate the treatment results, prognostic factors and complication rates in patients with locally advanced cancer of uterine cervix after radiotherapy with high-dose rate (HDR) brachytherapy. MATERIALS AND METHODS: One hundred and twenty patients with a locally advanced (stages IIB~IVA according to FIGO classification) carcinoma of the uterine cervix were treated with radiotherapy at the Department of Radiation Oncology, Samsung Medical Center between September 1994 and December 2001. The median age of the patients was 61 years (range 29 to 81). Sixty-one, 56 and 3 patients had FIGO stage IIB, III, and IV diseases, respectively. All patients were given external beam radiotherapy over the whole pelvis (median 50.4 Gy) and HDR intracavitary brachytherapy, with a median of 4 Gy per fraction, to point A. Twenty-one patients received chemotherapy, of which 13 and 21 received neoadjuvant chemotherapy and concurrent chemotherapy, respectively, during the first and fourth weeks of external beam radiotherapy. The chemotherapy was not randomly assigned and the median follow-up time was 28.5 months (range: 6~100 months). RESULTS: The three- and 5-year overall survival (OS) and disease-free survival (DFS) rates were 64.4 and 57.0%, and 63.7 and 60.2%, respectively. The 5-year OS and DFS rates of the patients at stages IIB, III and IV were 602, 57.9 and 33.3%, and 57.4, 65.4 and 33.3%, respectively. Univariate analysis indicated that the FIGO stage, overall treatment time (OTT) and treatment response were significant variables for the OS (p=0.035, p=0.0649 and p=0.0009) and of the DFS (p=0.0009, p=0.0359 and p=0.0363). Multivariate analysis showed that the treatment response was the only significant variable for the OS (p=0.0018) and OTT for the DFS (p=0.0360). The overall incidence of late complications in the rectum and bladder were 11.7 and 6.7%, respectively. In addition, insufficiency fractures were observed in 7 patients (5.8%). CONCLUSION: The results of this study suggest that radical radiotherapy with HDR brachytherapy was appropriate for the treatment of locally advanced uterine cervix cancer. Also, the response after treatment and OTT are significant prognostic factors.
MeSH Terms
Figure
Reference
-
1. Shin HR, Won YJ, Jung KW, Park JG. 2001 Annual Report of the Korea Central Cancer Registry: Based on Registered Data from 134 Hospitals. Cancer Res Treat. 2004; 36:19–30.
Article2. Coia L, Won M, Lanciano R, Marcial VA, Martz K, Hanks G. The patterns of care outcome study for cancer of the uterine cervix. Results of the second national practice survey. Cancer. 1990; 66:2451–2456. PMID: 2249184.
Article3. Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000; 48:201–211. PMID: 10924990.
Article4. Huh SJ. Current status of high dose rate brachytherapy in cervical cancer in Korea and optimal treatment schedule. J Korean Soc Ther Radiol Oncol. 1998; 16:357–366.5. Huh SJ, Kim BK, Lim DH, Shin SS, Lee JE, Kang MK, Ahn YC. Treatment results of radical radiotherapy in uterine cervix cancer. J Korean Soc Ther Radiol Oncol. 2002; 20:237–245.6. Huh SJ, Lim DH, Ahn YC, Kim DY, Kim MK, Wu HG, Choi DR. Effect of customized small bowel displacement system in pelvic irradiation. Int J Radiat Oncol Biol Phys. 1998; 40:623–727. PMID: 9486612.
Article7. International Commission on Radiation Units and Measurements. Report 38, Dose and Volume Specifications for Reporting Intracavitary Therapy in Gynecology. 1985. Bethesda MD: International Commission in Radiation Units and Measurements.8. Chassagne D, Sismondi P, Horiot JC, Sinistrero G, Bey P, Zola P, Pernot M, Gerbaulet A, Kunkler I, Michel G. A glossary for reporting complications of treatment in gynecological cancers. Radiother Oncol. 1993; 26:195–202. PMID: 8316648.
Article9. Kim OB, Choi TJ, Kim JH, Lee HJ, Kim YA, Suh YW, Lee TS, Cha SD. Carcinoma of uterine cervix treated with high dose rate intracavitary irradiation: pattern of failure. J Korean Soc Ther Radiol Oncol. 1993; 11:369–376.10. Perez CA, Breaux S, Madoc-Jones H, Bedwinek JM, Camel HM, Purdy JA, Walz BJ. Radiation therapy alone in the treatment of carcinoma of uterine cervix. I. Analysis of tumor recurrence. Cancer. 1983; 51:1393–1402. PMID: 6402291.
