Clin Endosc.
2014 Sep;47(5):415-419. 10.5946/ce.2014.47.5.415.
Colonic Stent-Related Complications and Their Management
- Affiliations
-
- 1Department of Gastroenterology, Dong-A Medical Center, Dong-A University College of Medicine, Busan, Korea. jh2002@dau.ac.kr
- KMID: 2165372
- DOI: http://doi.org/10.5946/ce.2014.47.5.415
Abstract
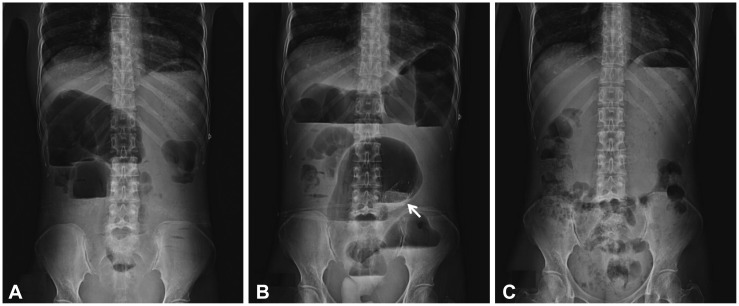
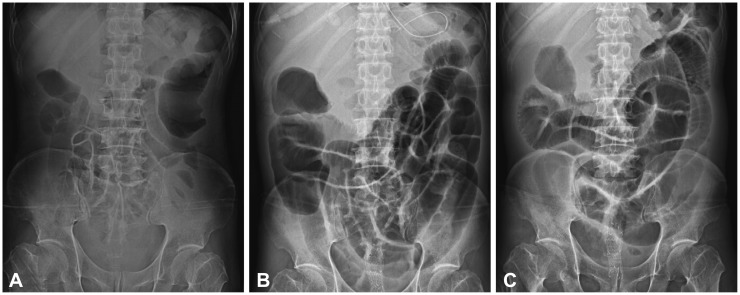
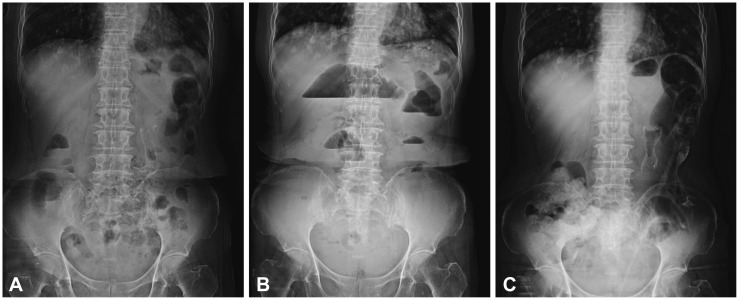
- Since its introduction in the early 1990s, the self-expandable metal stent (SEMS) has been increasingly used for the management of malignant colorectal obstruction, not only as a palliative method but also as a preoperative treatment in surgical candidates. However, more recently, concerns have been raised over stent complication rates. Early complications include pain, perforation, and rectal bleeding, and late complications include stent migration and stent obstruction. With the increasing use of SEMS for treatment, physicians need to be more aware of complications occurring after the placement of these stents. This review covers the technical considerations and management of complications after colonic stenting.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Colon stenting as a bridge to surgery in obstructive colorectal cancer management
Dong Hyun Kim, Han Hee Lee
Clin Endosc. 2024;57(4):424-433. doi: 10.5946/ce.2023.138.Development of colonic stent simulator using three-dimensional printing technique: a simulator development study in Korea
Hyundam Gu, Suyoung Lee, Sol Kim, Hye-Lim Jang, Da-Woon Choi, Kyu Seok Kim, Yu Ri Shin, Dae Young Cheung, Bo-In Lee, Jin Il Kim, Han Hee Lee
Clin Endosc. 2024;57(6):790-797. doi: 10.5946/ce.2024.110.
Reference
-
2. Trompetas V. Emergency management of malignant acute left-sided colonic obstruction. Ann R Coll Surg Engl. 2008; 90:181–186. PMID: 18430330.
Article3. Helfer KS. Auditory and auditory-visual perception of clear and conversational speech. J Speech Lang Hear Res. 1997; 40:432–443. PMID: 9130211.