Article11. Lee SW, Suh CO, Chung EJ, Kim GE. Dose optimization of fractionated external radiation and high-dose-rate intracavitary brachytherapy. Int J Radiat Oncol Biol Phys. 2002; 52:1338–1344. PMID: 11955747.12. Huh SJ. The result of curative radiotherapy for carcinoma of uterine cervix. J Korean Soc Ther Radiol Oncol. 1993; 11:143–149.13. Orton CG, Seyedasdr M, Somnay A. Comparison of high and low dose rate remote afterloading for cervix cancer and the importance of fractionation. Int J Radiat Oncol Biol Phys. 1991; 21:1425–1434. PMID: 1938550.
Article14. Eifel PJ. High dose rate brachytherapy for carcinoma of the cervix: High tech or high risk? Int J Radiat Oncol Biol Phys. 1996; 24:383. PMID: 1526879.15. Petereit DG, Sarkaria JN, Chappell R, Fowler JF, Hartmann TJ, Kinsella TJ, Stitt JA, Thomadsen BR, Buchler DA. The adverse effect of treatment prolongation in cervical carcinoma. Int J Radiat Oncol Biol Phys. 1995; 32:1301–1307. PMID: 7635769.
Article16. Delaloye JF, Coucke PA, Pampallona S, Peltecu G, De Grandi P. Radiation therapy duration influences overall survival in patients with cervical carcinoma. Int J Gynaecol Obstet. 1997; 57:295–303. PMID: 9215493.
Article17. Lanciano RM, Won M, Coia LR, Hanks GE. Pretreatment and treatment factors associated with improved outcome in squamous cell carcinoma of the uterine cervix: a final report of the 1973 and 1978 patterns of care studies. Int J Radiat Oncol Biol Phys. 1991; 20:667–676. PMID: 2004942.
Article18. Lehman M, Thomas G. Is concurrent chemotherapy and radiotherapy the new standard of care for locally advanced cervical cancer? Int J Gynecol Cancer. 2001; 11:87–99. PMID: 11328406.
Article19. National Cancer Institute. Concurrent chemoradiation for cervical cancer. 1999. 2. 22. Washington D.C:20. Pearcey R, Brundage M, Drouin P, Jeffrey J, Johnston D, Lukka H, MacLean G, Souhami L, Stuart G, Tu D. Phase III Trial Comparing Radical Radiotherapy With and Without Cisplatin Chemotherapy in Patients With Advanced Squamous Cell Cancer of the Cervix. J Clin Oncol. 2002; 20:966–972. PMID: 11844818.
Article21. Potter R, Knocke TH. The potential of 3-D conformal brachytherapy and external beam radiotherapy in cervical cancer. Strahlenther Onkol. 2001; 177:641–642. PMID: 11789402.22. Heron DE, Gerszten K, Selvaraj RN, King GC, Sonnik D, Gallion H, Comerci J, Edwards RP, Wu A, Andrade RS, Kalnicki S. Conventional 3D conformal versus intensity-modulated radiotherapy for the adjuvant treatment of gynecologic malignancies: a comparative dosimetric study of dose-volume histograms small star, filled. Gynecol Oncol. 2003; 91:39–45. PMID: 14529660.23. Kang MK, Huh SJ, Han Y, Park W, Ju SG, Kim KJ, Lee JE, Park YJ, Nam HR, Kim DH, Ahn YC. Small bowel sparing effect of small bowel displacement system in 3D-CRT and IMRT for cervix cancer. J Korean Soc Ther Radiol Oncol. 2004; 22:130–147.24. Huh SJ, Park W, Ju SG, Lee JE, Han Y. Small-bowel displacement system for the sparing of small bowel in three-dimensional conformal radiotherapy for cervical cancer. Clin Oncol. 2004; (article in press).
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interferon-alpha2a, 13-cis-retinoic Acid and Radiotherapy for Locally Advanced Squamous Carcinoma of the uterine Cervix: Preliminary Study
- The ideal strategies of chemotherapy for the treatment of cervical cancer
- Rationale of Surgery in Locally Advanced and Oligometastatic Prostate Cancer
- Concurrent Chemoradiotherapy in Cervical Cancer (A New Paradigm in Cervical Cancer Treatment)
- Impact of histological subtype on survival in patients with locally advanced cervical cancer that were treated with definitive radiotherapy: adenocarcinoma/adenosquamous carcinoma versus squamous cell carcinoma