Article4. Small AJ, Coelho-Prabhu N, Baron TH. Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc. 2010; 71:560–572. PMID: 20189515.5. Athreya S, Moss J, Urquhart G, Edwards R, Downie A, Poon FW. Colorectal stenting for colonic obstruction: the indications, complications, effectiveness and outcome: 5 year review. Eur J Radiol. 2006; 60:91–94. PMID: 16806783.6. Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007; 94:1151–1154. PMID: 17541987.
Article7. Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012; 26:110–119. PMID: 21789642.
Article8. Choi JH, Lee YJ, Kim ES, et al. Covered self-expandable metal stents are more associated with complications in the management of malignant colorectal obstruction. Surg Endosc. 2013; 27:3220–3227. PMID: 23494513.
Article9. Binkert CA, Ledermann H, Jost R, Saurenmann P, Decurtins M, Zollikofer CL. Acute colonic obstruction: clinical aspects and cost-effectiveness of preoperative and palliative treatment with self-expanding metallic stents: a preliminary report. Radiology. 1998; 206:199–204. PMID: 9423673.10. Abbott S, Eglinton TW, Ma Y, Stevenson C, Robertson GM, Frizelle FA. Predictors of outcome in palliative colonic stent placement for malignant obstruction. Br J Surg. 2014; 101:121–126. PMID: 24301218.
Article11. Jung MK, Park SY, Jeon SW, et al. Factors associated with the long-term outcome of a self-expandable colon stent used for palliation of malignant colorectal obstruction. Surg Endosc. 2010; 24:525–530. PMID: 19597776.12. Arenas RB, Fichera A, Mhoon D, Michelassi F. Incidence and therapeutic implications of synchronous colonic pathology in colorectal adenocarcinoma. Surgery. 1997; 122:706–709. PMID: 9347846.13. Miyayama S, Matsui O, Kifune K, et al. Malignant colonic obstruction due to extrinsic tumor: palliative treatment with a self-expanding nitinol stent. AJR Am J Roentgenol. 2000; 175:1631–1637. PMID: 11090392.14. Keswani RN, Azar RR, Edmundowicz SA, et al. Stenting for malignant colonic obstruction: a comparison of efficacy and complications in colonic versus extracolonic malignancy. Gastrointest Endosc. 2009; 69(3 Pt 2):675–680. PMID: 19251009.
Article15. Khot UP, Lang AW, Murali K, Parker MC. Systematic review of the efficacy and safety of colorectal stents. Br J Surg. 2002; 89:1096–1102. PMID: 12190673.
Article16. Tekkis PP, Kinsman R, Thompson MR, Stamatakis JD. Association of Coloproctology of Great Britain, Ireland. The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. Ann Surg. 2004; 240:76–81. PMID: 15213621.
Article17. Leitman IM, Sullivan JD, Brams D, DeCosse JJ. Multivariate analysis of morbidity and mortality from the initial surgical management of obstructing carcinoma of the colon. Surg Gynecol Obstet. 1992; 174:513–518. PMID: 1595029.18. Dharmadhikari R, Nice C. Complications of colonic stenting: a pictorial review. Abdom Imaging. 2008; 33:278–284. PMID: 17505852.
Article19. Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004; 99:2051–2057. PMID: 15447772.
Article20. Mainar A, Tejero E, Maynar M, Ferral H, Castañeda-Zúñiga W. Colorectal obstruction: treatment with metallic stents. Radiology. 1996; 198:761–764. PMID: 8628867.
Article21. Canon CL, Baron TH, Morgan DE, Dean PA, Koehler RE. Treatment of colonic obstruction with expandable metal stents: radiologic features. AJR Am J Roentgenol. 1997; 168:199–205. PMID: 8976946.
Article22. Lopera JE, Ferral H, Wholey M, Maynar M, Castañeda-Zúñiga WR. Treatment of colonic obstructions with metallic stents: indications, technique, and complications. AJR Am J Roentgenol. 1997; 169:1285–1290. PMID: 9353443.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Malignant Colonic Obstruction
- Enteral stents: Complications and their management
- A Case of Sigmoidorectal Intussusception after Self-Expandable Colonic Stent Placement
- Colon stenting as a bridge to surgery in obstructive colorectal cancer management
- Fluoroscopic Management of Complications after Colorectal Stent Placement